This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
The goal of this study was to evaluate the rates of complications, morbidity, and safety with the transparotid approach.
Materials and Methods
A retrospective study was conducted and consisted of 53 surgically treated patients in the past five years for low condylar neck and subcondylar fractures. Only patients with malocclusion and who underwent open reduction with internal fixation with the retromandibular transparotid approach were included. The examined parameters were postoperative suboptimal occlusion, deflection, saliva fistula, and facial nerve weakness.
Results
Fifty-three patients had an open reduction with internal fixation on 55 sides (41 males, 77.4%; mean age, 42 years [range, 18–72 years]). Four patients (7.5%) experienced transient facial nerve weakness of the marginal mandibular branch, but none was permanent. Four patients had a salivary fistula, and 5 patients showed postoperative malocclusion, where one needed repeat surgery after one year. One patient showed long-term deflection. No other complications were observed.
Conclusion
The retromandibular transparotid approach is a safe procedure for open reduction and internal fixation of low condylar neck and subcondylar fractures, and it has minimal complications.
Go to :

Keywords: Maxillofacial surgery, Mandibular fractures, Open fracture reduction, Parotid gland
I. Introduction
Fractures of the subcondylar region and condylar process represent 25% to 35% of mandibular fractures
12. The management of these fractures is still a topic of debate. Many studies have compared closed reduction with maxillomandibular fixation (MMF) and open reduction with internal fixation (ORIF)
3456. Since the early 2000s, endoscopic-assisted reduction with internal fixation (ERIF) has been an alternative for low subcondylar fractures, and many studies have concluded that it achieves the benefits of both open and closed reduction with limited scarring and decreased risk of facial nerve damage
789. In higher subcondylar and low condylar neck fractures, endoscopic treatment is not sufficient, and an open treatment can be indicated. While many relative and absolute indications for open reduction and internal fixation have been proposed, patients are often treated based on the experience and preferences of the surgeon
1011. Open treatment is typically used in patients with bilateral displaced subcondylar fractures with ramus height loss and malocclusion or in patients with concomitant panfacial fractures to restore at least one side of the mandible and to restore height
1112. The advantage of fixation of the proximal fragment on the mandible is the patient's faster return to normal function. Patients with closed treatment (MMF) often suffer malocclusion, mandibular asymmetry, and restricted masticatory function or ankylosis. Disc displacement and malunion or nonunion of the fragment are often observed because the lateral pterygoid muscle tends to displace the proximal segment to the anterior-medial direction
313. Various approaches are possible to treat condylar process and subcondylar region fractures. The retromandibular transparotid approach is commonly used to access the fractured area and is always used in our department of oral and maxillofacial surgery. Possible complications associated with this technique include facial nerve paralysis, salivary fistulae, sialocoele, and Frey syndrome. Other complications in the retromandibular transparotid approach, as well as in other approaches, are postoperative malocclusion, hematoma, wound infection, and potential non-esthetic scarring. In literature, the most important complication is temporary facial nerve damage. Ellis et al.
14, in a prospective study of 93 open treated patients, found that the rate of temporary facial nerve damage was 17.2% at six weeks after surgery, and that all cases had resolved after six months. Other studies have shown similar results, but the number of included patients in those studies rarely exceeded 30
11151617. In our study, we evaluated the complications of 53 patients treated with the retromandibular transparotid approach to fix lower condylar neck and subcondylar fracture.
Go to :

II. Materials and Methods
In this study, we retrospectively examined all medical records of surgically treated patients with maxillofacial fracture in the ETZ Hospitals (Tilburg, The Netherlands) from January 2012 to December 2016. Patients with who underwent the retromandibular transparotid approach for internal fixation with miniplates and screws for low condylar neck and subcondylar fractures were included. Only patients with preoperative posttraumatic malocclusion and a proven fracture on orthopantomogram, computed tomography (CT), or cone beam CT were surgically treated. Edentulous patients were excluded. The examined variables for this study were demographic data, fracture type, postoperative complications such as wound infection, auricular anesthesia, facial nerve palsy, malocclusion, salivary fistulae, deflection of the mandible, plate fracture, and scarring.
