Abstract
Background
Although bone marrow (BM) or mobilized peripheral blood (PB) is frequently used as the source of hematopoietic stem cells, hematopoietic stem cell transplantation (HSCT) using cord blood (CB) is gradually gaining popularity in many countries. However, BM or PB is still preferred over CB in Korea. Therefore, we tried to assess the awareness of CB transplantation (CBT) among domestic HSCT physicians and develop strategies for boosting its utilization by administering questionnaires to some of these physicians.
Methods
A direct questionnaire survey was conducted using the "Audience Response System" among 301 members who attended the annual meeting of the Korean Society of Blood and Marrow Transplantation. The data were analyzed for only 67 board certified physicians who were directly involved in HSCT activities.
Results
The poor outcomes resulting from insufficient experience in CBT was designated by the physicians as the main reason for the low domestic implementation of HSCT using CB. Other reasons identified in the survey were distrust in the quality and management of domestic CB and the high cost of obtaining CB.
Conclusion
Increasing the use of donated CB would foremost require increasing the inventory of donated CB containing a sufficient cell number for CBT and securing structured quality control of the CB banks. In addition, it would be necessary to minimize CB supply costs and continue to provide academic data, including CBT guidelines, so that clinicians could perform CBT with more confidence.
Cord blood (CB) has been an important source for hematopoietic stem cell transplantation (HSCT) since the early 1990s, and more than 30,000 patients with refractory hematological disease and malignant tumors have benefited from cord blood transplantation (CBT) worldwide in 2010 [1]. In Korea, the first successful CBT was performed in 1998 [2], and donated CB banks have appeared since then. In 2014, there are approximately 40,000 units of stored donated CB, and about 500 patients have received CBT [3]. However, the frequency of HSCT using donated CB is considerably lower in Korea than in Japan, Europe, or the United States (US) [4, 5, 6, 7].
Therefore, the aim of this study was to formulate strategies to increase the use of donated CB by identifying the perceptions of CBT by transplant physicians.
