Abstract
Background
This study aimed to survey the clinical spectrum of diffuse large B-cell lymphoma (DLBCL) in terms of epidemiology, pathologic subtypes, stage, and prognostic index as well as treatment outcomes.
Methods
In 2007-2008, 13 university hospitals evenly distributed in the Korean peninsula contributed to the online registry of DLBCL at www.lymphoma.or.kr and filed a total of 1,665 cases of DLBCL recorded since 1990.
Results
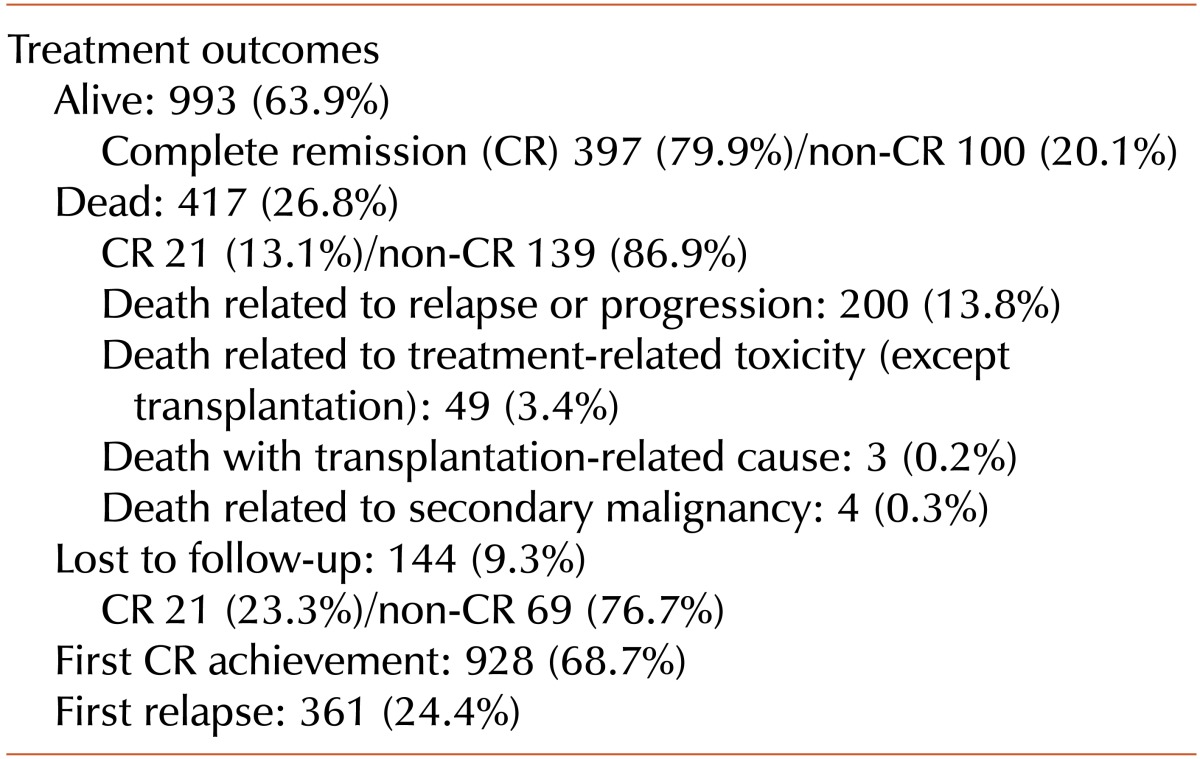
Our analysis showed a higher prevalence of DLBCL in male than in female individuals (M:F=958:707), and extranodal disease was more common than primary nodular disease (53% vs. 47%). Among the 1,544 patients who had been treated with CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) or rituximab-CHOP (R-CHOP) therapy with or without radiation, 993 (63.9%) were alive, with 80% free of disease, 417 were dead (26.8%), with 13% free of disease, and 144 (9.3%) were lost to follow-up, with 23% free of disease. Age below 60 years, stage at diagnosis, international prognostic index (IPI) score regardless of age, and addition of rituximab to CHOP therapy in low- and low-intermediate-risk groups according to IPI scores significantly increased survival duration.
Diffuse large B-cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma (NHL) worldwide, accounting for 30% to 40% of all cases [1, 2]. In addition, in Korea, DLBCL is the most common disease representing 42.6% of malignant lymphomas [3].
Since the anti-CD20 monoclonal antibody, rituximab, was added to the conventional standard chemotherapy CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) regimen, the improvement in treatment outcomes of DLBCL has been proven by large-scale randomized trials and registry data [4-9]. Nonetheless, there have been few nationwide registry data regarding the clinical features of DLBCL in the era of rituximab in Korea or other Asian countries.
The Korean Lymphoma Working Party (KLWP) developed a nationwide web-based registry for DLBCL patients designated as the "Korean lymphoma Registry", which includes data on age, pathologic subtypes, stage, prognostic index as well as treatment regimens, and therapeutic outcomes for each patient. We retrospectively reviewed and analyzed the data of 1,665 Korean DLBCL patients.
The registry committee of the KLWP designed the web-based DLBCL application for the Korean Lymphoma Registry (www.lymphoma.or.kr). The site was open from 2007 through 2008, and 13 university hospitals evenly distributed in the Korean peninsula were involved. During this period, 1,665 cases of DLBCL encountered since 1990 were analyzed by 1 institution. The compiled variables included demographic features, clinical and laboratory disease characteristics, chemotherapy regimens, treatment outcomes, and survival status. The collected clinical and laboratory data at diagnosis included the presence of extra-nodal involvement, DLBCL subtype, complete blood cell counts, chemistry test results, and findings of bone marrow studies. Staging was determined in accordance with the Ann Arbor staging system, and risk groups were defined using the international prognostic index (IPI) and age-adjusted IPI (aaIPI) scoring system. Tumor response was evaluated using the International Working Group Criteria [10].