The retromandibular transparotid approach was similar to that described by Ellis and Dean
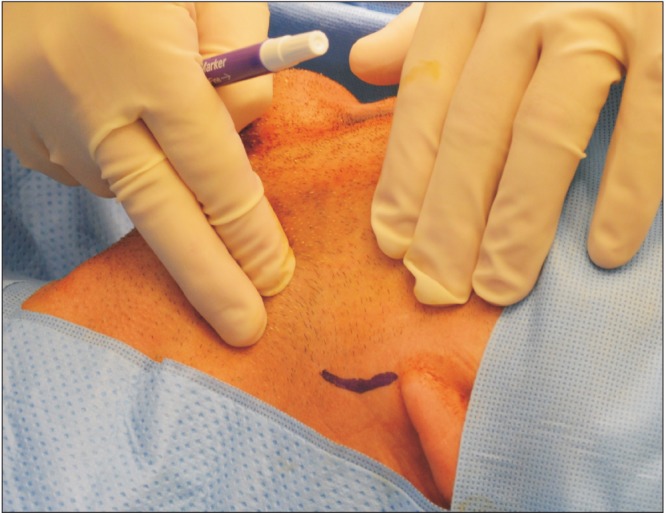
18. The patients were intubated through the nasotracheal route. After disinfecting the patient, a 2 to 3 cm incision line was drawn vertically 5 mm below the ear lobe with a marker, parallel to the posterior border of the mandible.(
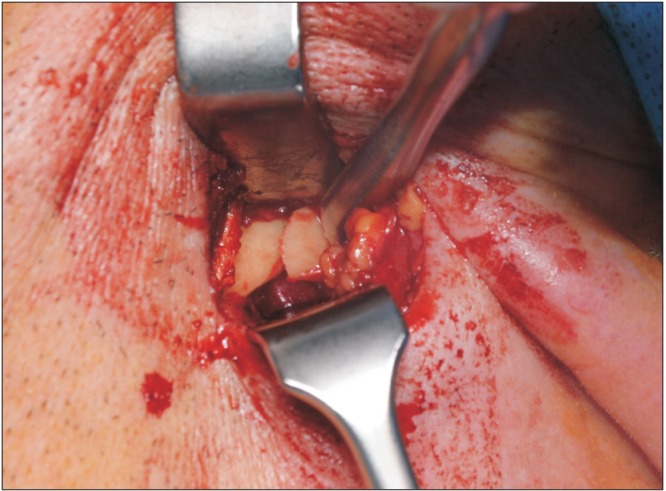
Fig. 1) Then, 1,000 mg of cefazolin was given intravenously 30 minutes before surgery. Surgery was most always performed by a resident along with one of the six staff members of the department. An incision was made through the skin, the subcutaneous fatty tissue, and the superficial muscular aponeurotic system layer, until the parotid capsule was identified and incised. A blunt dissection in the direction of the posterior border mandibular ramus was made through the parotid tissue in the anteromedial direction, parallel to the fibers of the facial nerve to avoid damage, until the masseter muscle was observed. If facial nerve branches were observed, careful dissection of the branches was performed for a short distance, and then they were retracted anteriorly or posteriorly. A nerve stimulator was not used. The masseter muscle and periost were incised at the lateral side of the posterior border of the ramus of the mandible. Exposure of the fracture site was performed by subperiostal dissection. (
Fig. 2) If the proximal fragment was difficult to locate or to align, a towel clamp was placed at the angle of the mandible, and traction was performed to distract the fragment and to allow reduction of the fracture. One 2.0 mm miniplate or two 1.5 mm miniplates were placed to fix the fracture. If the intraoral occlusion was not perfect as an isolated subcondylar fracture without fracture of the body of the mandible, then MMF was performed with four intermaxillary fixation screws, and the lower part of the miniplate was replaced. In patients with more fractures or fractures at the body of the mandible, intermaxillary fixation with screws was always performed. Closure was completed in two layers, with attention paid to closing the parotid capsule with a sealing running suture. No postoperative antibiotics were given. Ibuprofen 600 mg and paracetamol 1,000 mg were prescribed, and a soft diet was recommended for three weeks. If the patient had intermaxillary fixation screws, guiding elastics were placed for a maximum of two weeks, and the screws were removed after three weeks. Physiotherapy was started 3 to 4 weeks postoperatively until normal mouth opening was achieved. The patients were discharged after one day, with a follow-up visit after 1 week, 3 weeks, 3 months, and 12 months. Medical records were notated when late complications were first observed.
