Abstract
Background
We aimed to investigate which factors in the clinical profile of mothers with idiopathic thrombocytopenic purpura (ITP) can predict neonatal risk of thrombocytopenia.
Methods
Data was retrospectively collected from all pregnant women with ITP who presented to our institution between 2001 and 2013. Neonatal offspring of these women were classified into 2 groups based on the presence or absence of neonatal thrombocytopenia (platelet count <100×109/L). Several parameters were compared between the 2 groups, including maternal age, maternal platelet count, maternal treatment history, and thrombocytopenia in siblings. We further examined the correlation between maternal platelet count at the time of delivery and neonatal platelet count at birth; we also examined the correlation between the minimum platelet counts of other children born to multiparous women.
Results
Sixty-six neonates from 49 mothers were enrolled in the study. Thrombocytopenia was observed in 13 (19.7%) neonates. Maternal treatment for ITP such as splenectomy did not correlate with a risk of neonatal thrombocytopenia. Sibling thrombocytopenia was more frequently observed in neonates with thrombocytopenia than in those without (7/13 vs. 4/53, P<0.01). No association was observed between maternal and neonatal platelet counts. However, the nadir neonatal platelet counts of first- and second-born siblings were highly correlated (r=0.87).
Go to : 
Idiopathic thrombocytopenic purpura (ITP) is an immunohematological disorder characterized by acquired thrombocytopenia with no clinically apparent associated condition or other clear cause of thrombocytopenia. ITP is thought to be caused by autoantibodies against nonpolymorphic platelet antigens, although antibodies cannot be detected in all women with ITP. A major problem associated with ITP in pregnancy is neonatal thrombocytopenia. Indeed, the pathogenic antiplatelet antibodies can cross the placenta and cause neonatal thrombocytopenia, which may increase the risk of cerebral hemorrhage in newborn infants [1, 2]. ITP is most prevalent in women of childbearing age; therefore, managing this disease is of great importance in clinical obstetrics. In this study, we investigated neonates with and without thrombocytopenia born to mothers with ITP and sought to identify factors that predict the risk of neonatal thrombocytopenia.
Go to : 
Data was retrospectively collected from all pregnant women with ITP who presented to our institution between 2001 and 2013. The Kyushu University Hospital Ethical Review Board approved the study (approval number 26-134). The following information was extracted from the medical chart of each eligible patient: maternal age, prior splenectomy, medication during pregnancy, platelet count during early pregnancy and at delivery, treatments received to raise platelet count immediately before delivery (immunoglobulin infusion or platelet transfusion), gestational age at delivery, neonatal birth weight, Apgar scores, cord artery pH, and neonatal cord blood platelet count after delivery. Information collected for each infant included platelet count throughout the early neonatal period, bleeding complications, and medical/procedural treatments.
