Abstract
The Consortium for Improving Survival of Lymphoma (CISL) in Korean Society of Hematology Lymphoma Working Party had first meeting in February, 2006 with 10 institutions and 12 members. Now CISL comprised of 64 centers. CISL has concentrated research activity on lymphomas which are relatively frequent in Korea and has tried to give favors for the Korean lymphoma patients. CISL has conducted more than 30 retrospective studies to evaluate Korean peculiar lymphoma subtypes. More than 30 prospective trials have been being performed for diffuse large B-cell lymphoma, marginal zone lymphoma, extra-nodal NK/T-cell lymphoma, and so on. The first prospective trial for advanced marginal zone lymphoma has led to use Rituximab containing chemotherapy with the re-imbursement of health insurance in Korea. The multi-center trials of the CISL with new therapeutic modalities will improve further the survival of lymphoma patients not only quantitatively but also qualitatively.
Lymphomas are clonal neoplasms of B cells, T cells, or natural killer (NK) cells [1, 2]. Recently, changes in how lymphomas are classified, proposals for new subtype entities, and the development of innovative treatment modalities that utilize novel therapeutic agents have stimulated a paradigm shift in the diagnosis and management of lymphomas [3]. Accompanying these advances, the Consortium for Improving Survival of Lymphoma (CISL) of the Korean Society of Hematology Lymphoma Working Party (KLWP) first met in 2006. CISL has concentrated its attention on the types of lymphoma that occur most frequently in the Korean population and their unique features and has tried to conduct research that could be of benefit to Korean patients with lymphoma. Here, we summarize the clinical studies performed by CISL.
KLWP, founded in October 2005, is responsible not only for trials against lymphoma but also for administrative work, patient education, and other work/projects related to lymphoma control and treatment in Korea. With the need for more comprehensive and active clinical research, we formed a clinical study group for lymphoma. In the first CISL meeting, conducted in February 2006, 12 members participated from 10 institutions. Since then, CISL has held research meetings twice a year and now comprises 130 scholars and 80 clinical research coordinators from 64 institutions. Since 2011, CISL has also run a central office that undertakes administrative work. However, the consortium requires much more funding in order to perform better prospective clinical trials and improve organization. Despite these limitations, CISL has conducted more than 30 retrospective studies to evaluate unique clinical and pathological features of lymphoma subtypes that are more frequent in Korea than in other countries. CISL has also performed more than 30 prospective trials on diffuse large B-cell lymphoma (DLBCL), marginal zone lymphoma (MZL), and extra-nodal NK/T-cell lymphoma (ENNKTCL). As of December 2012, CISL had published 35 articles in internationally renowned, peer-reviewed journals, as well as in the Korean journals, and these will be discussed here.
CISL also collaborates with foreign lymphoma study groups. These include the Groupe d'Etudes des Lymphomes de l'Adulte, which developed the rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) regimen for the treatment of DLBCL; the German High-Grade Non-Hodgkin Lymphoma Study Group, which performed the RICOVER trial on young patients with DLBCL; the International Extranodal Lymphoma Study Group, whose work focuses on extranodal lymphomas; and the Lymphoma Study Group of the Japan Clinical Oncology Group, which is one of the leading lymphoma study groups in Japan and has conducted a DLBCL study with CISL. KLWP holds the Asian Lymphoma Forum annually for the international coordination of CISL activity.
CISL has published several retrospective studies of MZL [4-12] and also published a review article [13]. MZL represents a distinct subgroup of non-Hodgkin lymphoma (NHL), which is typically characterized by an indolent clinical course and long survival times. CISL has shown that MZL comprises 17.3% of NHLs, while mucosa-associated lymphoid tissue lymphoma accounts for 16.7% and nodal MZL accounts for 0.6% of all NHLs. MZL is the second most frequent histologic lymphoma subtype after DLBCL in Korea. Gastric MZL accounts for 50% of all patients with MZL in Korea. In patients with non-gastric MZL, the most commonly involved sites are (in decreasing order of frequency) the orbit and ocular adnexa (48.9%), lymph node and lymphatic organs (17.8%), bowel (9.3%), lungs (6.1%), thyroid (4.9%), and salivary glands (4.5%). In a retrospective multivariate analysis, nodal type compared to extranodal MZL, advanced stage, and poor performance were predictive of poor survival in patients with non-gastric MZL. The clinical features of primary site-specific MZL have been reported for the thyroid, intestine, lungs, and synchronous multiple primary sites involvement.