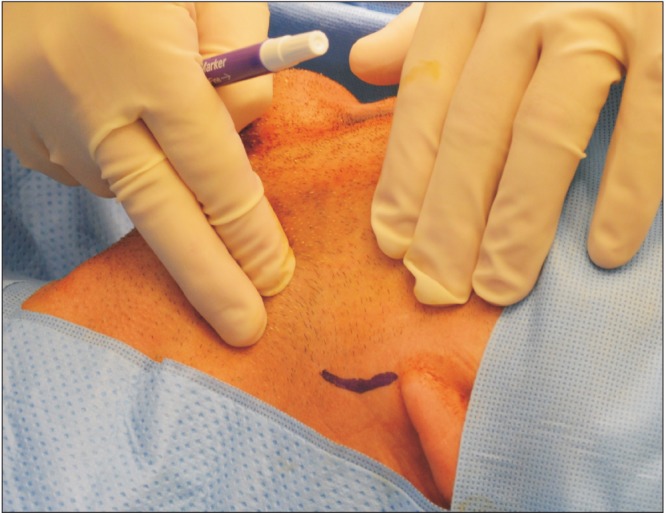 | Fig. 1Vertical incision line of 2 cm, parallel to the posterior border of the mandible.
|
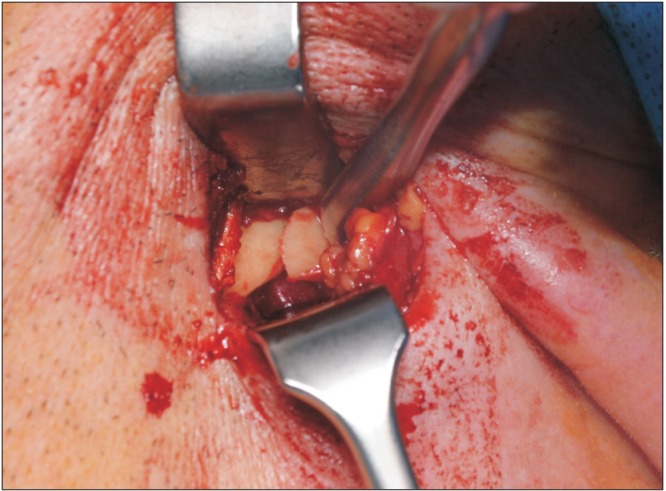 | Fig. 2Exposure of the fracture site by placing the reversed retractor behind the posterior border of the mandible.
|
Go to :

III. Results
Over 5 years, 462 patients were surgically treated in our hospital. Of the 171 patients surgically treated for mandible fracture, 53 patients (31.0%) underwent an open reduction and internal fixation of the subcondylar (37 patients) or low condylar neck (16 patients) region. All patients preoperatively showed malocclusion, with open bite at the contralateral side or frontal open bite in bilateral cases. There were 41 male (77.4%) and 12 female patients (22.6%), with an age range of 18 to 72 years (mean age, 42 years). Thirteen patients had a bilateral subcondylar or condylar process fracture, but only two patients required surgery on both sides. The proximal condylar segment was displaced to the lateral side in 24 operated sites and to the medial side in 22 operated sites. In nine patients, we could not retrospectively assess the side of displacement because the radiological data were no longer available. Fifteen patients (28.3%) presented with an isolated subcondylar fracture, and 38 patients (71.7%) presented with an accompanying fracture of the body of the mandible, which was also restored by open reduction and internal fixation after MMF. The subcondylar fracture was always restored before the body fracture. In 16 cases, two 1.5 mm miniplates were used, and in 39 cases, one 2.0 mm miniplates was used.
