TO THE EDITOR: Although much is known about hypereosinophilic syndrome (HES), the notable discovery of a few genetic rearrangements, such as FIP1L1/PDGFRA (F/P) and TEL/PDGFRB, and the identification of a phenotypically aberrant clonal T lymphocyte brought a new paradigm to HES. As a result, multidisciplinary groups of hematologists and scientists have created more stratified treatment guidelines for patients with HES.
However, more than half of patients with HES are still classified as undefined under the current diagnostic criteria and the best course of treatment for these patients remains unclear, especially after initial steroid treatments fail. Here, we present two cases of undefined HES who were successfully treated with cyclosporine A (CsA) after corticosteroid treatment failed.
A 41-year-old man visited our emergency room with rashes on both legs and his trunk area.
On physical examination, only a skin lesion was found. His complete blood count (CBC) showed hypereosinophilia (eosinophils 4,730/mm3). Although he had no history of allergies, a previous CBC reports showed persistent hypereosinophilia over the previous 6 months.
Subsequent analyses did not reveal any evidence of secondary HES including any autoimmune disease or parasitic infestation. Bone marrow aspirate and biopsy showed marked eosinophilia without dyspoiesis. FIP1L1-PDGFRA, TEL-PDGFRB, or BCR-ABL rearrangement was not detected on fluorescence in situ hybridization. JAK2 V617F mutation analysis performed with a reverse transcription polymerase chain reaction technique was negative. Serum immunoglobulin E (IgE) level (1,599 mg/dL) and eosinophilic cationic protein level (163.35 ng/mL) were elevated.
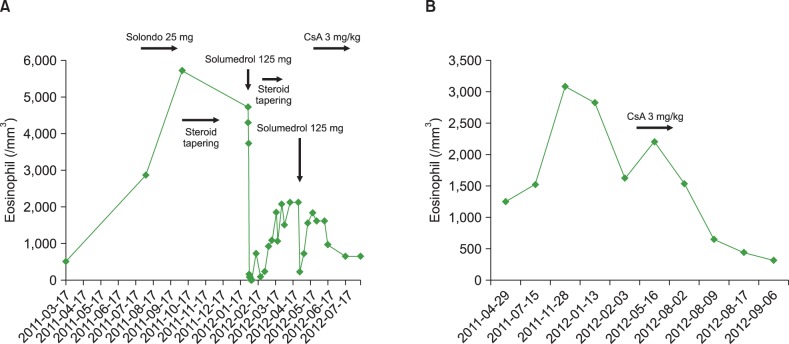
Skin biopsy of the leg rash showed perivascular lymphohistiocytic infiltration and many eosinophils. Flow cytometric analysis to evaluate the associated aberrant T-lymphocyte found no abnormal phenotypes such as CD3-CD4+ or CD3+CD4-CD8-, but the T cell receptor (TCR) gene rearrangement was not checked. Although we could not confirm the subclass of HES, clinical findings indicated a lymphocytic variant of HES (L-HES). The patient initially responded well to a high-dose glucocorticoid treatment, but after reducing prednisone, the eosinophil count and IgE level rebounded. Thus, we administered a low dose of CsA (100 mg bid), and his eosinophil count returned to normal after just 1 week of treatment. Prednisone was then tapered to 10 mg per day (Fig. 1A).
A 41-year-old man who had been suffering from intractable eosinophilic pustular folliculitis for 5 years was referred to our hospital. Skin biopsy from the lesion showed perivascular and periadnexal eosinophilic infiltration. He had no history of allergies. Although he had been taking dapsone, prednisone, and an antihistamine since 2008, his skin lesion had waxed and waned and the CBC showed persistent hypereosinophilia for over 1 year. The laboratory results showed an eosinophil count of 1,790/mm3 and a serum IgE level of 119 IU/mL. Nevertheless, there was no evidence of secondary HES. Sequentially performed bone-marrow aspiration and biopsy showed hyperplasia of the eosinophilic lineage, but the molecular analysis did not show any specific aberrant genetic mutations consistent with the myelocytic variant of HES (M-HES). Unfortunately, we did not analyze the T cell phenotype and T cell clonality. On physical examination, only skin manifestations were found. The patient could not be categorized as L-HES according to the laboratory results; however, considering the relatively gentle clinical course and absence of cardiac involvement, we selected an immune-modulating drug as a second line treatment rather than a cytotoxic agent or imatinib. We administered a low dose of CsA (100 mg bid), and his eosinophil count returned to normal after 1 week of treatment. In addition, his skin lesion disappeared (Fig. 1B).
Previously, the diagnosis of HES was usually based on exclusion and treatment included mostly steroids and cytotoxic agents. With the improved understanding of the pathogenesis of HES, distinguishing M-HES from non-M-HES and analyzing the F/P rearrangement have become prerequisites for optimizing HES treatment. However, steroids still play a major role as the first line treatment for HES, except for F/P positive HES, which should be treated with imatinib.
Corticosteroids are known to interfere with the transcription of pro-inflammatory genes necessary for eosinophil maturation, proliferation, migration, and chemo-attraction. Because these mechanisms perform diverse actions, corticosteroids have been used for decades to treat HES, irrespective of the subtype. However, the accompanying side effects of systemic corticosteroids preclude long-term usage and some patients with HES respond only to a high dose of steroids or are resistant to steroid treatment. Nevertheless, treatment guidelines after failure or intolerance of glucocorticoid therapy for HES have not been established.