Fisher's exact test was applied to assess associations between categorical variables. Overall survival (OS) was measured from the date of diagnosis to the date of death or last follow-up and is reported in months. OS was estimated using the Kaplan-Meier method. The log-rank test was used to compare OS among groups. All statistical analyses were performed using a statistical software package (SPSS, Version 17.0 Network version, Inc., Chicago, Ill., USA). Statistical analyses of categorical variables were performed using the chi-square test, and continuous data were compared using linear regression. Two-sided P values of <0.05 were considered statistically significant.
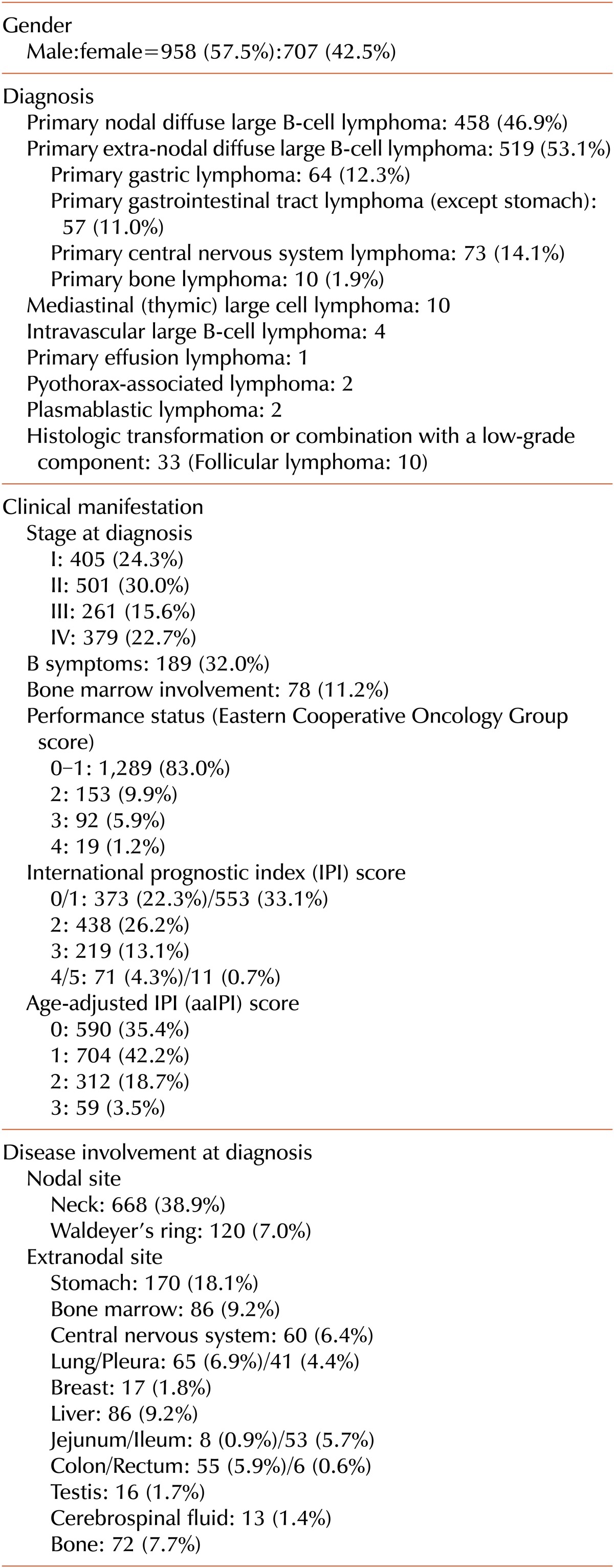
The demographic findings have been summarized at Table 1. The median age at diagnosis was 58 years (range, 1-95 years). Of all patients analyzed, 958 (57.5%) were men and 707 (42.5%) were women. Performance status according to the Eastern Cooperative Oncology Group scale was less than 2 in 1,289 cases (83.0%). In terms of disease site, primary nodal DLBCL was detected in 458 people (46.9%), and extra-nodal DLBCL, in 519 (53.1%); the latter involved the stomach in 64 cases (12.3%), the gastrointestinal tract other than stomach in 57 (11.0%), the central nervous system in 73 (14.1%), and bone in 10 (1.9%). Rare types of DLBCL included mediastinal lymphoma (N=10), intravascular lymphoma (N=4), pyothorax-associated lymphoma (N=2), plasmablastic lymphoma (N=2), and primary effusion lymphoma (N=1). Further, 906 (54.3%) cases were classified as early stage (defined as Ann Arbor stages I, II), and 640 (38.3%), as advanced stage (Ann Arbor stages III, IV). B symptoms were present in 189 patients (32.0%), and tumor deposit in the bone marrow was found in 78 people (11.2%). Grouping according to the IPI score was as follows: 926 (55.4%) patients had a score of 0/1; 438 (26.2%), a score of 2; 219 (13.1%), a score of 3; and 82 (5.0%), a score of 4/5. The aaIPI score was 0 in 590 patients (35.4%), 1 in 704 (42.2%), 2 in 312 (18.7%), 3 in 59 (3.5%). Hepatitis B surface antigen (HBs Ag) was positive in 113 cases (13.9%), anti-hepatitis C antibody (anti-HCV) was positive in 17 (2.1%), and anti-human immunosuppressive antibody (anti-HIV) was positive in 3 (0.4%).
Treatment including CHOP or rituximab-CHOP (R-CHOP) therapy with or without radiotherapy was carried out in 1,544 patients (92.7%), whereas no treatment was administered in 121 cases (7.3%) for various reasons. Among those who were treated, 499 (49.8%) received CHOP, and 502 (50.2%), R-CHOP. After treatment, 499 (49.8%) received CHOP and 502 (50.2%) R-CHOP; 993 (63.9%) were alive in CR status [397 (79.9%)] or not [100 (21.1%)]; 417 (26.8%) died of relapse, 200(13.8%) of refractory disease, and 56 (3.8%) of treatment-related causes; and 144 (9.3%) were lost to follow-up in CR status [21 (23%)] or not [69 (76.7%)]. Complete remission after first-line treatment was achieved in 928 patients (68.7%) (Table 2).
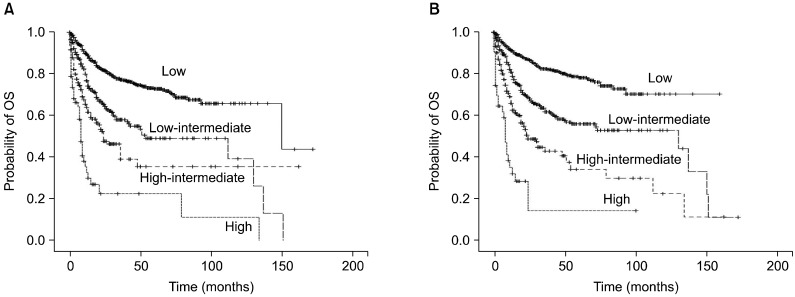
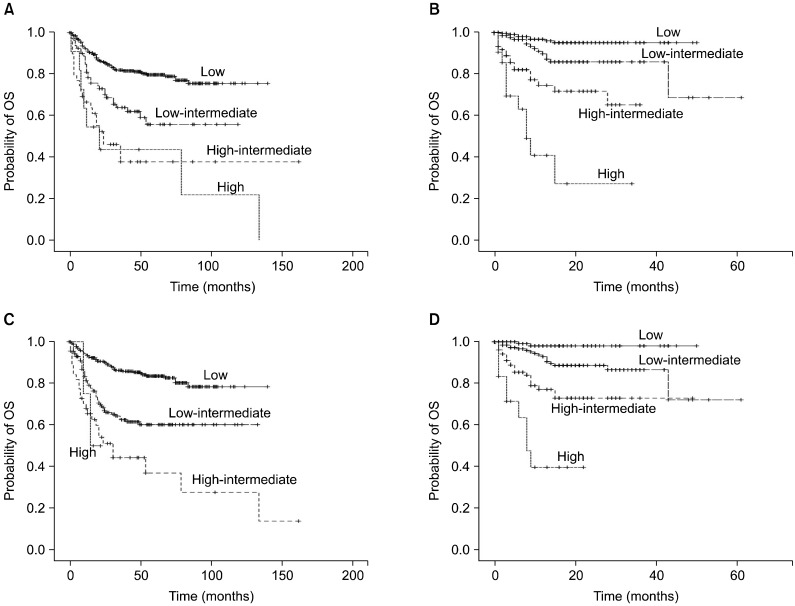
The median follow-up period was 17 months, and the 1-year, 2-year and 5-year OS rates were 80.7%, 71.9%, and 61.2%, respectively. OS was compared according to age (over 60 vs. 60 years or less), IPI score, aaIPI score, and treatment regimen (CHOP vs. R-CHOP). OS was significantly shorter in patients over 60 years (N=933, 55.9%) than in patients aged 60 years or less (N=736, 44.1%; P<0.001). The overall trend of superior OS for R-CHOP compared to CHOP was not significant (P=0.059). On stratification according to each risk group, OS was significantly longer for R-CHOP than for CHOP in low- and low-intermediate-risk groups (P=0.005, P=0.029, respectively), but not in the high-intermediate- and high-risk groups (Fig. 1). The IPI score and aaIPI score had a statistically meaningful impact on survival duration (P<0.001), regardless of the treatment modality (Figs. 2 and 3).
