A 53-year-old male patient presented to the surgery OPD with history of swelling of the left side of his neck for the last six months. The swelling had gradually increased to its present size over this time period and was not associated with pain, changes in his voice, or difficulty in breathing. A well-healed scar was present on the front of the patient's neck, as he had undergone surgery four years earlier for which no further details were available. The patient had not received any post-operative chemotherapy or radiotherapy. On examination, a soft, non-tender swelling measuring 8×10 cm was noted on the front of the neck toward the left side that moved with deglutition but not with protrusion of the tongue. The cervical lymph nodes were not enlarged. There were no signs of pressure effects on the trachea, larynx, esophagus, or major veins of the thorax, and no sign of hypothyroidism or hyperthyroidism.
All routine investigations, including complete blood count, liver function test and renal function test, were within normal limits. A thyroid profile showed slightly increased thyroid-stimulating hormone levels (TSH, 5.92 mIU/mL; normal range, 0.5-5.0 mIU/mL) and slightly decreased T
4 levels (3.65 µ/dL; normal range, 4.5-12.6 µ/dL). Contrast-enhanced computed tomography of the neck and chest showed a well-defined mass lesion of 6×6×10 cm in the region of the left lobe of the thyroid gland extending up to the hyoid bone. Inferiorly, the mass extended 2 cm above the level of the aortic arch. Ultrasonography of the abdomen showed fatty liver with an enlarged prostate, and no enlarged lymph nodes or hepato-splenomegaly were observed. Fine-needle aspiration cytology of the swollen area was performed, revealing a dispersed population of atypical plasma cells along with a few benign follicular epithelial cells that were infiltrated by lymphocytes. The possibility of plasmacytoma of the thyroid in a background of thyroiditis was suggested. Following a cytology report, an extensive workup for multiple myeloma (MM) was performed, which showed normal bone marrow, and radiographs of the skull, chest, spine, and pelvis did not show any abnormalities. Serum protein electrophoresis showed normal levels of serum proteins with a very low serum M protein level of 0.25 g/dL. Other values were as follows: serum total protein 6.90 g/dL, albumin 4.41 g/dL, alpha 1 globulin 0.35 g/dL, alpha 2 globulin 0.77 g/dL, and gamma globulin 0.82 g/dL with an A:G ratio of 1.77. The serum kappa-free light chain level was increased (24.07 mg/L; normal range, 3.30-19.40 mg/L), while the level of lambda free light chain and the kappa/lambda ratio were within normal limits (19.06 mg/L and 1.26, respectively). Serum β