CISL has carried out retrospective studies on some specific primary sites of DLBCL. Retrospective analysis of primary breast DLBCL suggested that the patient group with one extranodal disease in the breast, compared to those with multiple extranodal diseases, had a different treatment outcome, prognosis, and pattern of progression, and patients with one extranodal disease in the breast should be considered primary breast lymphoma in future trials [14].
CISL also conducted a matched pair analysis of primary breast DLBCL and nodal DLBCL [15]. This report suggested that clinical outcomes of primary breast DLBCL might no longer be worse than those of nodal DLBCL in the rituximab era; however, even when taking rituximab treatment into account, extranodal progressions in the breast or central nervous system (CNS) are problematic.
Intestinal DLBCL was also studied retrospectively [16]. CISL concluded that surgical resection followed by chemotherapy might be an effective treatment strategy with acceptable levels of life quality deterioration for localized intestinal DLBCL.
CISL has also studied primary adrenal DLBCL [17]. We showed that outcomes of primary adrenal DLBCL treated with the R-CHOP regimen are encouraging and that achieving complete response after R-CHOP is predictive of survival. A modified staging system was also suggested.
In a retrospective analysis of 208 patients with ENNKTCL from multiple CISL centers, we suggested that CNS evaluation and prophylaxis do not seem to be necessary in NK prognostic index group I or II patients owing to a very low incidence, despite the fact that ENNKTCL frequently involves the paranasal sinuses [18]. Nevertheless, CNS prophylaxis should be considered as a treatment for patients in NK prognostic index groups III and IV [19]. A multinational retrospective analysis was undertaken to evaluate the clinical features and outcomes of ENNKTCL arising from extranasal sites [20]. We suggested a treatment recommendation according to tumor-node-metastasis stage. Radiotherapy with or without chemotherapy seemed to be optimal in localized disease. In advanced stages, a more aggressive treatment regimen with newer agents should be sought.
For peripheral T-cell lymphoma (PTCL), CISL has reported 2 retrospective studies. In one report, lymphopenia was suggested to be an independent prognostic marker that predicted unfavorable survival in patients with PTCL treated with anthracycline-containing chemotherapy and can be used to further stratify high-risk patients using International Prognostic Index scores [21]. A multinational retrospective study was performed with a focus on non-bacterial infections in patients receiving alemtuzumab. Based on that report, CISL has constructed a guideline for antimicrobial prophylaxis in patients receiving alemtuzumab therapy [22].
Clinical features of some specific sites involved in lymphoma were assessed retrospectively.
A study dealing with ovary involvement showed that treatment outcomes of secondary ovarian involvement in NHL were comparable to those of primary ovarian involvement. We suggested that ovarian involvement itself does not necessarily predict a worse prognosis for patients with NHL [23].
CISL retrospectively analyzed 581 patients from 16 hospitals in Korea for primary intestinal NHL and compared clinical features and treatment outcomes according to the anatomic site of involvement and histologic subtypes. The survival of patients with ileocecal region involvement was better than those with involvement of other sites, which might be related to histologic distribution, tumor stage, and the need for surgical resection [24].
We studied 539 patients with Hodgkin lymphoma from 16 centers in Korea retrospectively, and concluded that, despite the lower incidence in Korea than in Western countries, the distribution of morphological subtypes, treatment outcomes, and patient prognoses were similar [25].
Fifty-five newly diagnosed patients with lymphoblastic lymphoma were analyzed, and CISL concluded that clinical features and treatment outcomes of Korean adult lymphoblastic lymphoma were comparable to previous results, and that the prognosis is still poor, even if treated with intensive chemotherapy [26].
A prospective phase II trial of rituximab with cyclophosphamide, vincristine, and prednisolone (R-CVP) as a first-line treatment for advanced-stage MZL was initiated in 2006 (Fig. 1, CISL 0605) [27]. Between March 2006 and July 2008, 42 patients were enrolled in this trial from 13 institutions. Overall response rate was 87.5% with complete response of 60% and partial response of 27.5%. Toxicity was acceptable, with no treatment-related deaths. The estimated 3-year progression-free survival and overall survival rates were 59.5% and 95.0%, respectively. Although defining the value of rituximab is difficult in a single-arm phase II trial, this study concluded that the R-CVP regimen appears to be effective and well tolerated in patients with advanced-stage MZL. This has led to health insurance re-imbursement of the R-CVP regimen for patients with advanced stage MZL in Korea.
