Abstract
Objectives
Foreign bodies (FBs) account for 3.8% of all pathologies of the head and neck region, and approximately one third of them are missed on initial examination. Thus, FBs represent diagnostic challenges to maxillofacial surgeons, rendering it necessary to employ an appropriate imaging modality in suspected cases.
Materials and Methods
In this cross-sectional study, five different materials, including wood, metal, glass, tooth and stone, were prepared in three sizes (0.5, 1, and 2 mm) and placed in three locations (soft tissue, air-filled space and bone surface) within a sheep's head (one day after death) and scanned by panoramic radiography, cone-beam computed tomography (CBCT), and ultrasonography (US) devices. The images were reviewed, and accuracy of the detection modalities was recorded. The data were analyzed statistically using the Kruskal-Wallis, Mann-Whitney U-test, Friedman, Wilcoxon signed-rank and kappa tests (P<0.05).
Results
CBCT was more accurate in detection of FBs than panoramic radiography and US (P<0.001). Metal was the most visible FB in all of modalities. US was the most accurate technique for detecting wooden materials, and CBCT was the best modality for detecting all other materials, regardless of size or location (P<0.05). The detection accuracy of US was greater in soft tissue, while both CBCT and panoramic radiography had minimal accuracy in detection of FBs in soft tissue.
The maxillofacial region is a complex anatomical area containing the external openings of the respiratory and digestive systems along with the orbital cavities. While it is a relatively small area, the prevalence of penetrating injuries at this site is known to be similar to that of larger regions of the body1.
Foreign bodies (FBs) are defined as any object originating from outside of the body. The prevalence of FB injuries in the head and neck region is estimated to be 3.8% of all pathologies in this region2. The most commonly retained objects are wood splinters, glass fragments and metallic objects3. Approximately one-third of all the FBs are missed during initial clinical and radiographic examinations4, and this can lead to significant complications. They might become irritated, causing inflammation, infection, abscess formation, pain, swelling, migration of the FB and potential injury to vessels or nerves. Furthermore, inflammatory reactions and granuloma formation might impair wound healing. FBs can also cause serious complications such as intracranial abscesses. To avoid complications, FBs must be detected and removed as soon as possible2567. Identification and localization of FBs is based on the patient's history and clinical and radiographic examinations89.
Conventional plain radiographs, computed tomography (CT), cone-beam computed tomography (CBCT), ultrasonography (US), and magnetic resonance imaging (MRI) are used routinely in trauma settings for detecting and localizing FBs210.
Conventional plain radiographs or panoramic radiographs are usually the initial imaging techniques for detection of FBs24911. They were successful in the diagnosis of radiopaque FBs in soft tissue11, but non-radiopaque objects cannot be detected by these techniques. Superimposition of tissues is also a limitation of 2D imaging2. Because of its multi-planar scans and high contrast technique, CT is the gold standard for detecting FBs912; however, metal artifacts can interfere with CT's detection abilities2. CBCT has advantages over CT, like lower radiation doses and greatly reduced size and cost13. US is an inexpensive, widely accessible, realtime imaging modality with no radiation exposure71012. It is helpful in the detection of suspected non-radiopaque FBs, especially in superficial tissues211. Intraoral US utilizes a high frequency probe that allows for high spatial resolution13.
The present study was undertaken to compare the accuracy of special imaging techniques available in dental settings, including panoramic radiography, CBCT, and intraoral US, in detection of different FBs.
This study was carried out in Department of Radiology, School of Dentistry, Isfahan University of Medical Science (Isfahan, Iran) from January to March 2017.
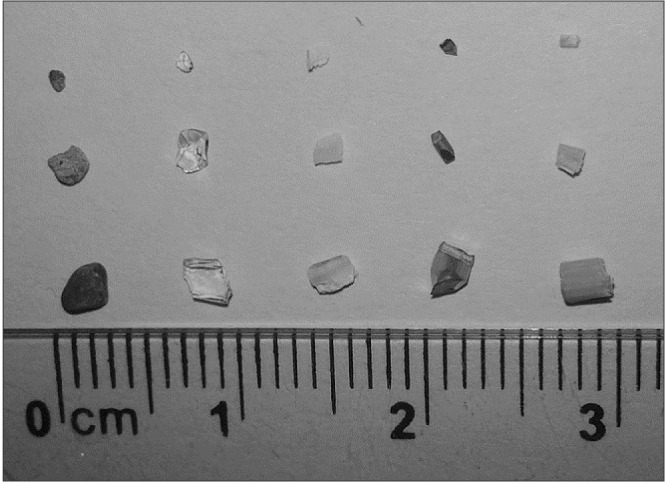