2 microglobulin and calcium levels were within the normal ranges. The patient was prepared for surgery, and a total thyroidectomy was performed. Intra-operatively, there was a 10×8 cm swelling on the left lobe of the thyroid with a shift of the trachea to the right side without any infiltration of the adjacent structures or capsule, and there was no lymphadenopathy. Gross examination of the specimen showed a globular soft piece of tissue measuring 8.5×6×5 cm. The external surface was nodular with an adherent capsule and showed prominent blood vessels. The cut section of the specimen was gray, firm, and fleshy in appearance (
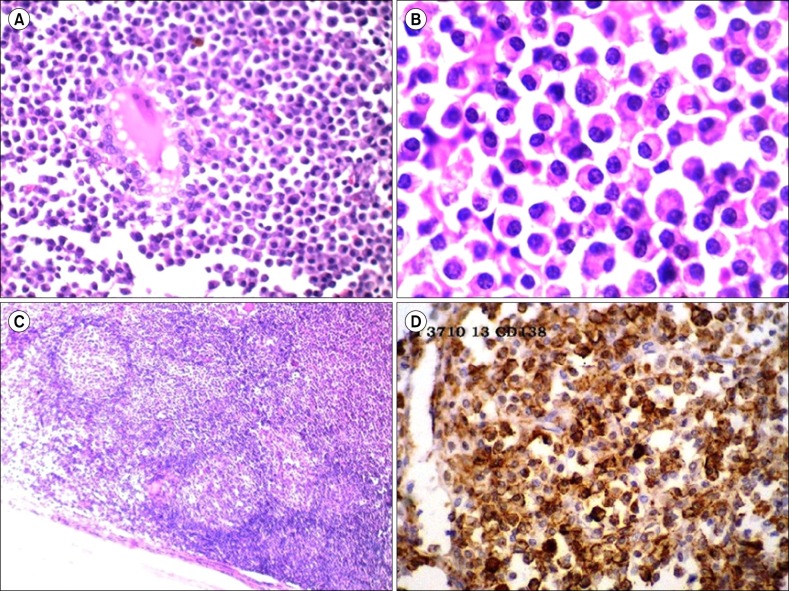
Fig. 1). Microscopically, multiple sections taken from the tumor showed sheets of plasma cells infiltrating the thyroid parenchyma with few entrapped atrophic thyroid follicles (
Fig. 2A). These cells have eccentric, round nuclei with abundant eosinophilic cytoplasm. Sporadic binucleated and multinucleated plasma cells were also observed (
Fig. 2B). Many lymphoid follicles with germinal centers were also present (
Fig. 2C). Thus, a diagnosis of EMP of the thyroid in a background of Hashimoto's thyroiditis was made. Immunohistochemistry (IHC) showed CD138-positive tumor cells while CD20 was negative, thus clinching the diagnosis of EMP (
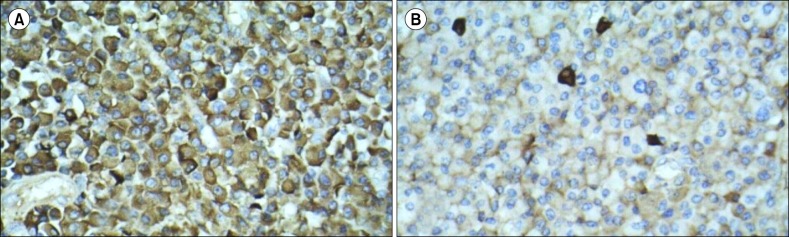
Fig. 2D). IHC for kappa light chain showed strong cytoplasmic positivity in the tumor cells while that of the lambda light chain was negative (
Fig. 3). The patient is undergoing regular follow-up and has been asymptomatic for the past eight months.
 | Fig. 1Extramedullary plasmacytoma: gross-cut section of a specimen appears gray, firm, and fleshy. 
|
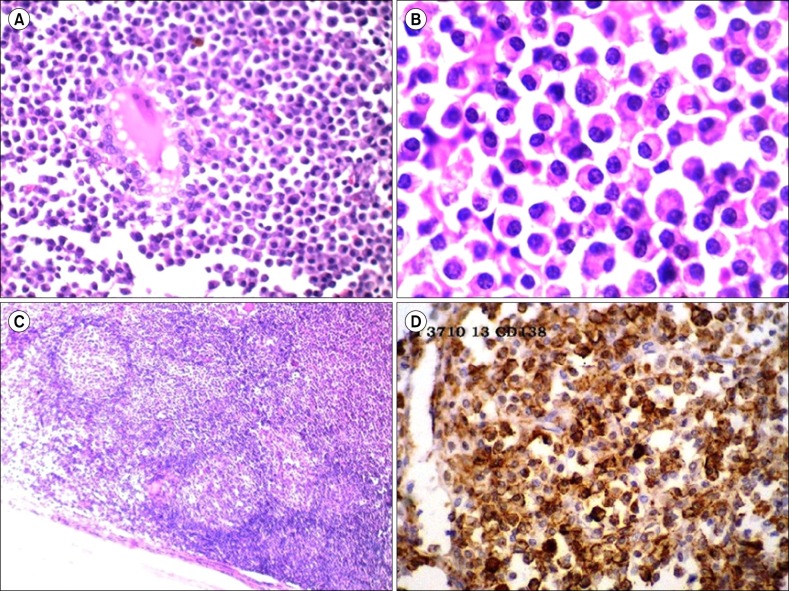 | Fig. 2Microscopy of extramedullary plasmacytoma of the thyroid. (A) Sheets of plasma cells infiltrating the thyroid parenchyma with few entrapped atrophic thyroid follicles (H&E, ×100). (B) Sheets of plasma cells with some binucleated forms (H&E, ×400). (C) Many lymphoid follicles with germinal centers (H&E, ×100). (D) CD138-positive tumor cells on immunohistochemistry. 
|
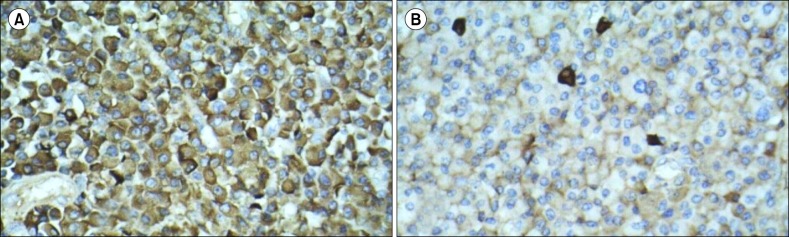 | Fig. 3Immunohistochemistry of extramedullary plasmacytoma of the thyroid showing (A) tumor cells positive for kappa light chain and (B) tumor cells negative for lambda light chain. 
|




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download