To obtain the general opinions regarding the management of donated CB and CBT, all attendees at an annual meeting of the Korean Society of Blood and Marrow Transplantation, which was held at the Grand Hilton Hotel, Seoul, Korea, were selected as the study subjects. The attendees included both medical doctors (MDs) and non-MDs engaged in the field of HSCT. Specifically, the questionnaire survey was administered to adults and pediatric hemato-oncologists (board certified physicians) who decided on the transplantation source for allogeneic HSCT and performed the procedures. The data from 67 physicians, among the 301 attendees, were analyzed.
To increase the efficiency of the questionnaire survey and obtain diverse opinions, a direct questionnaire survey was administered to the professionals indicated above using the "Audience Response System." The questionnaire included items concerning responders' basic knowledge, CBT experience, awareness of CBT, opinions on the frequency and cost of CBT, selection criteria for donors for allogeneic HSCT, and items related to improving domestic donated CBT activity.
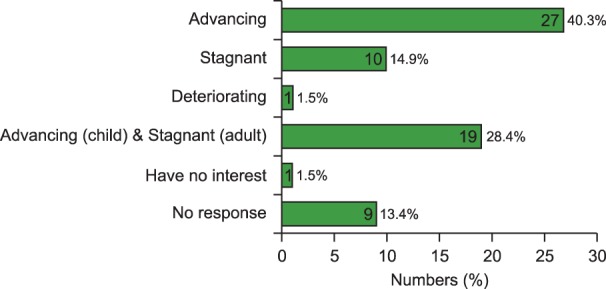
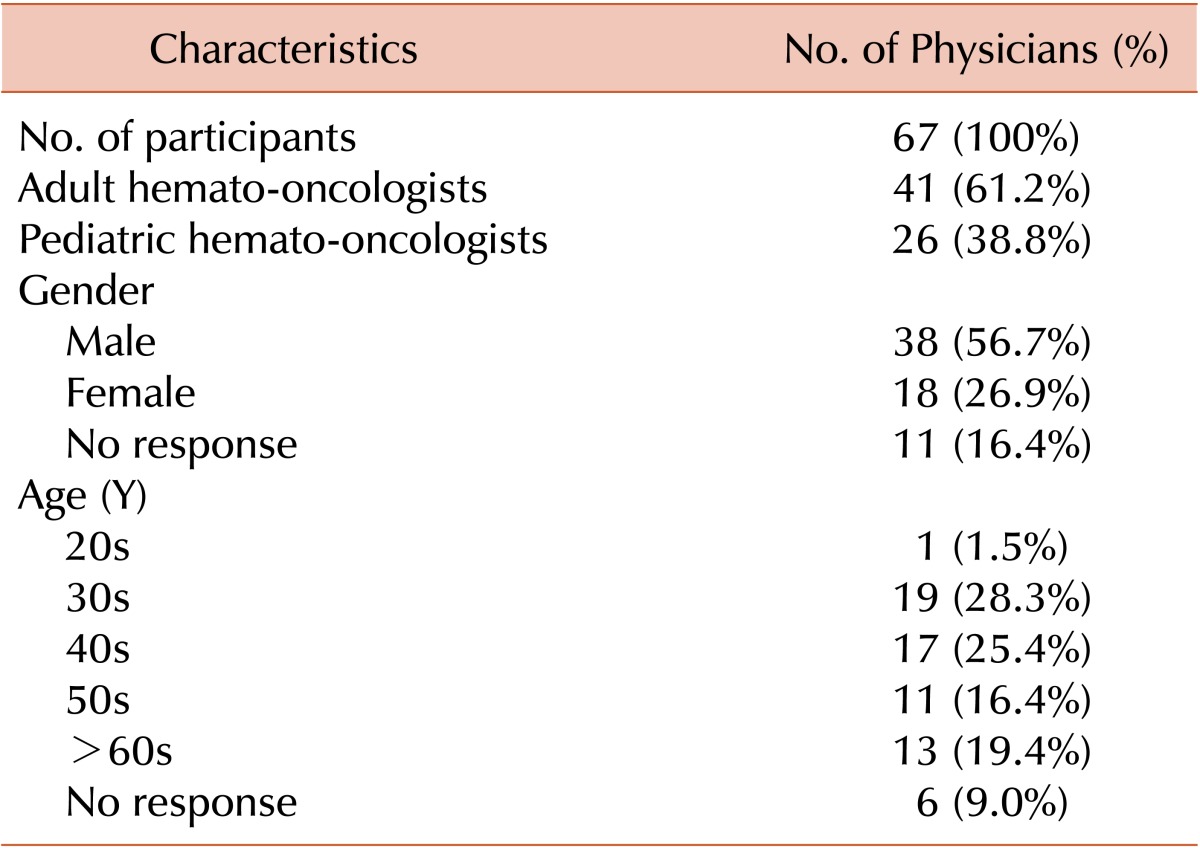
Basic information of the responders included gender, age, and their occupations (Table 1). Regarding the awareness of CBT advances worldwide, 40.3% of the participants said that CBT had advanced and 28.4% of participants believed that it was only advancing in the pediatric field (Fig. 1). The responses to a question about the status of advancement of domestic CBT in Korea, compared to the rest of the world, were similar to those regarding general awareness of CBT; 31.3% of respondents placed the pediatric field at a world-class level, but the adult field was placed at a level below world class (Fig. 2). When the participants answered the question about awareness of the handling and management of domestic CB, 40.3% of them distrusted the handling process and 58.2% distrusted the management system. Only 7.5% of physicians indicated trust in the handling and management of CB in general; however, 28.3% of participants responded with "do not know" or did not respond to the question (Fig. 3).
The most common reason provided for the low frequency of domestic CBT was the lack of experience (19.4%), followed by poor outcomes and bitter experience of CBT (16.4% and 14.9%, respectively) (Fig. 4). The wide range of potential donors was observed as an advantage of CBT by 44.7% of physicians, due to the ability to transplant without the need for fully matched domestic adult donors (Fig. 5A). However, inferior domestic CBT results (compared to other donors) was selected as the main reason that made choosing CBT difficult by 26.9% of physicians (Fig. 5B). Approximately, 37.3% of physicians selected distrust of the quality of CB as the most common factor making choosing CBT difficult with regard to surrounding conditions (Fig. 5C).