CISL has concurrently conducted a multi-center phase II trial to assess the efficacy and safety of gemcitabine single chemotherapy for patients with MZL in relapse or refractory status (Fig. 1, CISL 0606) [28]. In total, 16 patients were enrolled from 6 institutions. There were 2 cases of partial responses, 9 cases of stable disease, and 1 case of progression. Toxicities were mild and tolerable with no treatment-related deaths. As the response rate in stage I of the trial did not justify progressing to stage II of the trial, this study had to be discontinued in accordance with established protocols. It was suggested that gemcitabine as a single agent showed minimal clinical activity in cases of relapsed or refractory MZL.
In 2006, CISL began a phase I/II study of advanced stage DLBCL (Fig. 1, CISL 0603). The safety and efficacy of bortezomib treatment with dose-dense CHOP every 2 weeks were evaluated. The phase I result recommended a bortezomib dose of 1.6 mg/m2 for phase II. In phase II, the overall response rate was 95% (complete response: 80%; partial response: 15%). Severe sensory neuropathy was the main toxicity in this trial. We concluded that bortezomib plus CHOP-14 is highly effective but, in many cases, dose or schedule modification is required to reduce neurotoxicity [29].
The clinical efficacy and safety of yttrium-90 ibritumomab tiuxetan (Zevalin) consolidation treatment following R-CHOP chemotherapy was investigated in patients with limited-stage and bulky DLBCL (Fig. 1, CISL 0607). This prospective, multi-center, pilot trial included 21 patients, who achieved complete or partial response after 6 cycles of R-CHOP. The overall response rate after Zevalin consolidation treatment was 80.9%, including 4.8% cases of partial response. The 3-year overall and progression-free survival rates were 85% and 75%, respectively. Grade 3-4 adverse events were mainly hematologic toxicities; thus, Zevalin consolidation following 6 cycles of R-CHOP resulted in an acceptable response with tolerable toxicity [30].
CISL conducted a prospective phase II trial for patients with relapsed or refractory DLBCL (Fig. 1, CISL 0802). We investigated a regimen of etoposide, methylprednisolone, high-dose cytarabine, and oxaliplatin (ESHAOx). The overall response rate was 63%, with 33% of participants showing complete response. The most common toxicities were hematologic, and no patient experienced grade 3/4 renal or neurotoxicity. ESHAOx was assumed to be an alternative option for patients with refractory/relapsed DLBCL [31].
Consequently, salvage therapy with gemcitabine, ifosfamide, dexamethasone, and oxaliplatin (GIDOX) for relapsed or refractory DLBCL was tested (Fig. 1, CISL 0702). Twenty-seven eligible patients were recruited and 15% showed a complete response, while 37% showed a partial response. CISL concluded that GIDOX is an active salvage regimen for DLBCL and has acceptable levels of toxicity [32].
A radioimmunotherapy trial was performed for salvage modality in B-cell NHL (Fig. 1, CISL 0602). Radioiodinated rituximab (median dose: 7.3 GBq) was administered in 24 patients, including 11 with DLBCL. The overall response rate was 29%; 46% in patients with low grade B-cell NHL and 9% (one partial response) in patients with DLBCL. Grades 3-4 thrombocytopenia and neutropenia occurred in 33% and 21% of patients with B-cell NHL and DLBCL, respectively. This study concluded that radioimmunotherapy with radioiodinated rituximab seems to be effective and tolerable with modest activity in patients with refractory DLBCL. Further studies are warranted to determine the efficacy of radioiodinated rituximab for treating patients with DLBCL [33].
Based on CISL's 0602 study, CISL conducted a trial of repeated radioimmunotherapy for B-cell NHL (Fig. 1, CISL 1013). Thirty-one patients with relapsed or refractory B-cell NHL, including 7 patients with DLBCL, received radioimmunotherapy repeated at 4-week intervals. A total of 87 cycles were administered and yielded 2-fold increases in response rate (68%) and in median response duration (8.6 months) compared to a single radioimmunotherapy. This regimen induced a favorable response in patients with an aggressive histology compared to that induced by a single treatment [34].
Based on the proven benefits of frontline radiation in early-stage ENNKTCL, CISL conducted a phase II trial of concurrent chemoradiotherapy (CCRT) followed by 3 cycles of etoposide, ifosfamide, cisplatin, and dexamethasone (Fig. 1, CISL 0601). All 30 patients completed CCRT, which resulted in 100% response rate that included 22 complete responses and 8 partial responses. Twenty-six of 30 patients completed the scheduled 3 cycles of chemotherapy. The overall response rate after completion of chemotherapy was 83.3%, with 80% showing complete response. Only 1 patient experienced grade 3 nausea during CCRT, whereas 12 of 29 patients experienced grade 4 neutropenia. The estimated 3-year progression-free and overall survival rates were 85% and 86%, respectively. CISL concluded that patients with newly diagnosed, stages IE to IIE, nasal ENNKTCL are best treated with frontline CCRT [35].