Neonates were classified into 2 groups based on the presence or absence of thrombocytopenia (defined as a minimum platelet count during the neonatal period of less than 100×109/L). The 2 groups were compared for differences in maternal age, parity, maternal platelet count, maternal treatment history, gestational age at birth, birth weight, and thrombocytopenia among an infant's siblings. We further examined the correlation between maternal platelet count at the time of delivery and neonatal platelet count at birth as well as correlations between the minimum platelet counts of other children born to multiparous women. In the latter analysis, if a woman had more than 3 pregnancies, only data from the first 2 pregnancies were used.
Maternal ITP had been previously diagnosed by hematology specialists at the Kyushu University Hospital. ITP is a diagnosis of exclusion, and criteria for its diagnosis were as follows: isolated thrombocytopenia for which other causes were excluded, normal or hypermegakaryocyte production in the bone marrow, and normal white and red blood cell counts. In the absence of a definite diagnosis of ITP before pregnancy, significant thrombocytopenia in the first trimester with a declining platelet count as gestation progressed was considered consistent with ITP. Meanwhile, mild thrombocytopenia during the second or third trimester and not associated with hypertension or proteinuria was considered gestational thrombocytopenia; these patients were not included in the study. Detection of maternal serum antiplatelet antibodies or platelet-associated immunoglobulin G was not systematically performed because these data were not required for diagnosis confirmation. Patients were treated with standard ITP treatment regimens, including corticosteroids and intravenous immunoglobulins (IVIG). Splenectomy was performed on patients who were either refractory to steroids or who were steroid-dependent and on those patients who failed to respond to IVIG therapy.
Institutional management policies for pregnant women with ITP were followed. In the second or third trimester, patients with an indication for treatment were administered standard-dose steroids as first-line treatment. If the platelet count was less than 50×109/L later in pregnancy, aggressive treatment with IVIG (0.4 g/kg/d for 5 days) was performed to prepare the patient for labor and delivery. If the maternal platelet count did not increase more than 50×109/L despite aggressive treatment, platelet transfusion was performed to increase maternal platelet counts to levels sufficient for vaginal delivery or cesarean section. After delivery, platelet counts were obtained from the neonatal cord blood of each infant and serial platelet counts were obtained during the first postpartum week until either the platelet count increased spontaneously or a stable platelet level was observed. All platelet counts were measured using a Coulter counter on blood samples collected in EDTA vacutainers.