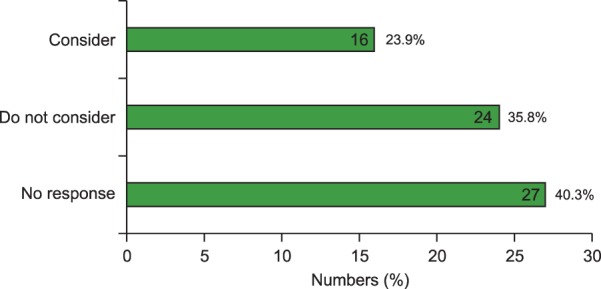
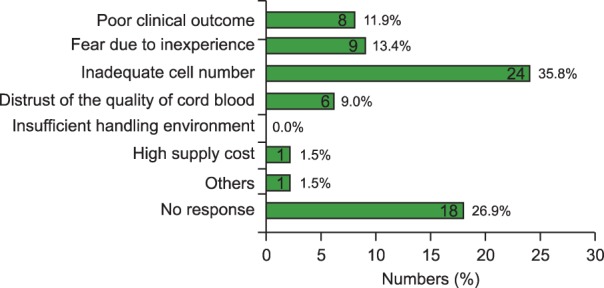
Physicians perceived that CBT had greater financial demands because 38.8% physicians believed that the price of CB was relatively high (Fig. 6A). When the participants were asked what the cost of CB should be, 22.5% of them felt that the price should be 80% of the current cost, which would be the same as the price for BM or PB donors (Fig. 6B). Over one-third (35.8%) of physicians did not consider CB as an alternative source, under the current domestic search arrangements, when searching for unrelated donors (Fig. 7). However, 56.7% of physicians believed that CB would be chosen more often if searching became easier and the search system was modified to allow BM/PB and CB data to be viewed simultaneously (Fig. 8). Only 16.4% of physicians selected donated CB as the next-favored donor when human leukocyte antigen (HLA)-matched domestic adult donors were unavailable. The order of choices among the physicians who were responsible for selecting donors was as follows: foreign unrelated adult donor, donated CB, domestic one-antigen mismatched unrelated adult donor, and mismatched family donor (Fig. 9). Among domestic CB searches since 2001, 100% resulted in matched searches including at least 4 of the 6 major HLA. Despite this, the most common reason for not choosing CBT was that it did not result in successful CBT because of inadequate cell numbers. This opinion was expressed by 35.8% of physicians (Fig. 10).
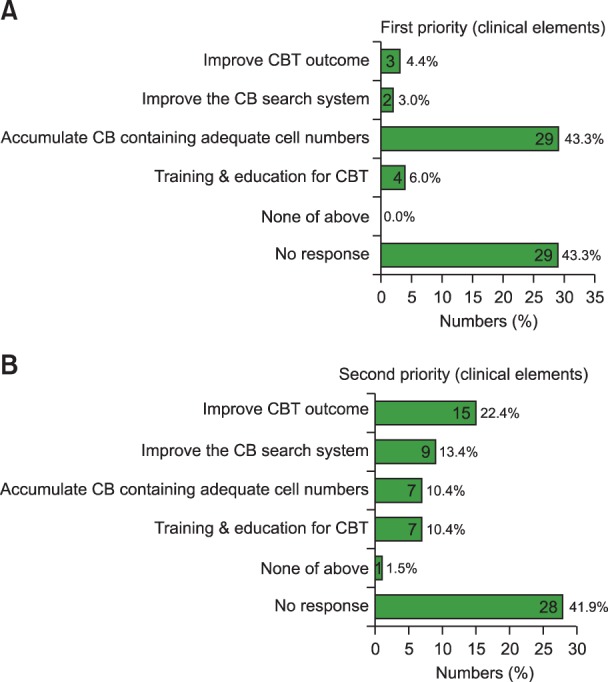
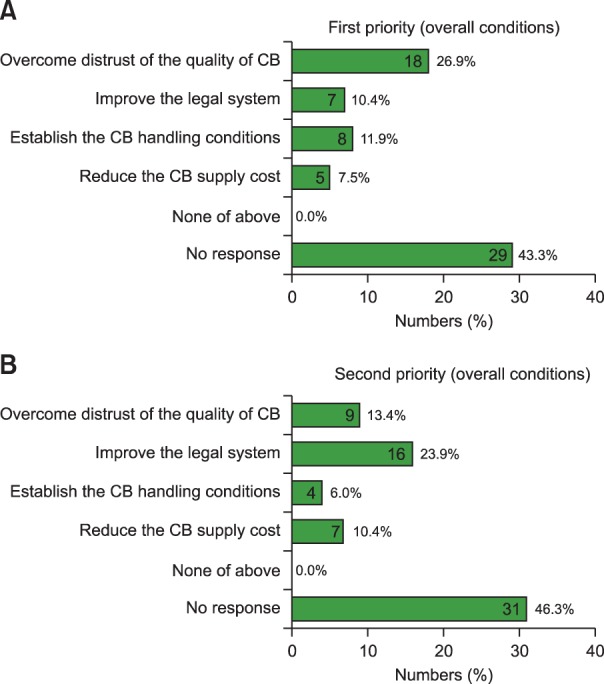
When physicians were asked about the most important factor that needs to be improved in the CBT field, the majority of them (43.3%) mentioned that CB with adequate cell numbers should be accumulated. The next clinical priority (22.4% of physicians) was that the outcome of domestic CBT should be improved (Fig. 11). With regards to overall conditions, 26.9% of physicians thought that the distrust relating to CB quality should be solved in order for transplantation to be performed more frequently. The next environmental priority (23.9% of physicians) was that domestic CBT should be revitalized by improving the legal system relating to CB and strengthening the management system (Fig. 12).