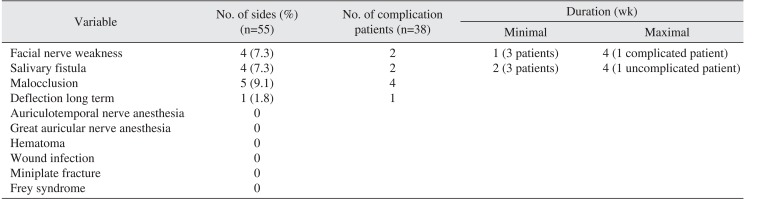
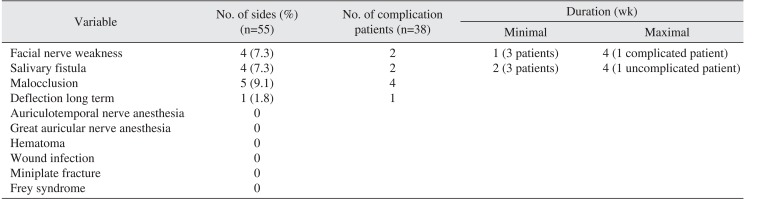
Postoperative malocclusion was found in five patients (9.4%). Four of these patients were also treated for a fracture of the body of the mandible. The malocclusion was resolved in four patients by dental tooth grinding, and proper occlusion was achieved.(
Table 1) One patient continued to have an open bite and underwent bilateral sagittal split osteotomy one year after the trauma. This patient also had a fracture of the body of the mandible and a bilateral low condylar fracture, of which only one side was surgically treated.(
Fig. 3,
4) One patient with bilateral subcondylar fractures with open reduction and internal fixation on one side had a deflection to the non-surgically treated side when opening the jaw. Four temporary salivary fistulae were seen, which resolved in three cases after two weeks and in one case after four weeks of pressure dressings. Of the 55 surgically treated sides, four sides (7.3%) with a subcondylar fracture had temporary weakness of the marginal branch of the facial nerve. One patient regained normal function within four weeks, and three patients had normal function within the first week. There were no cases of anesthesia or paraesthesia of the auriculotemporal and greater auricular nerve, postoperative hematoma, or wound infection. After one year, no cases of miniplate fracture, Frey syndrome, condylar necrosis, trismus, or ankylosis were seen. None of the patients complained about the scar.
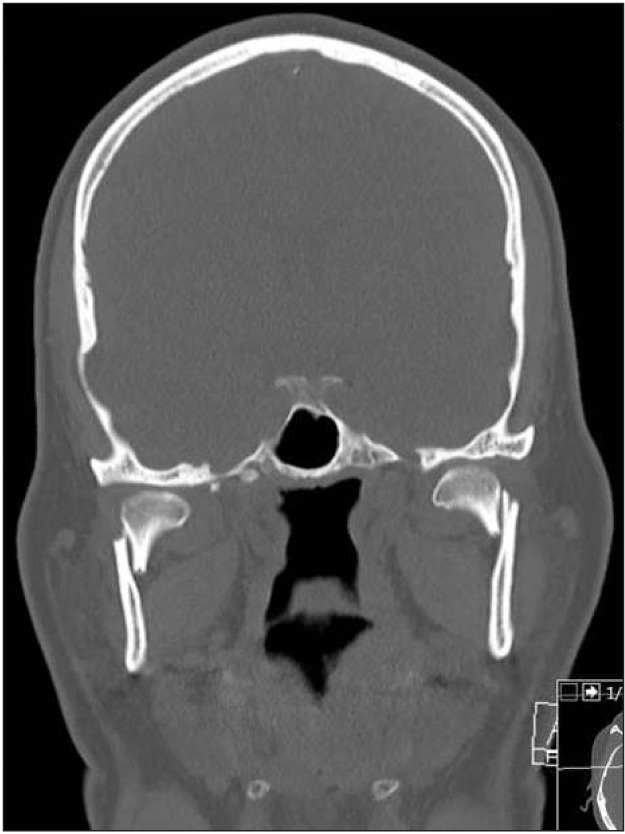
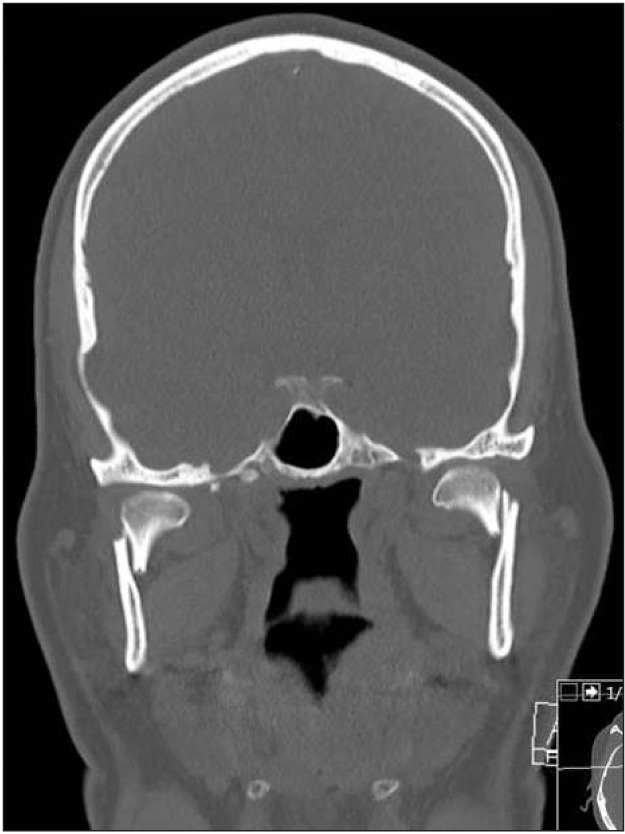 | Fig. 3Preoperative computed tomography image of bilateral subcondylar fracture in patient who needed new intervention one year after fracture management.