In this in vitro study, two fresh sheep's heads (one day after death) were used. First, an initial scan of the two heads was carried out to rule out the existence of any FBs or anomalies. The following five different materials, known to be common FBs in head and neck traumas, were selected: wood (dry toothpick), metal (iron), glass, tooth (both enamel and dentin), and stone (small pebbles).(Fig. 1) The materials were prepared in three sizes (0.5, 1, and 2 mm) and placed in three different locations (soft tissue, an air-filled space, and bone surface). Placement techniques are outlined as follows:
The materials were placed in the sheep's lower lip bilaterally. Incisions measuring 5 mm in width and depth on the left and right sides of the lower lip were made using a scalpel.
After placing the FBs in the six locations of the sheep's head randomly, they were scanned by three imaging devices (panoramic radiography, CBCT, and US) simultaneously.
The panoramic views were scanned by a Papaya (Genoray, Seongnam, Korea) device with exposure settings of 65 kVp, 7 mA, and 12 seconds.
The utilized CBCT device was a GALILEOS Comfort (Sirona, Bensheim, Germany) with settings of 85 kVp, 35 mA, large field of view (15×15 cm), and Vol 1 HC (high resolution and high contrast).
The US machine was a ECUBE7 (Alpinion, Seoul, Korea) device with a frequency of 3 to 12 MHz and a linear intraoral probe (18 mm footprint). This modality could not be used for air-filled spaces.
Ultimately, 16 images from each modality were obtained. (Fig. 2) The images were analyzed by three interpreters (one oral and maxillofacial radiologist, one postgraduate oral and maxillofacial radiology student and one postgraduate oral and maxillofacial surgery student). The observers were well trained and calibrated. A four-point scoring scale ranging from 0 to +4 was used for evaluating accuracy of the modalities for detecting FBs10.(Table 1)
The inter- and intra-examiner agreement was excellent (Cohen' kappa coefficient of 0.76–0.88), and thus, the average of the results was recorded for data analysis.(Table 2)
By using Friedman and Wilcoxon signed-rank tests, the difference in FB detection accuracy of the three modalities was statistically significant (P<0.001), revealing that CBCT was better than US and panoramic radiography (P<0.001). US was more accurate than panoramic radiography, but the difference was not significant (P=0.165).
The effect of FB composition, size and location on detection accuracy was evaluated using the Kruskal-Wallis test. CBCT and panoramic radiograph accuracy were significantly affected by the composition of the FBs (P<0.001 and P=0.009, respectively). US was significantly affected by the size and location of the FBs (P<0.001).
The accuracy of the three FB detection modalities is demonstrated in Fig. 3. Accuracy was significantly different between the three modalities for all types of FBs. For wooden materials, US was more accurate than CBCT and panoramic radiography (P=0.005 and P=0.004, respectively). For other materials, CBCT was the best detection modality (P<0.05). Metal was the most visible FB in all modalities.
Panoramic radiography was significantly more accurate for detecting metal than for detecting any other material (P<0.001). Detection accuracy for wooden FBs in CBCT was significantly lower than for other materials (P<0.001).
The detection accuracy of the modalities based on FB size is shown in Fig. 4. There was a significant difference between the accuracy of the three techniques for all sizes of FBs. CBCT was significantly more accurate for detecting all three sizes of materials (P<0.05).
The accuracy of all modalities increased with an increasing FB size, but this increase was statistically significant only for US (P<0.05).
The detection accuracy of the three techniques based on FB location is demonstrated in Fig. 5. The difference in detection accuracy between the three modalities was significant for all the three locations. CBCT was the most accurate modality for each location. US was significantly better than panoramic radiography in soft tissue (P=0.001), while panoramic radiography was more accurate than US at the bone surface. However, this difference was not statistically significant (P=0.071).
The highest FB detection accuracy was in the air-filled space for panoramic radiography, at the bone surface for CBCT and in soft tissue for US. Both CBCT and panoramic radiography exhibited the least accuracy in detection of FBs in soft tissue. The differences were statistically significant only for US (P<0.001).