CISL has conducted a phase I trial with bortezomib and CHOP as first-line therapy in advanced, aggressive T-cell lymphoma (Fig. 1, CISL 0701). Patients received increasing doses of bortezomib on days 1 and 8 (weekly schedule: 1.0, 1.3, and 1.6 mg/m2/dose) in addition to CHOP every 3 weeks, and were scheduled for 6 cycles. No dose-limiting non-hematologic toxicity was reported. The maximum-tolerated dose was not reached at 1.6 mg/m2, and the complete response rate was 62%. We concluded that bortezomib can be safely combined with CHOP chemotherapy and constitutes an active regimen for patients with advanced-stage, aggressive T-cell lymphoma. The recommended dose for subsequent phase II studies of bortezomib plus CHOP is 1.6 mg/m2 on days 1 and 8 every 3 weeks as first-line treatment [36].
Based on the results of this phase I study, we consequently performed a phase II trial of bortezomib plus CHOP as the first-line treatment for advanced PTCLs. Forty-six patients were enrolled, and 30 patients (65%) achieved complete response, with an overall response rate of 76%. However, the 3-year overall survival and progression- free survival were 47% and 35%, respectively, owing to frequent relapse after remission. Grade 3/4 leucopenia was the most frequent toxicity, whereas neurotoxicity was tolerable (grade 1 or 2 of peripheral neuropathy). We concluded that bortezomib plus CHOP is an effective and feasible regimen for advanced-stage PTCLs other than ENNKTCL, with acceptable toxicity. However, future studies exploring new drug combinations are warranted to overcome relapse after remission [37].
We designed a salvage regimen combining alemtuzumab with dexamethasone, cisplatin, and cytarabine (DHAP; Fig. 1, CISL 0604). A total of 16 patients with relapsed or refractory PTCL were enrolled, and the overall response rate was 86% for PTCL, unspecified (PTCL-U) which was much higher than 14% in ENNKTCL. Myelosuppression and infectious complications, including cytomegalovirus reactivation were major toxic effects. CISL concluded that alemtuzumab plus DHAP might be an effective salvage chemotherapy regimen for patients with PTCL-U, but that caution is recommended in light of potential infectious complications [38].
CISL has developed a protocol using intravenous busulfan, melphalan, and thiotepa as a conditioning regimen for high-dose therapy in patients with high-risk or relapsed NHL (Fig. 1, CISL 0806). Four out of 5 patients with partial response before ASCT achieved complete response after ASCT, and 10 out of 12 patients achieved or maintained complete response after ASCT. However, grade 3-4 mucositis and liver toxicity occurred in 65%, and venoocclusive disease developed in 46%. We conclude that this regimen is too toxic for our patients [39].
CISL has conducted and reported 13 prospective trials, while 22 retrospective studies have been performed and published (Table 1). CISL is currently undertaking 12 on-going prospective trials, and the flow of CISL studies is summarized in Fig. 1.
CISL intends to continue to focus on lymphoma subtypes relatively common in Korea, namely MZL, ENNKTCL, and PTCL, in addition to DLBCL. Clinical trials for lymphoma require the collaboration of specialists including pathologists, radiologists, radiotherapists, and diagnostic laboratory experts. CISL is trying to create a strong collaborative network with these specialists. We also intend to focus on introducing new drugs and treatment regimens to Korean patients with lymphoma through industry-supported trials or CISL's own studies.
CISL research is currently facing severe challenges. Inappropriately strict regulations and shortages of research funding prevent CISL from performing further clinical trials that could significantly improve survival and quality of life for the Korean patients with lymphoma.
Nevertheless, as a member of the Korean Society of Hematology Working Parties, CISL will strive to continue its work under these difficult circumstances. As its name implies, the KLWP-CISL's core aim is to improve the survival of patients with lymphoma.
CISL, which was established only 7 years ago, had 35 publications by the end of 2012. CISL will endeavor to provide invaluable evidence to improve the clinical course of patients with lymphoma, not only through independent research, but also through collaboration with international lymphoma study groups.
ACKNOWLEDGMENTS
We are grateful to the clinical trial participants for their dedication. We also greatly appreciate the efforts of the CISL members, especially the clinical research coordinators.
References
1. Swerdlow SH, Campo E, Harris NL, editors. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon, France: IARC Press;2008.
2. Jaffe ES, Harris NL, Stein H, Isaacson PG. Classification of lymphoid neoplasms: the microscope as a tool for disease discovery. Blood. 2008; 112:4384–4399. PMID: 19029456.

