1. Collins P, Macartney N, Davies R, Lees S, Giddings J, Majer R. A population based, unselected, consecutive cohort of patients with acquired haemophilia A. Br J Haematol. 2004; 124:86–90. PMID:
14675412.
2. Collins PW, Hirsch S, Baglin TP, et al. Acquired hemophilia A in the United Kingdom: a 2-year national surveillance study by the United Kingdom Haemophilia Centre Doctors' Organisation. Blood. 2007; 109:1870–1877. PMID:
17047148.

3. Franchini M, Montagnana M, Lippi G. Clinical, laboratory and therapeutic aspects of platelet-type von Willebrand disease. Int J Lab Hematol. 2008; 30:91–94. PMID:
18333841.

4. Meiklejohn DJ, Watson HG. Acquired haemophilia in association with organ-specific autoimmune disease. Haemophilia. 2001; 7:523–525. PMID:
11554945.

5. Sallah S, Wan JY. Inhibitors against factor VIII in patients with cancer. Analysis of 41 patients. Cancer. 2001; 91:1067–1074. PMID:
11267950.
6. Solymoss S. Postpartum acquired factor VIII inhibitors: results of a survey. Am J Hematol. 1998; 59:1–4. PMID:
9723568.

7. Defendenti C, Atzeni F, Spina MF, et al. Clinical and laboratory aspects of Ro/SSA-52 autoantibodies. Autoimmun Rev. 2011; 10:150–154. PMID:
20854935.

8. Lavigne-Lissalde G, Schved JF, Granier C, Villard S. Anti-factor VIII antibodies: a 2005 update. Thromb Haemost. 2005; 94:760–769. PMID:
16270627.

9. Lavigne-Lissalde G, Rothschild C, Pouplard C, et al. Characteristics, mechanisms of action, and epitope mapping of anti-factor VIII antibodies. Clin Rev Allergy Immunol. 2009; 37:67–79. PMID:
19172415.

10. Scandella D, Mattingly M, de Graaf S, Fulcher CA. Localization of epitopes for human factor VIII inhibitor antibodies by immunoblotting and antibody neutralization. Blood. 1989; 74:1618–1626. PMID:
2477082.

11. Fulcher CA, de Graaf Mahoney S, Roberts JR, Kasper CK, Zimmerman TS. Localization of human factor FVIII inhibitor epitopes to two polypeptide fragments. Proc Natl Acad Sci U S A. 1985; 82:7728–7732. PMID:
2415970.

12. Scandella D, Gilbert GE, Shima M, et al. Some factor VIII inhibitor antibodies recognize a common epitope corresponding to C2 domain amino acids 2248 through 2312, which overlap a phospholipid-binding site. Blood. 1995; 86:1811–1819. PMID:
7544643.

13. Bray GL, Kroner BL, Arkin S, et al. Loss of high-responder inhibitors in patients with severe hemophilia A and human immunodeficiency virus type 1 infection: a report from the Multi-Center Hemophilia Cohort Study. Am J Hematol. 1993; 42:375–379. PMID:
8493988.

14. Reding MT, Lei S, Lei H, Green D, Gill J, Conti-Fine BM. Distribution of Th1- and Th2-induced anti-factor VIII IgG subclasses in congenital and acquired hemophilia patients. Thromb Haemost. 2002; 88:568–575. PMID:
12362225.

15. The Korean Society on Thrombosis and Hemostasis. The guidelines of Hemophilia. 2011. Seoul, Korea: Han Kuk Medical Publisher;p. 115–120.
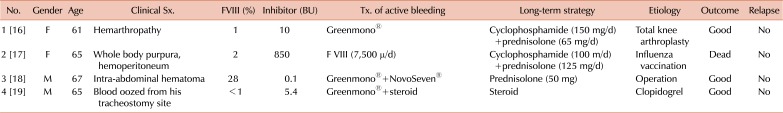
16. Song MH, Ahn SJ, Yoo SH, Kim BH, Park JH. Total knee arthroplasty-associated acquired hemophilia: a case report. J Korean Orthop Assoc. 2006; 41:167–169.

17. Chung BH, Kim YJ, Kim MS, et al. A case of acquired hemophilia detected after influenza vaccination. Korean J Med. 2004; 66:298–301.
18. Lee N, Yoon SH, Lim W, et al. Post-operative bleeding due to acquired hemophilia successfully treated with recombinant factor VIIa: case report. Korean J Hematol. 2009; 44:163–167.

19. Hwang HW, Kong JH, Yu DW, Kim WT, Kim HS, Lee CI. A patient with acquired hemophilia A induced by clopidogrel. Korean J Hematol. 2012; 47:80–82. PMID:
22479283.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download