Data are reported as median (range), discrete variables, or categories. Univariate analysis of the neonates with thrombocytopenia versus neonates without thrombocytopenia was performed by chi-squared or Mann-Whitney tests for categorical and continuous outcomes, respectively. Correlations were analyzed using Spearman's correlation. A P value less than 0.05 was considered statistically significant. Statistical analysis was performed using Statistical Package for the Social Sciences, version 21.0, for Windows (SPSS, Chicago, IL, USA).
Go to : 
During the study period, 74 neonates were born to 56 mothers with ITP. Because of incomplete data collection, 8 neonates from 7 mothers were excluded from the study. In total, 66 neonates from 49 mothers were enrolled in the study.
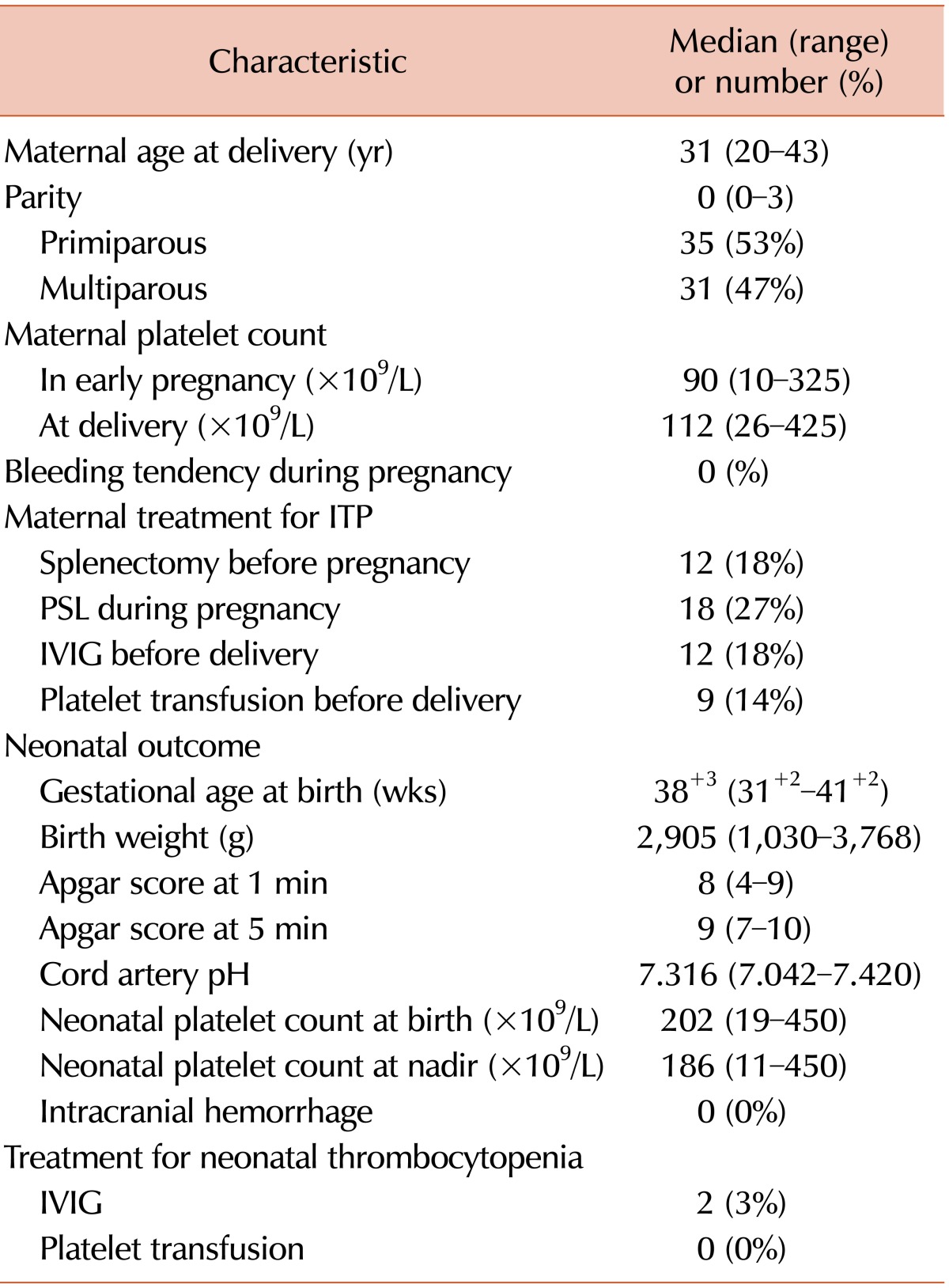
Table 1 shows the maternal profiles and neonatal outcomes of all 66 deliveries. The average gestational age at delivery was 38+3 weeks (31+2-41+2). Eleven patients who had previously undergone splenectomy delivered 12 infants. The median maternal platelet count was 90×109/L (range, 10-325×109/L) during early pregnancy and 112×109/L (range, 26-425×109/L) at delivery. Treatment with corticosteroids had been performed during pregnancy in 18 cases (27%). Before delivery, 12 pregnant women (18%) had received IVIG injections and 9 (14%) had received platelet transfusions (these agents were used to elevate platelet counts to prevent bleeding complications during the intrapartum period). As a result, bleeding amounts at the time of delivery were less than 1,000 mL in these mothers. In this series, no asphyxiated neonates (Apgar score at 5 min ≤6 or umbilical cord pH <7.0) were observed. The neonatal platelet count at birth was 19-450×109/L with a median platelet count of 202×109/L. Thrombocytopenia (platelet count <100×109/L) was diagnosed in 13 (19.7%) infants. No neonates required platelet transfusion and no neonate suffered from intracranial hemorrhage.
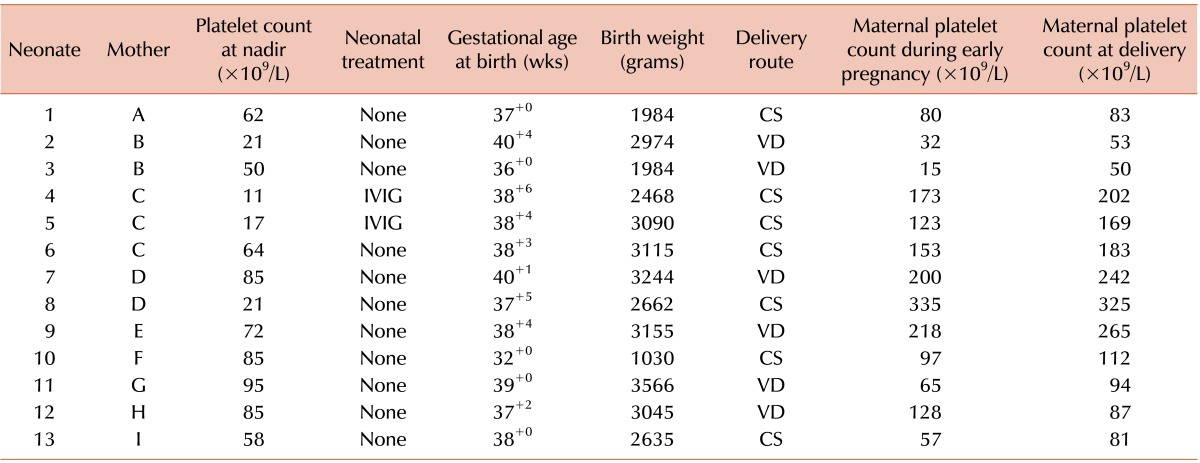
Table 2 shows the clinical profiles of neonates with thrombocytopenia (platelet count at nadir <100×109/L). Thirteen neonates born to 9 mothers were thrombocytopenic. Among these neonates, the maternal platelet count was less than 100×109/L in 6 mothers during early pregnancy and less than 100×109/L in 6 mothers at the time of delivery. Postnatal treatment of infants with severe thrombocytopenia consisted solely of IVIG administration (N=2).
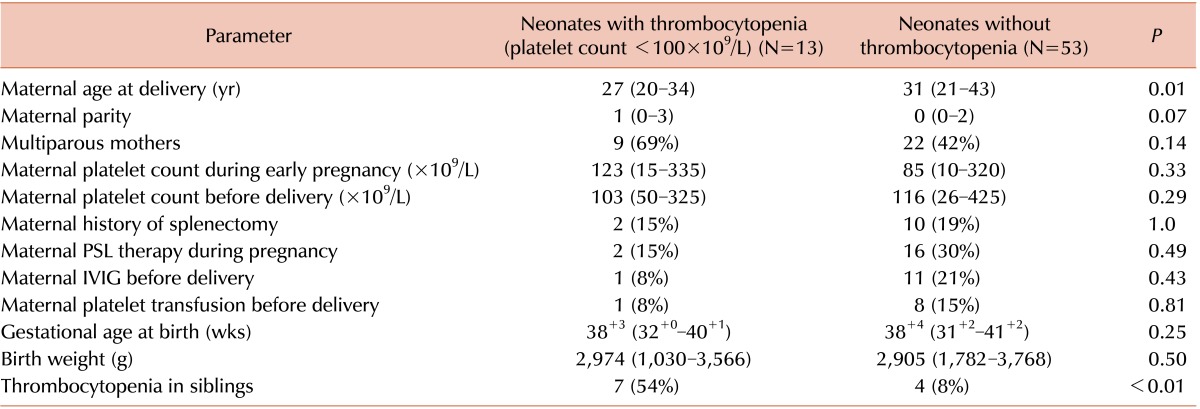
Table 3 shows the predictive value of maternal treatment history, maternal platelet count, and other parameters for predicting neonatal thrombocytopenia. Maternal treatments such as splenectomy, betamethasone use during pregnancy, IVIG administration, and platelet transfusion before delivery did not correlate with the risk of neonatal thrombocytopenia. Thrombocytopenia in siblings was more frequently observed in infants with neonatal thrombocytopenia than in those without (P <0.01).