3. Shankland KR, Armitage JO, Hancock BW. Non-Hodgkin lymphoma. Lancet. 2012; 380:848–857. PMID: 22835603.

4. Oh SY, Ryoo BY, Kim WS, et al. Nodal marginal zone B-cell lymphoma: Analysis of 36 cases. Clinical presentation and treatment outcomes of nodal marginal zone B-cell lymphoma. Ann Hematol. 2006; 85:781–786. PMID: 16847665.

5. Oh SY, Ryoo BY, Kim WS, et al. Nongastric marginal zone B-cell lymphoma: analysis of 247 cases. Am J Hematol. 2007; 82:446–452. PMID: 17266060.

6. Oh SY, Kwon HC, Kim WS, et al. Intestinal marginal zone B-cell lymphoma of MALT type: clinical manifestation and outcome of a rare disease. Eur J Haematol. 2007; 79:287–291. PMID: 17692101.

7. Oh SY, Kwon HC, Kim WS, et al. Nongastric marginal zone B-cell lymphoma: a prognostic model from a retrospective multicenter study. Cancer Lett. 2007; 258:90–97. PMID: 17936499.

8. Oh SY, Kim WS, Kim SJ, et al. Relapsed or refractory nongastric marginal zone B-cell lymphoma: multicenter retrospective analysis of 92 cases. Am J Hematol. 2009; 84:826–829. PMID: 19890833.

9. Oh SY, Kim WS, Kim JS, et al. Multiple mucosa-associated lymphoid tissue organs involving marginal zone B cell lymphoma: organ-specific relationships and the prognostic factors. Consortium for improving survival of lymphoma study. Int J Hematol. 2010; 92:510–517. PMID: 20838958.

10. Oh SY, Kim WS, Kim JS, et al. Pulmonary marginal zone B-cell lymphoma of MALT type--what is a prognostic factor and which is the optimal treatment, operation, or chemotherapy?: Consortium for Improving Survival of Lymphoma (CISL) study. Ann Hematol. 2010; 89:563–568. PMID: 20024551.

11. Oh SY, Kim WS, Kim JS, et al. Stage IV marginal zone B-cell lymphoma--prognostic factors and the role of rituximab: Consortium for Improving Survival of Lymphoma (CISL) study. Cancer Sci. 2010; 101:2443–2447. PMID: 20831770.
12. Oh SY, Kim WS, Kim JS, et al. Primary thyroid marginal zone B-cell lymphoma of the mucosa-associated lymphoid tissue type: clinical manifestation and outcome of a rare disease - consortium for improving survival of lymphoma study. Acta Haematol. 2012; 127:100–104. PMID: 22178776.

13. Oh SY, Suh C. Non-gastric marginal zone B-cell lymphoma in Korea: clinical features, treatment, and prognostic factors. Korean J Intern Med. 2010; 25:227–236. PMID: 20830217.

14. Yhim HY, Kang HJ, Choi YH, et al. Clinical outcomes and prognostic factors in patients with breast diffuse large B cell lymphoma; Consortium for Improving Survival of Lymphoma (CISL) study. BMC Cancer. 2010; 10:321. PMID: 20569446.

15. Yhim HY, Kim JS, Kang HJ, et al. Matched-pair analysis comparing the outcomes of primary breast and nodal diffuse large B-cell lymphoma in patients treated with rituximab plus chemotherapy. Int J Cancer. 2012; 131:235–243. PMID: 21823120.

16. Kim SJ, Kang HJ, Kim JS, et al. Comparison of treatment strategies for patients with intestinal diffuse large B-cell lymphoma: surgical resection followed by chemotherapy versus chemotherapy alone. Blood. 2011; 117:1958–1965. PMID: 21148334.

17. Kim YR, Kim JS, Min YH, et al. Prognostic factors in primary diffuse large B-cell lymphoma of adrenal gland treated with rituximab-CHOP chemotherapy from the Consortium for Improving Survival of Lymphoma (CISL). J Hematol Oncol. 2012; 5:49. PMID: 22889180.

18. Lee J, Suh C, Park YH, et al. Extranodal natural killer T-cell lymphoma, nasal-type: a prognostic model from a retrospective multicenter study. J Clin Oncol. 2006; 24:612–618. PMID: 16380410.

19. Kim SJ, Oh SY, Hong JY, et al. When do we need central nervous system prophylaxis in patients with extranodal NK/T-cell lymphoma, nasal type. Ann Oncol. 2010; 21:1058–1063. PMID: 19850636.

20. Ahn HK, Suh C, Chuang SS, et al. Extranodal natural killer/T-cell lymphoma from skin or soft tissue: suggestion of treatment from multinational retrospective analysis. Ann Oncol. 2012; 23:2703–2707. PMID: 22547542.