This web-based registry study, which involved 13 hospitals distributed evenly in the Korean peninsula, included the largest number of DLBCL patients among the studies reported in Korea so far and represents the best estimate of the clinical characteristics and outcomes of DLBCL.
We used anti-nuclear antibody (ANA), HBs Ag, anti-HCV, and anti-HIV to investigate if there was any relationship between viral infection and the incidence of DLBCL, as previously reported [11-13]. Of note, we found that the prevalence of HBs Ag positivity was much higher among DLBCL patients than in the general population of Korea surveyed by the national cancer screening program (13.9% vs. 2.57%), suggesting a possible impact of hepatitis B virus infection on the development of DLBCL [12, 14].
The proportion of patients with extra-nodal involvement of DLBCL in this study (58.1%) was similar to that reported by Yang at al. in China (60.1%), which is higher than that in Western countries (30-40%) [15-17]. Higher prevalence of Helicobacter pylori infection in Asian countries might in part contribute to this phenomenon. Further epidemiological studies are required to confirm these results.
The benefit of rituximab on survival in DLBCL patients has been proved by several studies [4-9]. However, in our study, the improvement of OS in the R-CHOP group compared with the CHOP group was not confirmed. Moreover, the difference in OS between each treatment group was only observed in the low- and low-intermediate-risk groups (Fig. 1). This discrepancy between our study and other studies can be explained by the limitations of retrospective studies, such as unmatched number of the patients between treatment groups and short follow-up duration of R-CHOP patients compared to CHOP patients. Furthermore, the survival benefit of rituximab might diminish over time because of the increase in non-lymphoma deaths, as suggested by the long-term results of GELA [9].
The optimal prognostic indices of DLBCL patients have been debated particularly since the introduction of rituximab. Some reports suggested that the revised IPI scoring system was more suitable than the IPI scoring system in patients treated with R-CHOP [18]. In our study, both IPI and aaIPI scoring systems effectively predicted OS in all patients group (Fig. 2). Among the patients treated with R-CHOP, both IPI and aaIPI scores were effective prognostic factors consistent with the result of the study from the Lunenburg Lymphoma Biomarker Consortium, which indicated that these 2 parameters were good prognostic indices for rituximab treatment (Fig. 3B, 3D) [19, 20]. However, neither IPI scores nor aaIPI scores could discriminate between the high-intermediate- and high-risk groups among CHOP-treated patients (Fig. 3A, 3C).
In conclusion, we presented the latest analysis of the epidemiological and clinical characteristics and clinical outcomes of patients with DLBCL in Korea, based on a nationwide web-based registry enlisting the largest number of DLBCL patients reported so far.
References
1. Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood. 2006; 107:265–276. PMID: 16150940.