Oral and maxillofacial surgeons frequently encounter FBs7. The ability of FB detection depends on the size and composition of the FB, its environment and the method of imaging6. Each imaging technique has specific restrictions, and an object that may not be visible using a certain imaging technique, might be detectable on other images. For example, US cannot be used for objects adjacent to air or behind bony structures911.
In recent years, some studies have evaluated and compared the accuracy of FB detection for the most commonly used modalities in the trauma settings including conventional plain radiography, CT, MRI, and US2357891011141516. However, none of these studies has compared the special modalities used in dental clinics. Panoramic radiography has not been evaluated in any study, and CBCT has been evaluated in only a few 269.
Thus, we decided to compare the accuracy of panoramic radiography, CBCT and intraoral US in the detection of FBs, while assessing the effect of FB composition, size and location on their visibility.
In this study, three imaging modalities (panoramic radiography, CBCT, and US) were evaluated and compared. Panoramic radiography and CBCT are based on x-ray, and US is based on ultrasound waves. CBCT was the most accurate technique for detection of FBs, while US was better than the panoramic technique. Only two studies have assessed CBCT, and they compared this technique with CT scan. Valizadeh et al.2 recommended US as the first choice imaging modality for suspected FBs located in the superficial soft tissues. They recommended CBCT and then CT for FBs penetrating into deeper tissues or beneath bone. In the study by Kaviani et al.9, CBCT scan by NewTom was a more effective technique for visualizing radiopaque FBs in air, compared to conventional CT. Both CT and CBCT can detect even the smallest FBs (0.5 mm) in muscle tissue and adjacent to bone.
CBCT has higher spatial and contrast resolution than panoramic radiography because of the small voxel size (about 0.3 mm) and wide gray scale (12-bit)17. The three-dimensional images of CBCT can also improve its ability to detect and localize FBs better than the panoramic technique18. The panoramic technique has a single image layer (focal trough), and objects out of this trough are blurred and cannot be visualized. US's ability to detect FBs is affected by the acoustic impedance of the object, the depth at which it is located, and the surrounding tissues (objects in the air-filled areas and behind the bone cannot be detected by US)213. Of note, the penetration depth of the high frequency US device we used is lower than that of lower frequency devices.
We compared five different materials, including wood, metal, tooth, glass and stone. For wooden materials, US was the most accurate technique, while the other materials were best seen on CBCT. Metal was the most visible FB in all three modalities. In a study by Aras et al.3, conventional radiography, CT, and US techniques best detected metal materials. Wood was invisible on conventional radiography and had the least visibility in CBCT, while US had good accuracy in detecting wooden materials, as also found in our study. In the study by Kaviani et al.9, both CBCT devices exhibited good accuracy in detecting high-density materials (metal, glass, stone, and tooth), but the detection accuracy for wooden materials was lowest with both CBCT devices. Javadrashid et al.10 concluded that CT and conventional radiography have the highest accuracy for metallic objects and good accuracy for tooth, stone and glass materials. However, wood was invisible with both modalities. US exhibited the highest accuracy for wooden objects and was acceptable for the other materials.
The visibility of FBs on x-ray–based devices depends on the radiodensity of the materials. The higher the density, the higher the attenuation of the x-ray beam and the better the differentiation from surrounding structures18. According to previous studies, metal has the highest radiopacity, and wooden materials are radiolucent16192021. Contrast resolution is the ability to distinguish anatomical structures of objects with similar contrast22. The radiodensity of wooden materials is similar to that of muscles and soft tissue, and thus, contrast resolution is important for detection accuracy of x-ray–based devices15. The contrast resolution of CBCT is lower than that of CT because of greater scatter radiation13.