21. Kim YR, Kim JS, Kim SJ, et al. Lymphopenia is an important prognostic factor in peripheral T-cell lymphoma (NOS) treated with anthracycline-containing chemotherapy. J Hematol Oncol. 2011; 4:34. PMID: 21843362.

22. Kim SJ, Moon JH, Kim H, et al. Non-bacterial infections in Asian patients treated with alemtuzumab: a retrospective study of the Asian Lymphoma Study Group. Leuk Lymphoma. 2012; 53:1515–1524. PMID: 22273250.

23. Yun J, Kim SJ, Won JH, et al. Clinical features and prognostic relevance of ovarian involvement in non-Hodgkin's lymphoma: A Consortium for Improving Survival of Lymphoma (CISL) report. Leuk Res. 2010; 34:1175–1179. PMID: 20206997.

24. Kim SJ, Choi CW, Mun YC, et al. Multicenter retrospective analysis of 581 patients with primary intestinal non-Hodgkin lymphoma from the Consortium for Improving Survival of Lymphoma (CISL). BMC Cancer. 2011; 11:321. PMID: 21798075.

25. Won YW, Kwon JH, Lee SI, et al. Clinical features and outcomes of Hodgkin’s lymphoma in Korea: Consortium for Improving Survival of Lymphoma (CISL). Ann Hematol. 2012; 91:223–233. PMID: 21789622.

26. Chang MH, Kim SJ, Kim K, et al. Clinical features and treatment outcomes of adult B- and T-lymphoblastic lymphoma: results of multicentre analysis in Korea. Leuk Lymphoma. 2009; 50:1119–1125. PMID: 19557632.

27. Kang HJ, Kim WS, Kim SJ, et al. Phase II trial of rituximab plus CVP combination chemotherapy for advanced stage marginal zone lymphoma as a first-line therapy: Consortium for Improving Survival of Lymphoma (CISL) study. Ann Hematol. 2012; 91:543–551. PMID: 21922208.

28. Oh SY, Kim WS, Lee DH, et al. Phase II study of gemcitabine for treatment of patients with advanced stage marginal zone B-cell lymphoma: Consortium for Improving Survival of Lymphoma (CISL) trial. Invest New Drugs. 2010; 28:171–177. PMID: 19421710.

29. Kim JE, Yoon DH, Jang G, et al. A phase I/II study of bortezomib plus CHOP every 2 weeks (CHOP-14) in patients with advanced-stage diffuse large B-cell lymphomas. Korean J Hematol. 2012; 47:53–59. PMID: 22479278.

30. Yang DH, Kim WS, Kim SJ, et al. Pilot trial of yttrium-90 ibritumomab tiuxetan consolidation following rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone chemotherapy in patients with limited-stage, bulky diffuse large B-cell lymphoma. Leuk Lymphoma. 2012; 53:807–811. PMID: 22035417.

31. Sym SJ, Lee DH, Kang HJ, et al. A multicenter phase II trial of etoposide, methylprednisolone, high-dose cytarabine, and oxaliplatin for patients with primary refractory/relapsed aggressive non-Hodgkin's lymphoma. Cancer Chemother Pharmacol. 2009; 64:27–33. PMID: 18839172.

32. Park BB, Kim WS, Eom HS, et al. Salvage therapy with gemcitabine, ifosfamide, dexamethasone, and oxaliplatin (GIDOX) for B-cell non-Hodgkin's lymphoma: a consortium for improving survival of lymphoma (CISL) trial. Invest New Drugs. 2011; 29:154–160. PMID: 19756371.

33. Kang HJ, Lee SS, Kim KM, et al. Radioimmunotherapy with (131)I-rituximab for patients with relapsed/refractory B-cell non-Hodgkin's lymphoma (NHL). Asia Pac J Clin Oncol. 2011; 7:136–145. PMID: 21585693.

34. Kang HJ, Lee SS, Byun BH, et al. Repeated radioimmunotherapy with 131I-rituximab for patients with low-grade and aggressive relapsed or refractory B cell non-Hodgkin lymphoma. Cancer Chemother Pharmacol. 2013; 71:945–953. PMID: 23370662.

35. Kim SJ, Kim K, Kim BS, et al. Phase II trial of concurrent radiation and weekly cisplatin followed by VIPD chemotherapy in newly diagnosed, stage IE to IIE, nasal, extranodal NK/T-Cell Lymphoma: Consortium for Improving Survival of Lymphoma study. J Clin Oncol. 2009; 27:6027–6032. PMID: 19884539.