In a review of the literature on HES treatment, previous reports mention various second lines of treatment including hydroxyurea, leukapheresis, vincristine, 6-mercaptopurine, IFN-α, or allogenic bone marrow transplantation, but most were case studies or retrospective analyses.
According to the largest study, a retrospective analysis on HES treatment, 163 patients of 188 (81%) without FP rearrangement received corticosteroids as the initial therapy; 85% of these patients experienced a favorable response [1]. However, 42% of these patients eventually had to discontinue steroid use or add another drug because of treatment failure or steroid toxicity. Furthermore, the most frequently combined agent was hydroxyurea. Therefore, considering the different prognoses and natural course of M-HES and L-HES, different approaches to treatment are needed to avoid unnecessary exposure to cytotoxic drugs.
Since Cogan et al. discovered the aberrant T lymphocyte clone in one patient with HES with a high interleukin 5 level, L-HES was defined as a lymphoid disorder caused by a sustained over-production of eosinopoietic cytokines such as interleukin 5 from T-lymphocytes that have undergone clonal expansion or aberrant T-lymphocytes [2]. Furthermore, these discoveries of a lymphocyte-based pathogenetic mechanism aroused attention regarding an immune-mediated treatment approach targeting lymphocytes for the treatment of L-HES. Compared with other immune-modulating drugs such as mepolizumab or IFN-α, CsA has not received much attention for the treatment of HES. However, systemic toxicity and a possible inhibitory effect on apoptosis of aberrant CD3-CD4+ T cells became an obstacle for the widespread application of IFN-α in the treatment of L-HES [3-5]. Thus, further studies are needed to link the anti-apoptotic effect on aberrant T cells with subsequent lymphoma. Although a few prospective studies on mepolizumab recently showed positive results, high cost can be a limitation in widespread use and the results of long-term use along with the toxicity profile are still unknown [6, 7]. CsA, a calcineurine inhibitor, has been used to prevent rejection after organ transplant because of its inhibitory effect on interleukin 2 production of T cells. The feasible toxicity profile and effective T-lymphocyte suppression properties of CsA made this drug applicable to many T lymphocyte-related diseases. However, not many studies have investigated the use of CsA for the treatment of HES; the first report was in 1996 [8]. A 7-year-old girl presented with a maculopapular rash with erosion over her entire body with hypereosinophilia and hyper IgE. Because she could not maintain a high dose of steroids and had a cushingoid appearance, 3 mg/kg of CsA was administered. Just one week after CsA administration, the eosinophil count returned to normal and she was weaned off corticosteroid use at an increment dose of up to 8 mg/kg. In 2009, the first adult case was reported. A 63-year-old man was diagnosed with L-HES by performing TCR gene rearrangement [9]. The patient did not respond to initial prednisone therapy or subsequent hydroxyurea. However, a low dose of CsA (100 mg/day) was attempted and a complete resolution was achieved. In our two cases, both patients also showed a favorable response 1 week after CsA administration and a 3-4 mg/kg dose was enough for to control the disease. Although we could not categorize our two cases into an HES subtype, a number of clinical features caused us to treat them as L-HES cases; thus, CsA was selected as the second line of treatment.
Firstly, both cases did not show an F/P rearrangement and were partially responsive to the initial steroid treatment. Secondly, neither patient had M-HES features such as hepatosplenomegaly, cardiac eosinophilic involvement, or a high vitamin B12 level. Lastly, both cases showed dermatologic manifestations. While an effort to find reliable clinical indicators that predict treatment response and help classify the subtype of HES has continued, a few parameters were suggested and some were accepted as minor criteria in differentiating between the subclasses of HES, such as serum thymus and regulated chemokine, IgE, interleukin 5, tryptase level, and organ involvement patterns [10, 11]. Even if these factors are not absolute indicators, a combination of these clinical parameters is expected to help predict treatment outcomes and select optimal drugs in patients with undefined HES.
Moreover, further prospective investigation is needed to clarify the effectiveness of CsA in non-M-HES patients; however, CsA may be a feasible and effective second-line drug for L-HES and patients with undefined HES with similar features.
References
1. Ogbogu PU, Bochner BS, Butterfield JH, et al. Hypereosinophilic syndrome: a multicenter, retrospective analysis of clinical characteristics and response to therapy. J Allergy Clin Immunol. 2009; 124:1319–1325.e3. PMID: 19910029.