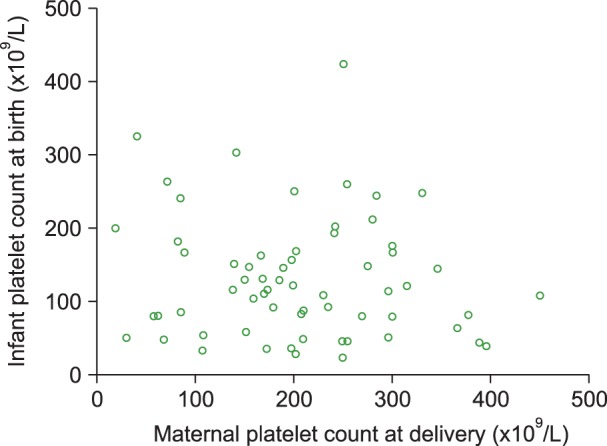
Fig. 1 shows the correlation between maternal platelet count at delivery (x axis) and neonatal platelet count at birth (y axis). No correlation was observed between these 2 parameters.
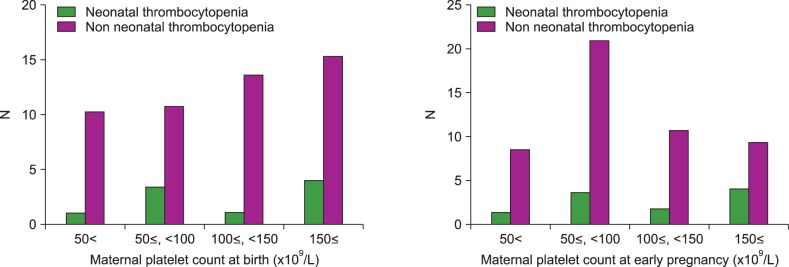
Fig. 2 shows the distribution of the maternal platelet count during early pregnancy and at delivery relative to neonatal thrombocytopenia (platelet count at nadir <100×109/L). Neonatal thrombocytopenia occurred at similar rates in each group and a definite tendency was not found.
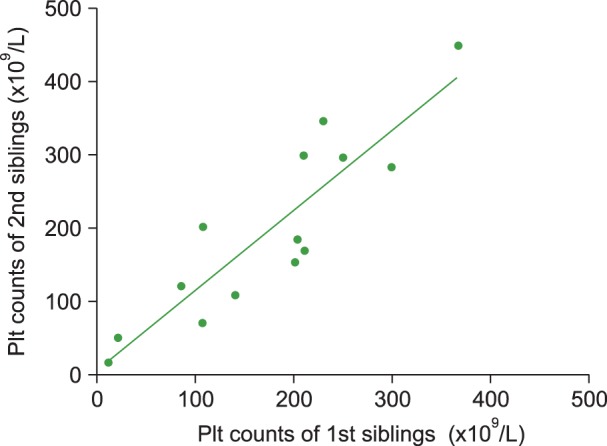
Among the 49 mothers included in the study, 14 were multiparous. Fig. 3 shows the correlation between the minimum platelet counts of the first and second children born to multiparous mothers. A strong positive correlation was observed between neonatal platelet counts among the first and second children, with a Spearman correlation coefficient of 0.87 (P <0.0001).
Go to : 
ITP is an autoimmune disorder caused by autoantibodies against several platelet membrane glycoproteins and results in platelet destruction within the reticular endothelial system. ITP predominantly affects young women of reproductive age; therefore, managing maternal ITP is of great importance in clinical obstetrics. Pregnancy can exacerbate ITP, and platelet counts have been shown to decrease throughout gestation in 50% of pregnancies [3]. Although it is well known that pregnant women with ITP can deliver neonates with severe thrombocytopenia, the exact cause of the neonatal thrombocytopenia is unknown. Circulating antiplatelet antibodies can cross the placenta and may cause a passive neonatal immune thrombocytopenia, but antiplatelet antibodies are not always detectable in maternal serum.
Severe thrombocytopenia in the newborn can cause hemorrhagic manifestations, the most dangerous of which is intracranial hemorrhage. In our cohort, thrombocytopenia was observed in 19.7% of neonates, which is similar to rates previously described [4, 5, 6, 7, 8]. Although its incidence is relatively low, intracranial bleeding is a serious thrombocytopenia complication in neonates born to mothers with ITP [4, 5, 9, 10]. Further, a prenatally diagnosed case of fetal intracranial hemorrhage secondary to maternal ITP has recently been reported [11]. Fetal and neonatal hemorrhagic complications remain the most pressing issues in the obstetric management of women with ITP. Our study reviewed 66 deliveries in 49 women with ITP. No bleeding complications occurred in any neonate, despite platelet counts at birth being less than 100×109/L in 13 infants and less than 50×109/L in 4 infants.
Recent studies have attempted to determine which factors may predict thrombocytopenia in infants born to mothers with ITP. Several studies have found a poor correlation between maternal and neonatal platelet counts [12, 13, 14, 15]. In agreement with these studies, we failed to find a definite correlation between these counts. Other investigators have found that maternal splenectomy before pregnancy is positively correlated with neonatal thrombocytopenia [2, 6, 13, 16, 17, 18], but we observed no such correlation. Hence, it may not be possible to predict neonatal thrombocytopenia based on maternal clinical profiles.