36. Lee J, Suh C, Kang HJ, et al. Phase I study of proteasome inhibitor bortezomib plus CHOP in patients with advanced, aggressive T-cell or NK/T-cell lymphoma. Ann Oncol. 2008; 19:2079–2083. PMID: 18689866.

37. Kim SJ, Yoon DH, Kang HJ, et al. Bortezomib in combination with CHOP as first-line treatment for patients with stage III/IV peripheral T-cell lymphomas: a multicentre, single-arm, phase 2 trial. Eur J Cancer. 2012; 48:3223–3231. PMID: 22770877.

38. Kim SJ, Kim K, Kim BS, et al. Alemtuzumab and DHAP (A-DHAP) is effective for relapsed peripheral T-cell lymphoma, unspecified: interim results of a phase II prospective study. Ann Oncol. 2009; 20:390–392. PMID: 19211502.

39. Lee SC, Kim SJ, Lee DH, Kim WS, Suh C, Won JH. Excessive toxicity of once daily i.v. BU, melphalan and thiotepa followed by auto SCT on patients with non-Hodgkin's lymphoma. Bone Marrow Transplant. 2010; 45:801–802. PMID: 19767780.

Fig. 1
Chronological flow of prospective CISL studies. Abbreviations: DLBCL, diffuse large B-cell lymphoma; MCL, mantle cell lymphoma; MZL, marginal zone lymphoma; OAML, ocular adnexa MZL; ENNKTCL, extranodal NK/T cell lymphoma; T-cell, T-cell lymphomas; HL, Hodgkin lymphoma; CNS, central nervous system; ASCT, autologous stem cell transplantation. CISL 0601, concurrent chemo-radiotherapy (CCRT) and weekly cisplatin followed by VIPD (etoposide, ifosfamide, cisplatin, and dexamethasone); CISL 0602, radioimmunotherapy with 131I-rituximab; CISL 0603, bortezomib plus CHOP (cyclophosphamide, adriamycin, vincristine, and prednisolone) every 2 weeks; CISL 0604, alemtuzumab plus and DHAP (dexamethasone, high-dose cytarabine, and cisplatin); CISL 0605, rituximab (R) plus CVP (cyclophosphamide, vincristine, and prednisolone); CISL 0606, gemcitabine single agent; CISL 0607, yttrium-90 ibritumomab tiuxetan consolidation following rituximab plus CHOP; CISL 0701, bortezomib plus CHOP; CISL 0702, GIDOX (gemcitabine, ifosfamide, dexamethasone, and