2. Cogan E, Schandene L, Crusiaux A, Cochaux P, Velu T, Goldman M. Brief report: clonal proliferation of type 2 helper T cells in a man with the hypereosinophilic syndrome. N Engl J Med. 1994; 330:535–538. PMID: 8302319.
3. Butterfield JH. Interferon treatment for hypereosinophilic syndromes and systemic mastocytosis. Acta Haematol. 2005; 114:26–40. PMID: 15995323.

4. Schandené L, Roufosse F, de Lavareille A, et al. Interferon alpha prevents spontaneous apoptosis of clonal Th2 cells associated with chronic hypereosinophilia. Blood. 2000; 96:4285–4292. PMID: 11110703.
5. Klion AD, Bochner BS, Gleich GJ, et al. Approaches to the treatment of hypereosinophilic syndromes: a workshop summary report. J Allergy Clin Immunol. 2006; 117:1292–1302. PMID: 16750989.

6. Rothenberg ME, Klion AD, Roufosse FE, et al. Treatment of patients with the hypereosinophilic syndrome with mepolizumab. N Engl J Med. 2008; 358:1215–1228. PMID: 18344568.

7. Roufosse F, de Lavareille A, Schandene L, et al. Mepolizumab as a corticosteroid-sparing agent in lymphocytic variant hypereosinophilic syndrome. J Allergy Clin Immunol. 2010; 126:828–835.e3. PMID: 20810155.

8. Nadarajah S, Krafchik B, Roifman C, Horgan-Bell C. Treatment of hypereosinophilic syndrome in a child using cyclosporine: implication for a primary T-cell abnormality. Pediatrics. 1997; 99:630–633. PMID: 9093318.

9. Donald CE, Kahn MJ. Successful treatment of hypereosinophilic syndrome with cyclosporine. Am J Med Sci. 2009; 337:65–66. PMID: 19002011.

10. Roufosse F. Hypereosinophilic syndrome variants: diagnostic and therapeutic considerations. Haematologica. 2009; 94:1188–1193. PMID: 19734412.

11. Klion AD. Recent advances in the diagnosis and treatment of hypereosinophilic syndromes. Hematology Am Soc Hematol Educ Program. 2005; 209–214. PMID: 16304382.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download