Utilization levels of donated CB are high in Japan, with approximately 30.1% utilization according to Japan Cord Blood Bank Network data [4]. Utilization levels are lower in the US (approximately 4.3%, the National Marrow Donor Program) [5, 6] and worldwide (6.3%, World Marrow Donor Association) [7]. However, the utilization of donated CB is even lower in Korea (1.2%) compared to Japan and the world standard [3]. In this questionnaire survey of physicians, 40.3% of them expressed that a lack of trust due to inadequate CB handling standards was the primary reason for the low utilization rate of donated CB. Their distrust of medical personnel in the banking facilities of donated CB mostly resulted from direct onsite experience. Physicians often experienced that the total nucleated cell (TNC) numbers, CD34 positive cells, and the cell viability indicated by the pre-cryopreservation CB bank data were different from the data obtained at the physicians' transplantation units when the CB is re-tested directly after thawing, which can lead to distrust in the CB banking procedures by many physicians. In addition, CB containing more nucleated cells tends to be selected because the most important factor determining the outcome of CBT was the TNC count [8]. Furthermore, the choices are limited because the majority of the CB samples preserved in Korea have a relatively low TNC [9], and therefore, there is a prevailing perception that only low quality CB is preserved.
The second reason behind the low usage rate of donated CB in Korea was the lack of clinical experience of CBT and uncertainty regarding clinical outcomes. In fact, the two most prevalent reasons given in response to why it was difficult to choose CB for unrelated HSCT included a lack of CBT experience and previous experience of negative results. The practical results obtained with CBT in Korea are not worse than those in other countries [10] and therefore, we believe that we can achieve clinical results comparable to other countries if recent domestic and foreign clinical data, as well as clinical experience in Korea to date, were shared.
The third reason for the low usage rate of donated CB was the supply cost of donated CB. CB costs about 25,000 USD in the US, which is similar to the cost of using an unrelated BM/PB donor (about 35,000 USD). In Taiwan, the cost is about 12,000 USD, which is 2-3 times the cost of using an unrelated BM/PB donor (about 4,800 USD). In Japan, CB is provided free of charge while the cost of using an unrelated BM/PB donor is about 2,100 USD. In Korea, it has recently been supplied at 4,000 USD per unit or 6,000 USD per 2 units, which is still more expensive compared to Japan [3]. About 60% of the respondents in our questionnaire mentioned that the current prices of CB should be lowered.
We believe that a strategy, such as the one outlined below, must be implemented to increase the use of donated CB in Korea at least to the level in other countries. Firstly, the confidence of the CB management system has to be gained through education and improvement. To accomplish this, a CB bank inspection system should be established based on the law governing CB management and research [11]. In addition, a revision of the current program is necessary to streamline the CB search system for unrelated stem cell donors. In the current computer program for unrelated stem cell donors, BM/PB and CB donors are located in different folders, which results in poor CB search results [12]. Therefore, revising the computer program to show all stem cell donors in the same folder would make CB selection easier, which can promote the use of donated CB.