2. Swerdlow SH, Campo E, Harris NL, editors. WHO Classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon, France: IARC;2008.
3. Kim JM, Ko YH, Lee SS, et al. WHO Classification of malignant lymphomas in Korea: report of the third nationwide study. Korean J Pathol. 2011; 45:254–260.

4. Coiffier B, Lepage E, Briere J, et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med. 2002; 346:235–242. PMID: 11807147.

5. Pfreundschuh M, Trümper L, Osterborg A, et al. CHOP-like chemotherapy plus rituximab versus CHOP-like chemotherapy alone in young patients with good-prognosis diffuse large-B-cell lymphoma: a randomised controlled trial by the MabThera International Trial (MInT) Group. Lancet Oncol. 2006; 7:379–391. PMID: 16648042.
6. Pfreundschuh M, Schubert J, Ziepert M, et al. Six versus eight cycles of bi-weekly CHOP-14 with or without rituximab in elderly patients with aggressive CD20+ B-cell lymphomas: a randomised controlled trial (RICOVER-60). Lancet Oncol. 2008; 9:105–116. PMID: 18226581.
7. Krause SW, Gerken M, Andreesen R, Hofstädter F, Klinkhämmer-Schalke M. Treatment of B cell lymphoma with chemotherapy plus rituximab: a survival benefit can be demonstrated in the routine data of a regional cancer registry. Ann Hematol. 2012; 91:561–570. PMID: 22200972.