US can image objects that have different acoustic impedance compared to surrounding tissues due to echo production at their interfaces13. Therefore, it does not have the limitation of x-ray devices in detecting low-density objects.
In this study, FBs were prepared in three sizes (0.5, 1, and 2 mm). Detection accuracy of all imaging modalities increased with an increasing the size of the materials. CBCT was significantly the most accurate modality for detection of all the three sizes of the materials. Materials 0.5 mm in size were least visible on US, and the largest materials had the lowest visibility on panoramic radiography. Kaviani et al.9 showed that two CBCT devices can detect metal, stone, glass and tooth fragments in all the locations at the smallest sizes (0.5 mm), except for 0.5 mm tooth fragments at the bone surface. Wooden objects were not visible with either device except in air-filled spaces with sizes larger than 0.5 mm.
An important factor that determines the ability of any imaging modality to visualize smaller sized objects is spatial resolution. Spatial resolution refers to the ability to image small objects that have high subject contrast22. CBCT has higher spatial resolution than even CT because of lower voxel size9. US with an intraoral probe is high-frequency and therefore has higher spatial-resolution compared to conventional US13.
In the present study, FBs were placed in three locations of sheep's heads (bone surface, soft tissue, and air-filled space). CBCT was the most accurate modality for all the three locations. US was better than panoramic radiography in soft tissues, and panoramic radiography was more accurate than US at the bone surface. The panoramic technique had the highest FB detection accuracy in air-filled space, while accuracy was greatest at the bone surface for CBCT and in soft tissue for US. Both CBCT and panoramic radiography had the lowest accuracy for detecting FBs in soft tissue. Valizadeh et al.2 showed that the accuracy of CBCT and CT was not statistically affected by the location of FBs but that US was able to visualize objects in superficial tissues and unable to detect deeper FBs and objects beneath bone. In the study by Kaviani et al.9, the detection accuracy of the two CBCT devices as not affected by the location of radiopaque objects, but non-radiopaque materials were affected by the surrounding structures to a higher degree. In the study by Javadrashid et al.10, CT had the highest detection accuracy in all three locations, which is reflected by CBCT in our study. US was more accurate than conventional radiography in soft tissues, and conventional radiography was better than US at the bone surface. These results were consistent with the present study.
The prioritization of US in detection of FBs in soft tissue rather than on the bone surface is probably due to the lower penetration of ultrasound waves into tissues13. The lower accuracy of CBCT and panoramic techniques in the detection of FBs in soft tissues demonstrates that the average density of the materials was closer to the density of soft tissues rather than that of bone or air.
Future studies can evaluate these modalities in real patients. In addition, the measurement of the density and the acoustic impedance of FBs and the surrounding tissues can allow for better interpretation of results. In addition, the effect of the depth of FBs on detection accuracy can be assessed.
CBCT was the most accurate modality in detection of all the sizes, locations and compositions of FBs, except for wooden materials. US more accurately visualized wooden FBs. Therefore, we recommended CBCT as the gold standard for imaging in the detection of FBs. US is recommended when the suspected FB is not visible on initial imaging, especially in superficial tissues and for radiolucent FBs.
Notes
Authors' Contributions: All authors participated in data collection and the study design. S.S. place the foreign bodies. All authors observed the images. M. Aminian wrote the manuscript and M. Abdinian edited it. S.S. helped to draft the manuscript. All authors read and approved the final manuscript.
References
1. Reginelli A, Santagata M, Urraro F, Somma F, Izzo A, Cappabianca S, et al. Foreign bodies in the maxillofacial region: assessment with multidetector computed tomography. Semin Ultrasound CT MR. 2015; 36:2–7. PMID: 25639172.