Given that many of the mothers in our study were multiparous, we compared platelet counts among first and second siblings. We found a strong positive correlation between neonatal thrombocytopenia among siblings. Thrombocytopenia in a sibling was more frequently observed in neonates with thrombocytopenia than in neonates without thrombocytopenia. Based on this result, we conclude that the presence of an older sibling with neonatal thrombocytopenia is a risk factor for neonatal thrombocytopenia in subsequent pregnancies. Previous studies have described similar findings [18, 19, 20]. The precise mechanisms underlying this phenomenon remain unclear. However, it is possible that the biological aggressiveness of the maternal antibodies and their avidity for platelets remain unchanged over time and over multiple pregnancies [20].
Our study has several limitations. The first is the retrospective study design. Our data collection was limited to information documented in the patient's medical chart and available in the laboratory database. For example, we were unable to include information on platelet-associated immunoglobulin G and serum antiplatelet antibody levels because these data were not collected for every patient. Furthermore, the postnatal platelet count was not followed for every neonate with a normal platelet count at birth. For these neonates, the nadir platelet count was assumed to be identical to the platelet count at birth. The study is also limited by sample size. Although our sample size was relatively large compared with other single-center studies, a larger number of study participants is required for reliable multivariable analysis. Finally, our hospital is a major referral center for pregnancies complicated by severe maternal diseases; this referral bias may have led to the inclusion of patients with particularly severe diseases.
In conclusion, the incidence of poor neonatal outcomes for mothers with ITP is extremely low. We were unable to predict neonatal thrombocytopenia based on maternal factors such as treatment history or platelet count during pregnancy. The presence or absence of an infant's sibling with thrombocytopenia was the only parameter to predict the neonatal clinical course of a subsequent pregnancy.
Go to : 
References
1. Burrows RF, Kelton JG. Pregnancy in patients with idiopathic thrombocytopenic purpura: assessing the risks for the infant at delivery. Obstet Gynecol Surv. 1993; 48:781–788. PMID: 8309660.
2. Payne SD, Resnik R, Moore TR, Hedriana HL, Kelly TF. Maternal characteristics and risk of severe neonatal thrombocytopenia and intracranial hemorrhage in pregnancies complicated by autoimmune thrombocytopenia. Am J Obstet Gynecol. 1997; 177:149–155. PMID: 9240599.