8. Cheson BD, Horning SJ, Coiffier B, et al. NCI Sponsored International Working Group. Report of an international workshop to standardize response criteria for non-Hodgkin's lymphomas. J Clin Oncol. 1999; 17:1244. PMID: 10561185.

9. Feugier P, Van Hoof A, Sebban C, et al. Long-term results of the R-CHOP study in the treatment of elderly patients with diffuse large B-cell lymphoma: a study by the Groupe d'Etude des Lymphomes de l'Adulte. J Clin Oncol. 2005; 23:4117–4126. PMID: 15867204.

10. Komrokji RS, Al Ali NH, Beg MS, et al. Outcome of diffuse large B-Cell lymphoma in the United States has improved over time but racial disparities remain: review of SEER data. Clin Lymphoma Myeloma Leuk. 2011; 11:257–260. PMID: 21658652.

11. Guyomard S, Salles G, Coudurier M, et al. Prevalence and pattern of antinuclear autoantibodies in 347 patients with non-Hodgkin's lymphoma. Br J Haematol. 2003; 123:90–99. PMID: 14510947.

12. Kang J, Cho JH, Suh CW, et al. High prevalence of hepatitis B and hepatitis C virus infections in Korean patients with hematopoietic malignancies. Ann Hematol. 2011; 90:159–164. PMID: 20821327.

