This article has been
cited by other articles in ScienceCentral.
TO THE EDITOR: Currently, the most common blood test in hospitals, complete blood count (CBC), is typically performed by automated hematology analyzers. However, pseudothrombocytopenia caused by pseudo gray platelet syndrome (PGPS) might cause errors in CBC test results. Here we report what we believe to be the first reported case of PGPS in Korea.
CASE
The patient was a 46 year-old woman who came to our hospital for a general health checkup. She had no history of bleeding tendency, and neither did any of her three sisters. She had one son and one daughter who were fraternal twins; also without history of bleeding tendency. Her blood was collected into ethylenediaminetetraacetic acid dipotassium salt dehydrate (EDTA-2K, 3.3 mmol/L) and the CBC was measured using a Sysmex XE-2100 (Sysmex, Kobe, Japan). During the general health checkup, CBC had been studied with the blood collected in the EDTA tube. The CBC results included a platelet count of 63×10
9/L, white blood cell (WBC) count of 3.31×10
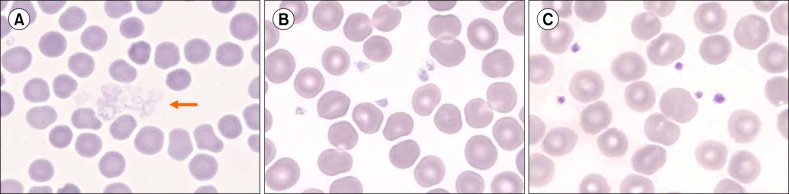
9/L, and hemoglobin level of 13.0 g/dL. The mean platelet volume (MPV) and platelet distribution width (PDW) were 'unmeasurable'. Based on these findings, we made a peripheral blood film. The blood film showed gray agranular platelets with aggregation (
Fig. 1A).
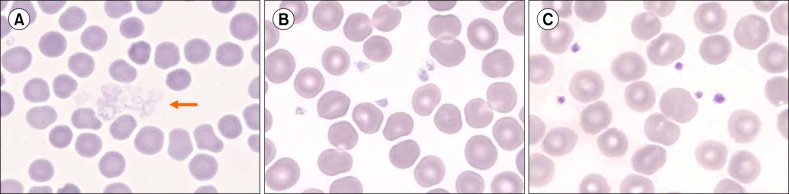 | Fig. 1Pseudo gray platelets. (A) Blood collected in EDTA 4 hours prior showing aggregated agranular gray platelets (arrow). (B) Blood collected into EDTA showing large and pale agranular platelets. (C) Blood collected into sodium citrate showing normally stained platelets with tiny purple granules. Blood films were prepared immediately after venipuncture (×1,000, Wright-Giemsa stain).
|
The patient returned after six days for a follow-up CBC. This time, the blood was collected into both EDTA and sodium citrate tubes. The platelet count of blood in sodium citrate was 261×10
9/L, with a WBC count of 4.72×10
9/L and hemoglobin level of 12.0 g/dL. The MPV was 11.4 fL (normal range, 7.9-11.8) and PDW was 13.5 fL (normal range, 9.1-19.4). Blood films were prepared immediately after venipuncture from both EDTA and citrate tubes. The EDTA blood showed poorly stained agranular gray platelets (
Fig. 1B) while the blood in sodium citrate showed normal platelets with purple-stained granules (
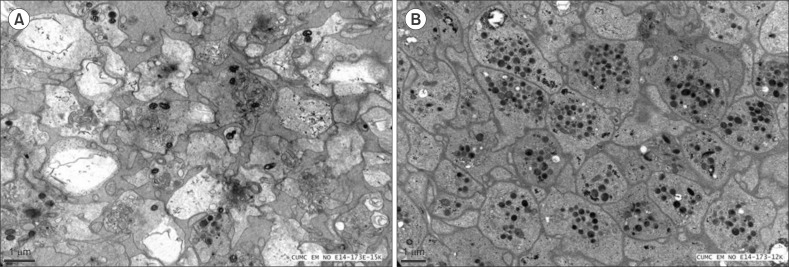
Fig. 1C). We also used electron microscopy (EM) to examine the platelets, using a transmission electron microscope (Jeol, JEM-1010, Tokyo, Japan) to examine cellular structure. Platelet-rich plasma (PRP) was separated by centrifugation at 100×g for 10 minutes at room temperature. Before EM, PRP samples were fixed, dehydrated in 35% ethanol for 15 minutes, and then embedded, sectioned into ultra-thin slices (70 nm), and stained in uranyl acetate for 2 hours. Platelet activation was apparent and only a few storage granules were found in EDTA blood (
Fig. 2A). However, no platelet activation was present in sodium citrate and many α-granules were visible in the cytoplasm (
Fig. 2B).
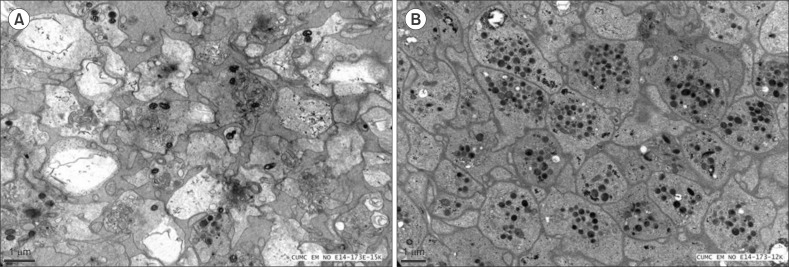 | Fig. 2Electron micrographs of pseudo gray platelets. (A) Blood collected into EDTA showing absence of storage granules (×15,000). (B) Blood collected into the trisodium citrate dehydrate-containing tube showing normal platelet structures, including typical α-granules (×12,000).
|
Go to :

DISCUSSION
We report a case of PGPS. The patient had pseudothrombocytopenia and agranular platelet morphology similar to gray platelet syndrome (GPS). Unlike GPS, however, this finding was noted only when the blood was collected into the EDTA-containing tube, and not when the blood was collected into the sodium citrate-containing tube, which showed normal platelet counts. Only a few cases of PGPS have been reported [
1234]. To our knowledge, this is the first case to be reported in Korea. Stavem and Berg [
1] described EDTA-induced 'platelet stain preventing factor', and Mant et al. [
2], Cockbill et al. [
3], and Toyota et al. [
4] reported platelet degranulation caused by EDTA.
Unlike GPS, which is a rare inherited disorder of the megakaryocytes characterized by loss of the α-granule storage pool of proteins in platelets and causing bleeding tendency [
5], PGPS is an
in vitro phenomenon showing EDTA-induced pseudothrombocytopenia with no bleeding tendency. The typical EM finding of PGPS is degranulation of EDTA-exposed platelets.
Mant et al. [
2] reported cases of EDTA-induced platelet degranulation with aggregation caused by a 'plasma factor' which was not IgG, IgM, fibrinogen or albumin. They thought it was an unidentified abnormal plasma component which, on exposure to EDTA, develops 'anti-platelet activity'. Cockbill et al. [
3] reported that the 'plasma factor' causing platelet degranulation could be an immunoglobulin but clearly different from the EDTA-sensitive antibodies which cause platelet aggregation and agglutination. The mechanism by which platelet degranulation occurs in PGPS remains unclear.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download