Secondly, the quality of preserved CB should be improved to increase confidence. To accomplish this, it is important to maintain a considerable level of qualified CB by continuously coordinating data between CB banks and medical facilities to eliminate data mismatches and by improving and standardizing CB collection methods. There are several variables that make it difficult to accurately compare TNC counts, CD34+ cell counts, and cell viabilities before and after cryopreservation. Therefore, to eliminate mistrust due to the difference in cell counts before and after cryopreservation, guidelines for the interpretation of CB cell data should take into account the fact that the TNC count decreases continuously during CB processing, and after thawing [13]. In other words, a transplantation specialist who has made a transplantation decision solely on the basis of pre-cryopreservation CB bank data should learn not to distrust the CB bank simply because their data is different from the post-thawing transplantation facility data. Instead, the specialist should consider the above facts when considering CB. The CB collection step, the first step in CB preservation, plays an important role in obtaining good quality CB. Furthermore, the interest, commitment, and technique of a collector can influence the quality and quantity of CB. Therefore, continuous education and standardization of the work of medical personnel in obstetrics and gynecology is necessary. A future prospective study will also be required in this regard. It is also important to obtain a large amount of good quality CB by raising the cryopreservation standards for donated CB.
Thirdly, it will be necessary to minimize the burden of costs associated with donated CB for recipients to increase the use of CB. In Korea, a national budget for a donated CB enterprise is currently being drafted based on the law governing CB management and research. However, the current national budget only supports the cost of certain aspects of CB processing. Although the cost of CB has been reduced to 4,000 USD per unit and 6,000 USD per 2 units for CB banks designated by the Ministry of Health and Welfare in recent times, ultimately providing CB free of charge or making it part of the health insurance reimbursement schemes would help increase its use.
In conclusion, increasing the inventory of donated CB with cell numbers sufficient for CBT and to securing structured quality control of the CB banks can increase the use of donated CB. In addition, it is vital to minimize CB supply costs and continue to provide academic data, including CBT guidelines, so that clinicians can be more confident about performing CBT.
ACKNOWLEDGEMENTS
We are grateful to all the members of the Korean Society of Blood and Marrow Transplantation, and particularly to the members of the Cord Blood Committee.
References
1. Ballen KK, Gluckman E, Broxmeyer HE. Umbilical cord blood transplantation: the first 25 years and beyond. Blood. 2013; 122:491–498. PMID: 23673863.

2. Lee YH, Cho NC, Je KH, et al. Successful sibling cord blood stem cell transplantation for relapsed acute mixed lineage leukemic. Korean J Hematol. 1999; 34:471–476.
3. Status of storage and transplantation of cord blood and an itemized account of patient's charges using cord blood. Seoul, Korea: Korea Marrow Donor Program;2014. Accessed June 5, 2014. at http://www.kmdp.or.kr.
4. Annual and cumulative incidence of unrelated hematopoietic stem cell transplantation according to the stem cell sources. Tokyo, Japan: Japan Marrow Donor Program;2012. Accessed June 5, 2014. at http://www.jmdp.or.jp/documents/file/07_about_us/press/press_12_08_29.pdf.
5. Growth of the cord blood registry. Minneapolis, MN: National Marrow Donor Program;2013. Accessed June 5, 2014. at https://bethematchclinical.org/Transplant-Therapy-and-Donor-Matching/Donor-or-Cord-Blood-Search-Process/Likelihood-of-Finding-a-Match/.
6. Transplants by cell source, 1990-2013. Minneapolis, MN: National Marrow Donor Program;2013. Accessed June 5, 2014. at https://bethematchclinical.org/Transplant-Therapy-and-Donor-Matching/Cell-Sources/.
7. Cord blood banking introduction-State of the art. Monaco: The World Marrow Donor Association;2013. Accessed June 5, 2014. at http://www.esh.org/wp-content/uploads/2013/11/Session-VState-of-the-art.pptx-Lecture-seule.pdf.
8. Barker JN, Scaradavou A, Stevens CE. Combined effect of total nucleated cell dose and HLA match on transplantation outcome in 1061 cord blood recipients with hematologic malignancies. Blood. 2010; 115:1843–1849. PMID: 20029048.

9. Lee YH, Kwon YH, Hwang K, et al. Analysis of stored and transplanted cord blood units from KoreaCORD: reappraisal of banking guidelines and selection strategy. Transfusion. 2013; 53:123–127. PMID: 22612248.

10. Yoo KH, Lee SH, Sung KW, et al. Current status of pediatric umbilical cord blood transplantation in Korea: a multicenter retrospective analysis of 236 cases. Am J Hematol. 2011; 86:12–17. PMID: 21064135.