13. Oh MD, Park SW, Kim HB, et al. Spectrum of opportunistic infections and malignancies in patients with human immunodeficiency virus infection in South Korea. Clin Infect Dis. 1999; 29:1524–1528. PMID: 10585807.

14. Lee EH, Han MA, Lee HY, Jun JK, Choi KS, Park EC. Liver cancer screening in Korea: a report on the 2008 National Cancer Screening Programme. Asian Pac J Cancer Prev. 2010; 11:1305–1310. PMID: 21198282.
15. Møller MB, Pedersen NT, Christensen BE. Diffuse large B-cell lymphoma: clinical implications of extranodal versus nodal presentation--a population-based study of 1575 cases. Br J Haematol. 2004; 124:151–159. PMID: 14687024.
16. López-Guillermo A, Colomo L, Jiménez M, et al. Diffuse large B-cell lymphoma: clinical and biological characterization and outcome according to the nodal or extranodal primary origin. J Clin Oncol. 2005; 23:2797–2804. PMID: 15728226.

17. Yang BY, Yong WB, Zhu J, et al. Clinical characteristics and prognosis of diffuse large B-cell lymphoma. Zhonghua Zhong Liu Za Zhi. 2005; 27:174–176. PMID: 15946571.
18. Sehn LH, Berry B, Chhanabhai M, et al. The revised International Prognostic Index (R-IPI) is a better predictor of outcome than the standard IPI for patients with diffuse large B-cell lymphoma treated with R-CHOP. Blood. 2007; 109:1857–1861. PMID: 17105812.

19. Ziepert M, Hasenclever D, Kuhnt E, et al. Standard international prognostic index remains a valid predictor of outcome for patients with aggressive CD20+ B-cell lymphoma in the rituximab era. J Clin Oncol. 2010; 28:2373–2380. PMID: 20385988.
20. Salles G, de Jong D, Xie W, et al. Prognostic significance of immunohistochemical biomarkers in diffuse large B-cell lymphoma: a study from the Lunenburg Lymphoma Biomarker Consortium. Blood. 2011; 117:7070–7078. PMID: 21536860.

Fig. 1
Comparison of OS in patients treated with CHOP vs. R-CHOP stratified according to risk: low-risk group (A), low-intermediate-risk group (B), high-intermediate-risk group (C), and high-risk group (D).
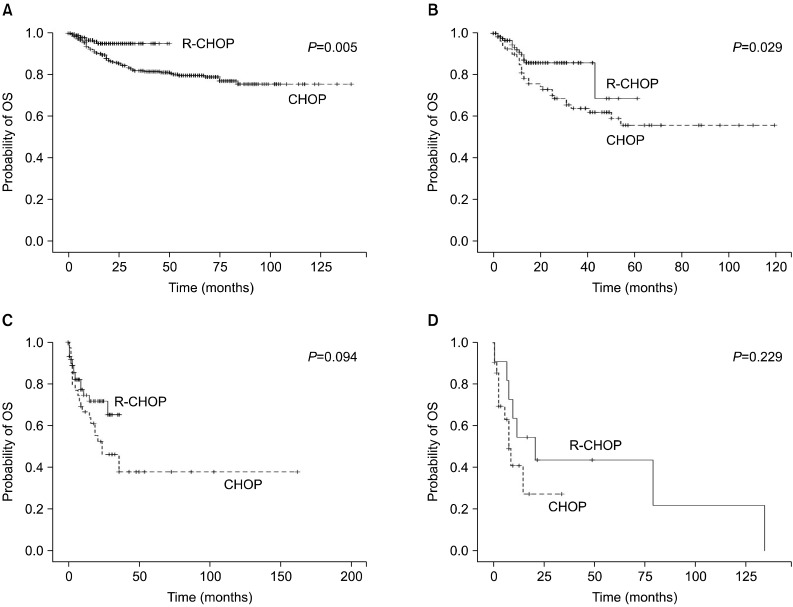
Fig. 2
OS according to IPI (A) and aaIPI (B) scores for all patients. The log-rank P value for both indices was <0.001.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download