2. Valizadeh S, Pouraliakbar H, Kiani L, Safi Y, Alibakhshi L. Evaluation of visibility of foreign bodies in the maxillofacial region: comparison of computed tomography, cone beam computed tomography, ultrasound and magnetic resonance imaging. Iran J Radiol. 2016; 13:e37265. PMID: 27895878.

3. Aras MH, Miloglu O, Barutcugil C, Kantarci M, Ozcan E, Harorli A. Comparison of the sensitivity for detecting foreign bodies among conventional plain radiography, computed tomography and ultrasonography. Dentomaxillofac Radiol. 2010; 39:72–78. PMID: 20100917.

4. Omezli MM, Torul D, Sivrikaya EC. The prevalence of foreign bodies in jaw bones on panoramic radiography. Indian J Dent. 2015; 6:185–189. PMID: 26752878.

5. Ober CP, Jones JC, Larson MM, Lanz OI, Werre SR. Comparison of ultrasound, computed tomography, and magnetic resonance imaging in detection of acute wooden foreign bodies in the canine manus. Vet Radiol Ultrasound. 2008; 49:411–418. PMID: 18833946.

6. Eggers G, Mukhamadiev D, Hassfeld S. Detection of foreign bodies of the head with digital volume tomography. Dentomaxillofac Radiol. 2005; 34:74–79. PMID: 15829688.

7. Haghnegahdar A, Shakibafard A, Khosravifard N. Comparison between computed tomography and ultrasonography in detecting foreign bodies regarding their composition and depth: an in vitro study. J Dent (Shiraz). 2016; 17:177–184. PMID: 27602392.
8. Oikarinen KS, Nieminen TM, Mäkäräinen H, Pyhtinen J. Visibility of foreign bodies in soft tissue in plain radiographs, computed tomography, magnetic resonance imaging, and ultrasound. An in vitro study. Int J Oral Maxillofac Surg. 1993; 22:119–124. PMID: 8320449.
9. Kaviani F, Javad Rashid R, Shahmoradi Z, Gholamian M. Detection of foreign bodies by spiral computed tomography and cone beam computed tomography in maxillofacial regions. J Dent Res Dent Clin Dent Prospects. 2014; 8:166–171. PMID: 25346836.
10. Javadrashid R, Fouladi DF, Golamian M, Hajalioghli P, Daghighi MH, Shahmorady Z, et al. Visibility of different foreign bodies in the maxillofacial region using plain radiography, CT, MRI and ultrasonography: an in vitro study. Dentomaxillofac Radiol. 2015; 44:20140229. PMID: 25426703.
11. Gomaa M, Abdelaal A. Ultrasonography versus radiography in detection of different foreign bodies in a cadaveric calf thigh specimen. Res J Vet Pract. 2015; 3:83–88.

12. Holmes PJ, Miller JR, Gutta R, Louis PJ. Intraoperative imaging techniques: a guide to retrieval of foreign bodies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 100:614–618. PMID: 16243249.

13. White SC, Pharaoh MJ. Oral radiology, principles and interpretations. St. Louis: Mosby;2014. p. 111–220.
14. Javadrashid R, Golamian M, Shahrzad M, Hajalioghli P, Shahmorady Z, Fouladi DF, et al. Visibility of different intraorbital foreign bodies using plain radiography, computed tomography, magnetic resonance imaging, and cone-beam computed tomography: an in vitro study. Can Assoc Radiol J. 2017; 68:194–201. PMID: 26899378.

15. Ginsburg MJ, Ellis GL, Flom LL. Detection of soft-tissue foreign bodies by plain radiography, xerography, computed tomography, and ultrasonography. Ann Emerg Med. 1990; 19:701–703. PMID: 2188542.

16. Roobottom CA, Weston MJ. The detection of foreign bodies in soft tissue--comparison of conventional and digital radiography. Clin Radiol. 1994; 49:330–332. PMID: 8013198.