11. The law for cord blood management and research. Seoul, Korea: Ministry of Health & Welfare;2011. Accessed June 5, 2014. at http://www.mw.go.kr/front_new/index.jsp.
12. Information system for searching unrelated hematopoietic stem cell donors. Cheongju, Korea: Comprehensive Management System for Disease and Health;2013. Accessed June 5, 2014. at http://is.cdc.go.kr/.
13. Laroche V, McKenna DH, Moroff G, Schierman T, Kadidlo D, McCullough J. Cell loss and recovery in umbilical cord blood processing: a comparison of postthaw and postwash samples. Transfusion. 2005; 45:1909–1916. PMID: 16371043.

Fig. 2
General awareness of domestic cord blood transplantation in Korea, regarding knowledge, procedure, and outcome of cord blood transplantation, compared to world class. Abbreviation: W/C, world class.

Fig. 4
Reasons for the low frequency of domestic cord blood transplantation. Abbreviation: CBT, cord blood transplantation.

Fig. 5
The advantages (A) and disadvantages (B, C) of cord blood as an alternative source. Abbreviations: BM, bone marrow; PB, peripheral blood.

Fig. 6
Opinions about the current supply cost of cord blood (A) and expectations for the supply cost (B).
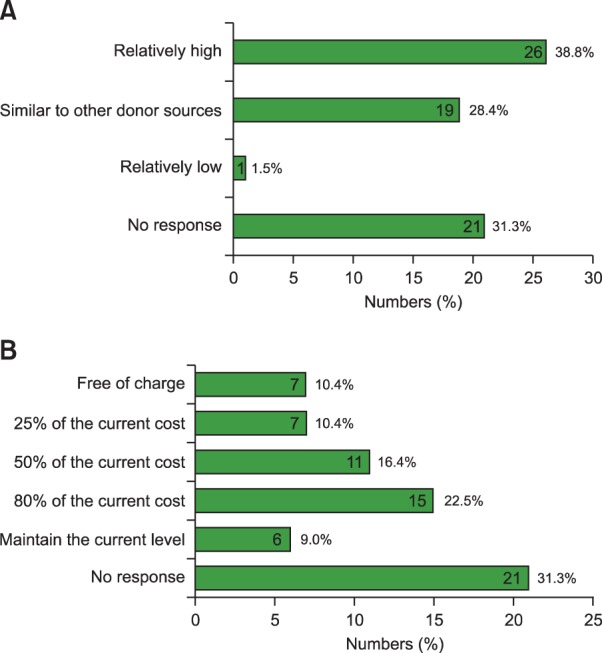
Fig. 8
Opportunity to select cord blood when the search program is upgraded to include unrelated donors simultaneously.
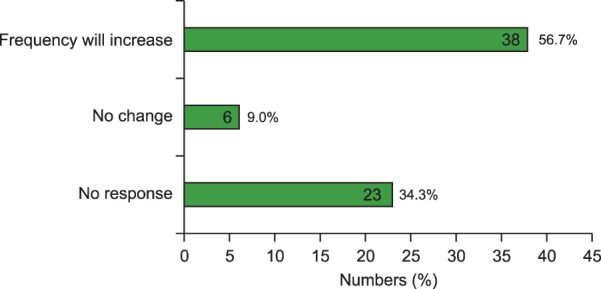
Fig. 9
The choice of next donor when a HLA-matched domestic unrelated adult donor is unavailable. Abbreviation: Ag, antigen.
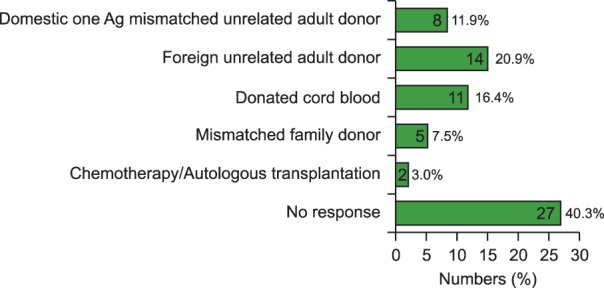
Fig. 11
Opinions regarding promoting domestic cord blood transplantation (clinical elements). Abbreviations: CBT, cord blood transplantation; CB, cord blood.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download