TO THE EDITOR: Acute leukemia during pregnancy is rare [1-8]. The exact incidence of acute promyelocytic leukemia (APL) in pregnant women is unknown; however, approximately 50 such cases have been reported in the literature [1-4, 7, 8]. APL is a unique type of acute myeloid leukemia (AML) characterized by proliferation of neoplastic promyelocytes bearing a specific chromosomal translocation t(15;17). We report a case of APL with an unusual presentation of secondary postpartum hemorrhage (PPH).
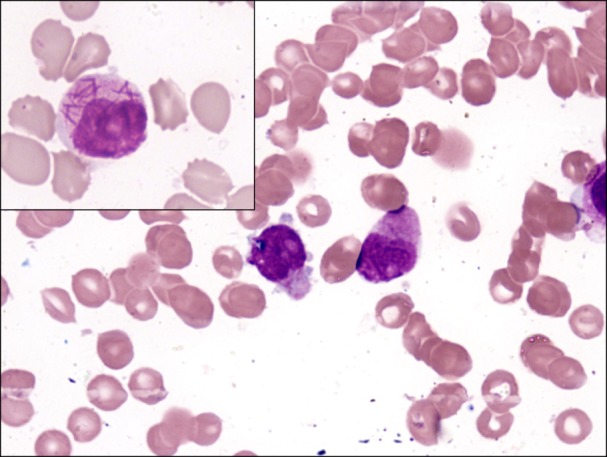
A 30-year-old woman (gravida 2, para 2, abortus 0) delivered a 2.1 kg baby girl through normal vaginal delivery but was otherwise healthy. She received 2 units of whole blood transfusion during labor and was discharged 3 days later. However, she was re-admitted 6 days following discharge with complaints of excessive bleeding per vaginum and bleeding gums. On examination, she was pale and afebrile with a pulse rate of 72 beats/min and blood pressure of 110/70 mmHg. There was no icterus, pedal edema, or lymphadenopathy, and no complaint of fever or bruising. Ultrasound revealed clots within the uterus possibly due to retained products of conception. There was hepatomegaly but no splenomegaly. Hematological investigations revealed the followings: hemoglobin level, 8.8 g/dL; total leukocyte count, 6.5×106/L; platelet count, 44×109/L; hematocrit, 24.4%; red blood cell count, 2.62×109/L; differential leukocyte count: blasts, 2%; promyelocytes, 65%; neutrophils, 4%; and lymphocytes, 29%. The abnormal promyelocytes were 2-4 times the size of small mature lymphocytes and had a moderate amount of cytoplasm with granules and Auer rods. The nuclei contained fine chromatin and 1-3 prominent nucleoli, and hallmark faggot cells were also observed (Fig. 1). The promyelocytes were strongly positive for myeloperoxidase. She was diagnosed with AML, suggestive of APL. Bone marrow aspiration was advised along with immunophenotyping and cytogenetic studies. The coagulation profile revealed the followings: prothrombin time, 15 sec (control, 13 sec); activated partial thromboplastin time, 31 sec (control, 30 sec); serum fibrinogen level, 110 mg/dL; D-Dimer level, 16-32 µg/mL fibrinogen equivalent units (reference range, <0.5 µg/mL fibrinogen equivalent units). Other biochemical tests were within normal limits. However, the patient died of hypovolemic shock following excessive blood loss. Therefore, further investigations could not be performed. During the antenatal period, the patient had a hemoglobin range of 9-9.5 g/dL, a total leukocyte count of 6-8×106/L, and a platelet count of 160-190×109/L. A peripheral blood smear revealed microcytic hypochromic red cells; however, no abnormal cells or blasts were seen on any smears during the antenatal period. Moreover, she had a normal coagulation profile.
Acute leukemia during pregnancy is very rare with an estimated frequency of 1 in 75,000-100,000 [3, 6, 7]. AML accounts for approximately two-thirds of leukemia cases seen during pregnancy and the diagnosis is generally made during the second and third trimesters [3, 5]. PPH is occasionally due to an underlying coagulation or hematologic disorder, but PPH as a presentation of APL is extremely rare [8]. APL is commonly complicated by disseminated intravascular coagulation (DIC), seen in >90% of patients, and a life-threatening hemorrhage can occur in the brain, gut, or less frequently, the uterus. In such cases, it is very important to diagnose the underlying disorder as APL and it is curable with a good prognosis. The treatment of choice for APL is all-trans retinoic acid followed by conventional chemotherapy [1-3]. This case report is important as it highlights the fact that APL can be a rare cause of PPH. A peripheral blood smear should be performed in all cases of unexplained DIC.
References
1. Consoli U, Figuera A, Milone G, et al. Acute promyelocytic leukemia during pregnancy: report of 3 cases. Int J Hematol. 2004; 79:31–36. PMID: 14979475.

2. Carradice D, Austin N, Bayston K, Ganly PS. Successful treatment of acute promyelocytic leukaemia during pregnancy. Clin Lab Haematol. 2002; 24:307–311. PMID: 12358893.

3. Chelghoum Y, Vey N, Raffoux E, et al. Acute leukemia during pregnancy: a report on 37 patients and a review of the literature. Cancer. 2005; 104:110–117. PMID: 15912518.
4. Park TS, Lee ST, Kim JS, et al. Acute promyelocytic leukemia in early pregnancy with translocation t(15;17) and variant PML/RARA fusion transcripts. Cancer Genet Cytogenet. 2009; 188:48–51. PMID: 19061780.

5. Firas AS, Demeckova E, Mistrik M. Leukemia in pregnancy. Bratisl Lek Listy. 2008; 109:364–366. PMID: 18837246.
6. Feliu J, Juarez S, Ordonez A, Garcia-Paredes ML, Gonzalez-Baron M, Montero JM. Acute leukemia and pregnancy. Cancer. 1988; 61:580–584. PMID: 3422173.

7. Hoffman MA, Wiernik PH, Kleiner GJ. Acute promyelocytic leukemia and pregnancy. A case report. Cancer. 1995; 76:2237–2241. PMID: 8635026.

8. Sharma JB, Gupta N, Vimala N, Anand M, Deka D, Mittal S. Acute promyelocytic leukemia: an unusual cause of fatal secondary postpartum hemorrhage. Arch Gynecol Obstet. 2006; 273:310–311. PMID: 16341866.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download