17. Ganguly R, Ruprecht A, Vincent S, Hellstein J, Timmons S, Qian F. Accuracy of linear measurement in the Galileos cone beam computed tomography under simulated clinical conditions. Dentomaxillofac Radiol. 2011; 40:299–305. PMID: 21697155.

18. Lari SS, Shokri A, Hosseinipanah SM, Rostami S, Sabounchi SS. Comparative sensitivity assessment of cone beam computed tomography and digital radiography for detecting foreign bodies. J Contemp Dent Pract. 2016; 17:224–229. PMID: 27207202.
19. Anderson MA, Newmeyer WL 3rd, Kilgore ES Jr. Diagnosis and treatment of retained foreign bodies in the hand. Am J Surg. 1982; 144:63–67. PMID: 7091533.

20. Krimmel M, Cornelius CP, Stojadinovic S, Hoffmann J, Reinert S. Wooden foreign bodies in facial injury: a radiological pitfall. Int J Oral Maxillofac Surg. 2001; 30:445–447. PMID: 11720049.

21. Specht CS, Varga JH, Jalali MM, Edelstein JP. Orbitocranial wooden foreign body diagnosed by magnetic resonance imaging. Dry wood can be isodense with air and orbital fat by computed tomography. Surv Ophthalmol. 1992; 36:341–344. PMID: 1566235.