oxaliplatin); CISL 0801, CCRT followed by VIDL (etoposide, ifosfamide, dexamethasone, and L-asparaginase) with risk-based application of ASCT; CISL 0802, ESHAOX (etoposide, methylprednisolone, high-dose cytarabine, and oxaliplatin); CISL 0803, intensified 1st cycle R plus 8 cycles of R-CHOP, CISL 0806 and 0901, busulfan, melphalan, and etoposide as conditioning; CISL 0905, Ox-P (oxaliplatin and prednisolone); CISL 1001, high-dose methotrexate induction followed by alternative high-dose methotrexate and high-dose cytarabine combination consolidation; CISL 1003, GDP (gemcitabine, dexamethasone, and cisplatin); CISL 1004, R augmentation following R-CHOP induction; CISL 1006 and 1107, prospective cohort study with risk-adapted CNS and bone marrow evaluation; CISL 1008, CCRT followed by MIDLE (methotrexate, ifosfamide, dexamethasone, L-asparaginase, and etoposide); CISL 1009, R-CVP followed by R maintenance; CISL 1010, R-CVP; CISL 1011, ESHAOX (etoposide, methylprednisolone, high-dose cytarabine, and oxaliplatin); CISL 1106, R-CHOP and prophylactic intrathecal methotrexate; CISL 1108, everolimus plus CHOP; CISL 1201, vorinostat plus fludarabine, mitoxantrone, and dexamethasone; CISL 1205, comparison intravenous busulfan, melphalan, and etoposide versus intravenous busulfan, cyclophosphamide, and etoposide as conditioning regimen; CISL 1206, R plus reduced dose CHOP for elderly.
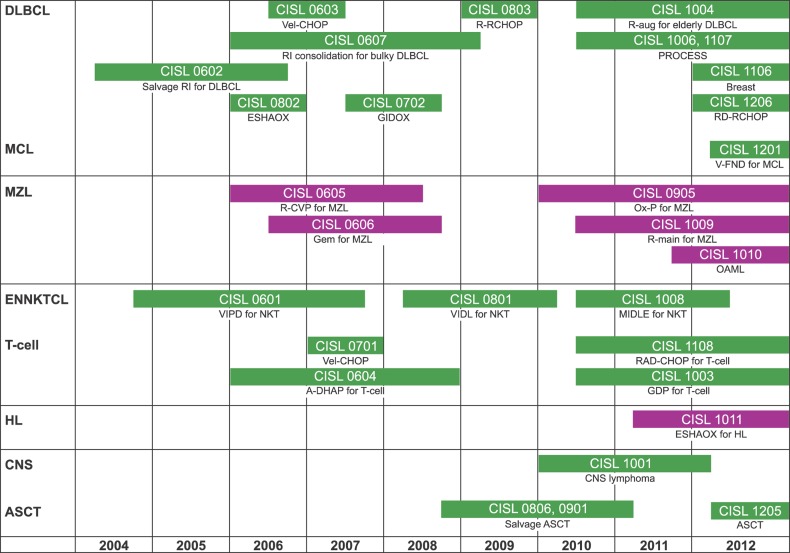
Table 1
Published reports of CISL trials according to lymphoma subtypes and study types.
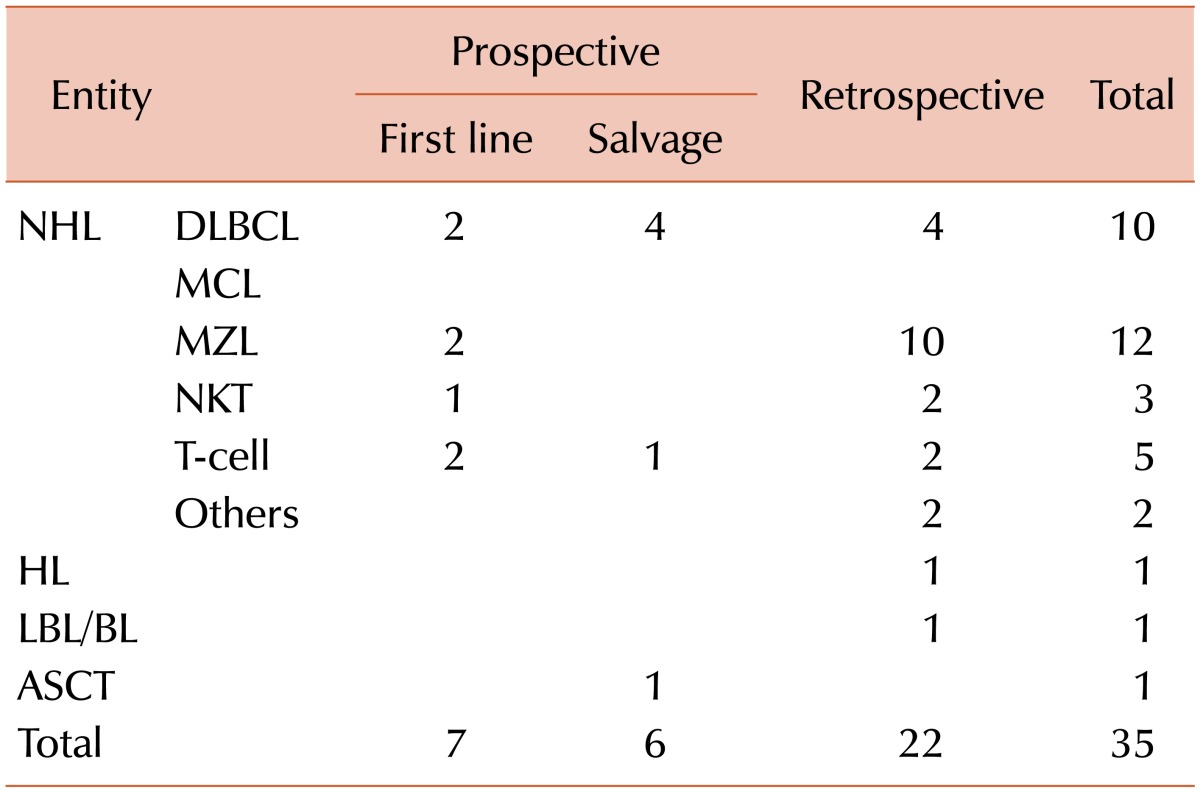
Abbreviations: NHL, non-Hodgkin lymphoma; DLBCL, diffuse large B-cell lymphoma; MCL, mantle cell lymphoma; MZL, marginal zone lymphoma; NKT, extranodal NK/T cell lymphoma; T-cell, T-cell lymphomas; HL, Hodgkin lymphoma; LBL, lymphoblastic lymphoma; BL, Burkitt lymphoma; ASCT, autologous stem cell transplantation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download