3. Debouverie O, Roblot P, Roy-Peaud F, Boinot C, Pierre F, Pourrat O. Chronic idiopathic thrombocytopenia outcome during pregnancy (62 cases). Rev Med Interne. 2012; 33:426–432. PMID: 22677087.
4. Gill KK, Kelton JG. Management of idiopathic thrombocytopenic purpura in pregnancy. Semin Hematol. 2000; 37:275–289. PMID: 10942222.

5. Subbaiah M, Kumar S, Roy KK, Sharma JB, Singh N. Pregnancy outcome in patients with idiopathic thrombocytopenic purpura. Arch Gynecol Obstet. 2014; 289:269–273. PMID: 23852640.

6. Fujimura K, Harada Y, Fujimoto T, et al. Nationwide study of idiopathic thrombocytopenic purpura in pregnant women and the clinical influence on neonates. Int J Hematol. 2002; 75:426–433. PMID: 12041677.

7. Sukenik-Halevy R, Ellis MH, Fejgin MD. Management of immune thrombocytopenic purpura in pregnancy. Obstet Gynecol Surv. 2008; 63:182–188. PMID: 18279544.

8. Song TB, Lee JY, Kim YH, Choi YY. Low neonatal risk of thrombocytopenia in pregnancy associated with immune thrombocytopenic purpura. Fetal Diagn Ther. 1999; 14:216–219. PMID: 10420044.