22. Bushong SC. Radiologic science for technologists: physics, biology, and protection. St. Louis: Elsevier Mosby;2013.
Fig. 2
A. Panoramic radiography view of 2 mm metal (left) and 2 mm stone (right) on bone surface. B. Cone-beam computed tomography sagittal view of 2 mm metal in air-filled space (upper arrow) and 1 mm tooth fragment in soft tissue (lower arrow). C. Ultrasonography view of 2 mm wood in soft tissue (arrow).
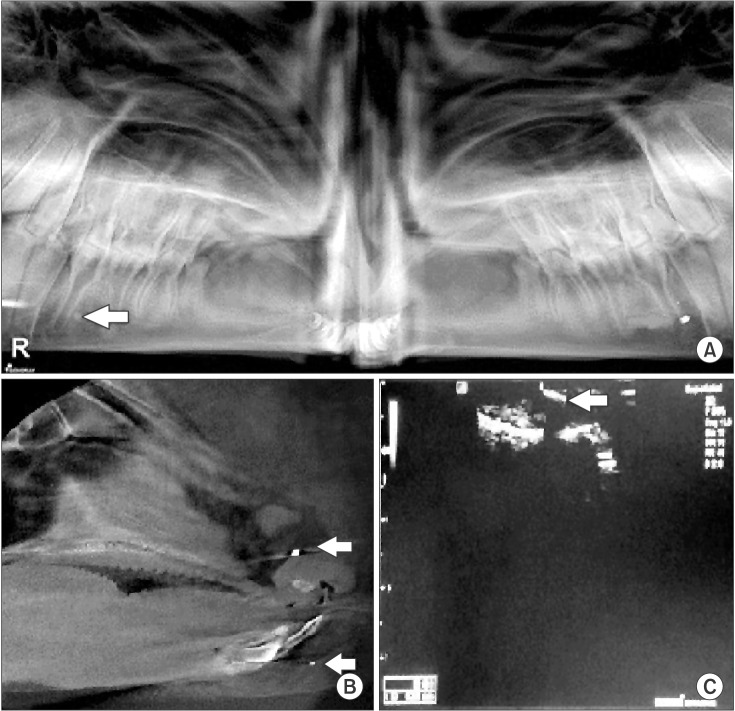
Fig. 3
Detection accuracy of panoramic radiography, cone-beam computed tomography (CBCT) and ultrasonography (US) for different type of foreign bodies (FBs).
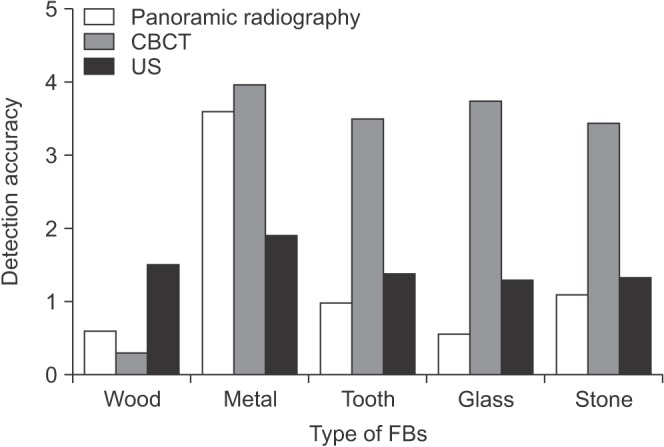
Fig. 4
Detection accuracy of panoramic radiography, cone-beam computed tomography (CBCT) and ultrasonography (US) for different size of foreign bodies (FBs).
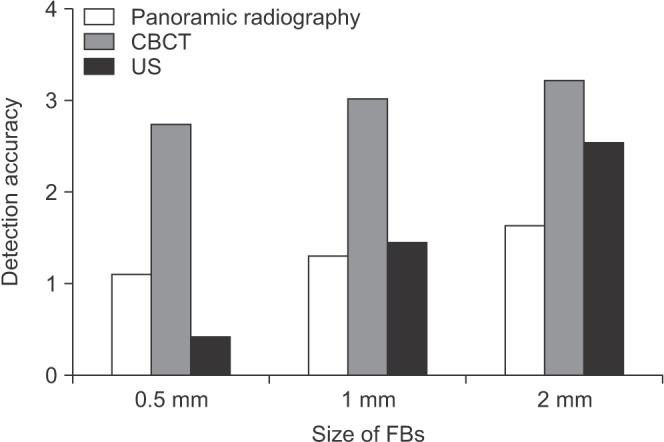
Fig. 5
The accuracy of the panoramic radiography, cone-beam computed tomography (CBCT) and ultrasonography (US) in detection of foreign bodies (FBs) in different locations.
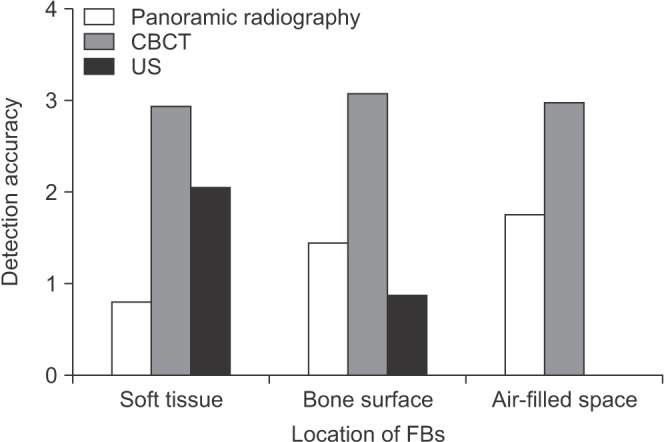
Table 1
Four-point scoring scale for image interpretation
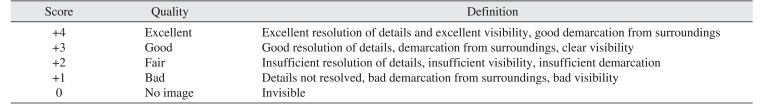
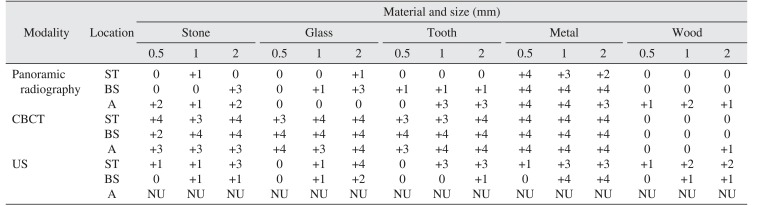
Table 2
Visibility scores of foreign bodies embedded on the ST, BS, and A using panoramic radiography, CBCT and US




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download