|
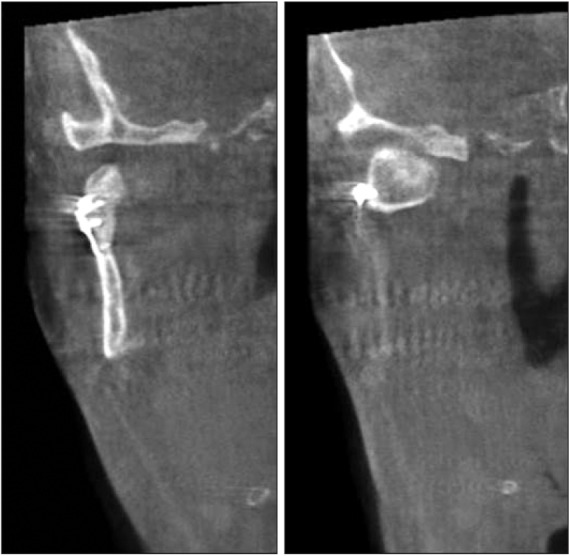
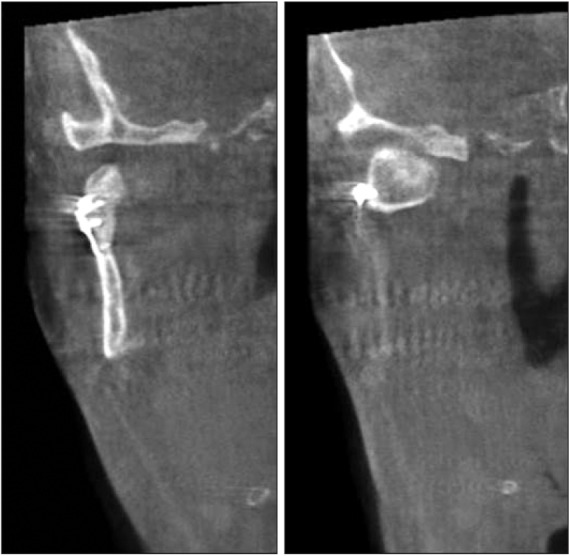 | Fig. 4Postoperative cone-beam computed tomography image of the restored right subcondylar fracture by one 2.0 mm miniplate in the same patient who needed new surgery one year after initial surgery.
|
Table 1
Complications in 55 surgically treated sides in 53 patients
|
Variable |
No. of sides (%) (n=55) |
No. of complication patients (n=38) |
Duration (wk) |
|
Minimal |
Maximal |
|
Facial nerve weakness |
4 (7.3) |
2 |
1 (3 patients) |
4 (1 complicated patient) |
|
Salivary fistula |
4 (7.3) |
2 |
2 (3 patients) |
4 (1 uncomplicated patient) |
|
Malocclusion |
5 (9.1) |
4 |
|
|
|
Deflection long term |
1 (1.8) |
1 |
|
|
|
Auriculotemporal nerve anesthesia |
0 |
|
|
|
|
Great auricular nerve anesthesia |
0 |
|
|
|
|
Hematoma |
0 |
|
|
|
|
Wound infection |
0 |
|
|
|
|
Miniplate fracture |
0 |
|
|
|
|
Frey syndrome |
0 |
|
|
|

Go to :

IV. Discussion
The goal of this study was to examine the complications associated with the retromandibular transparotid approach for low condylar neck and subcondylar fractures from 2012 to 2016. If a patient arrived at the emergency department, both a clinical examination and radiological images (orthopantogram, CT, or cone-beam CT) were essential to decide if the patient required open reduction with internal fixation. Because the ETZ Hospitals of Tilburg are major trauma centers in the southern areas of The Netherlands, and all neurosurgical trauma cases were transported to this hospital, the department of oral and maxillofacial surgery is very experienced with major trauma cases. When ramus shortening and malocclusion were observed, we preferred to use open treatment instead of closed treatment. Also, in bilateral subcondylar fractures with an anterior open bite, we attempted to restore at least one side if possible. Avoiding the closed reduction with MMF helped the patients to regain their function immediately after surgery, which was important for patients with malnutrition, older patients, and those with mental disorders. By restoring the ramus height and fixation of the proximal fractured segment, the chance of developing temporomandibular joint complications was reduced
19. Children were usually treated by closed reduction. In adults, when the fracture could not be restored by the retromandibular transparotid approach, such as in cases with condylar head fracture, we also used closed reduction with MMF. Endoscopic-assisted open reduction and internal fixation were indicated for subcondylar and low subcondylar fractures and left no scar when an angulated drill and fixating system were used
20. Transoral approaches, combined with transbuccal screw placements, resulted in risk facial nerve damage and left small scars because of the trocar placement.