9. Iyori H, Fujisawa K, Akatsuka J. Thrombocytopenia in neonates born to women with autoimmune thrombocytopenic purpura. Pediatr Hematol Oncol. 1997; 14:367–373. PMID: 9211541.
10. Tampakoudis P, Bili H, Lazaridis E, Anastasiadou E, Andreou A, Mantalenakis S. Prenatal diagnosis of intracranial hemorrhage secondary to maternal idiopathic thrombocytopenic purpura: a case report. Am J Perinatol. 1995; 12:268–270. PMID: 7575833.

11. Koyama S, Tomimatsu T, Sawada K, et al. Prenatal diagnosis of fetal intracranial hemorrhage in pregnancy complicated by idiopathic thrombocytopenic purpura. Prenat Diagn. 2010; 30:489–491. PMID: 20440739.

12. Burrows RF, Kelton JG. Fetal thrombocytopenia and its relation to maternal thrombocytopenia. N Engl J Med. 1993; 329:1463–1466. PMID: 8413457.

13. Yamada H, Kato EH, Kishida T, Negishi H, Makinoda S, Fujimoto S. Risk factors for neonatal thrombocytopenia in pregnancy complicated by idiopathic thrombocytopenic purpura. Ann Hematol. 1998; 76:211–214. PMID: 9671135.

14. Webert KE, Mittal R, Sigouin C, Heddle NM, Kelton JG. A retrospective 11-year analysis of obstetric patients with idiopathic thrombocytopenic purpura. Blood. 2003; 102:4306–4311. PMID: 12947011.

15. Valat AS, Caulier MT, Devos P, et al. Relationships between severe neonatal thrombocytopenia and maternal characteristics in pregnancies associated with autoimmune thrombocytopenia. Br J Haematol. 1998; 103:397–401. PMID: 9827911.

16. Sharon R, Tatarsky I. Low fetal morbidity in pregnancy associated with acute and chronic idiopathic thrombocytopenic purpura. Am J Hematol. 1994; 46:87–90. PMID: 8172201.

17. Mazzucconi MG, Petrelli V, Gandolfo GM, et al. Autoimmune thrombocytopenic purpura in pregnancy: maternal risk factors predictive of neonatal thrombocytopenia. Autoimmunity. 1993; 16:209–214. PMID: 8003616.

18. Koyama S, Tomimatsu T, Kanagawa T, Kumasawa K, Tsutsui T, Kimura T. Reliable predictors of neonatal immune thrombocytopenia in pregnant women with idiopathic thrombocytopenic purpura. Am J Hematol. 2012; 87:15–21. PMID: 22031338.

19. Yamada H, Kato EH, Kobashi G, et al. Passive immune thrombocytopenia in neonates of mothers with idiopathic thrombocytopenic purpura: incidence and risk factors. Semin Thromb Hemost. 1999; 25:491–496. PMID: 10625208.

20. Christiaens GC, Nieuwenhuis HK, Bussel JB. Comparison of platelet counts in first and second newborns of mothers with immune thrombocytopenic purpura. Obstet Gynecol. 1997; 90:546–552. PMID: 9380314.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download