Because the department of oral and maxillofacial surgery is experienced with parotid surgeries, the transparotid approach was familiar and allowed excellent visualization of the fracture site. Since the incision area just below the ear lobe was a certain distance from the ramus of the mandible (
Fig. 1), a few important anatomical structures, such as facial nerve and retromandibular veins, had to be avoided to avoid damage by blunt dissection or traction on the tissues. We, the authors and the other staff members of the department, do not dissect the facial nerve branches unless they are identified and cover a short distance. We use a reversed retractor after the posterior border of the ramus to protect all such structures when the bone is explored.(
Fig. 2) Axonotmesis or neuropraxia can occur when too much traction is applied on the retractor. Only 4 patients (7.5% of treated fracture sites) suffered transient facial nerve palsy of the marginal branch during a maximum of 4 weeks. The incidence of transient facial nerve palsy in literature is 0%, but 30% of these cases resolve within six months
11141516171921. Ellis et al.
14 found a rate of 17.2% transient facial nerve palsy in 93 treated patients with resolution within six months. A possible solution for the reduction of facial nerve damage is the intraoral endoscopic approach, which uses an angled screwdriver or the buccal punch method for plate fixation, especially in cases with lateral displaced fragmentation. In absorbable plate fixation, the intraoral approach with endoscopic view is often used with almost no facial nerve damage and less scarring
2223.
Salivary fistulae were observed in four (7.3%) of the operated sites, in accord with the rates found in the literature
21. To prevent fistulae, a carefully watertight closure of the parotid capsule must be performed. The salivary fistulae in this study occured maximum four weeks and were treated with local prssure dressings until the fistulae disappeared.
Paraesthesia of the distribution areas of the great auricular nerve and the auriculotemporal nerve has been reported, but was not observed in our study
24. Hematoma, Frey syndrome, wound infection, and miniplate fracture were not observed in this study, but have been reported in the literature
13. When the retromandibular transparotid approach was used, antibiotics were given 30 minutes before surgery; when temporary intermaxillary fixation was performed, new and clean gloves were provided before the extraoral incision. An infection rate of 0% to 11.9% was reported in the literature
1114. Some authors preferred two 2.0 mm miniplates to prevent miniplate fractures, but we did not observe any miniplate fractures with the 16 treated fractures with two 1.5 mm miniplates or with the 39 fractures with one 2.0 mm miniplate
19.
In our hospital, we start with reduction of the subcondylar fragment before operating on the body fracture, because we want to work from the sterile extraoral site to the less sterile intraoral region. Postoperative malocclusion was seen in five patients (9.4%), four of whom also had a concomitant fracture of the body of the mandible. Proper occlusion was achieved in four of the five patients via dental tooth grinding. One patient with a fracture of the body of the mandible and bilateral low condylar fracture and in whom only one side was surgically treated needed repeat surgery one year after the initial open reduction with internal fixation because of insufficient occlusion and a frontal open bite. On the postoperative CT, we did not observe good alignment of the fragments, and the proximal fragment was angled to the medial side.(
Fig. 4) Yang and Patil
13 reported 8.5% malocclusion in patients who also suffered multiple mandibular fractures. One patient with bilateral subcondylar fracture with open reduction and internal fixation on one side still showed deflection to the contralateral side when opening the jaw after one year, in accord with data in the literature
13.
Go to :

V. Conclusion
The weaknesses of this study were the retrospective design with limited patients (53 patients) and six different surgeons. However, we concluded that retromandibular transparotid open reduction with internal fixation of low condylar neck and subcondylar fractures provides good access and is a safe procedure with minimal complications.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download