Abstract
Subcutaneous facial emphysema after dental treatment is an uncommon complication caused by the invasion of high-pressure air; in severe cases, it can spread to the neck, mediastinum, and thorax, resulting in cervical emphysema, pneumomediastinum, and pneumothorax. The present case showed subcutaneous cervicofacial emphysema with pneumomediastinum after class V restoration. The patient was fully recovered after eight days of conservative treatment. The cause of this case was the penetration of high-pressure air through the gingival sulcus, which had a weakened gingival attachment. This case indicated that dentists should be careful to prevent subcutaneous emphysema during common dental treatments using a high-speed hand piece and gingival retraction cord.
Subcutaneous facial emphysema after dental treatment is an uncommon complication caused by the invasion of high-pressure air generated from high-speed hand pieces and airwater syringes. In severe cases, it can spread to the neck, mediastinum, and thorax along with the fascial planes, resulting in cervical emphysema, pneumomediastinum, and pneumothorax12.
In previous literature, occurrences of subcutaneous facial emphysema after dental treatment have been reported following third molar extraction, endodontic treatment, class V restoration, crown preparation, and other treatments3456. The symptoms in these cases were mostly mild to severe swelling and crepitus on palpation of the affected area. Difficulty swallowing and breathing have also been seen when the deep neck space was involved1.
In this report, we introduce a case of iatrogenic subcutaneous cervicofacial emphysema with pneumomediastinum after class V restoration. The compressed air from the high-speed hand piece led the emphysema to spread from the right mandible to the facial, cervical, and anterior chest walls and the superior mediastinum.
A 59-year-old woman presented to the emergency department with facial, cervical, and chest swelling that had begun 1.5 hours earlier; she was previously healthy without any underlying disease. She had received dental restorative treatment for a class V defect in her right lower first premolar, and during the restoration procedure, an air-driven highspeed hand piece was used to polish the subgingival margin of the composite restoration. High-pressure air penetrated into the facial subcutaneous tissue through the gingival sulcus and spread from the right mandible to the facial, cervical, and anterior chest walls and the superior mediastinum. The dentist did not recognize the gradual swelling of the soft tissue due to a sterile covering drape.
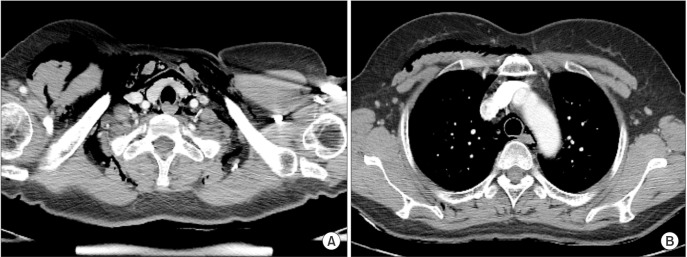
At the emergency department, the patient complained of a headache and dysphagia. Physical examination revealed crepitus on palpation of her facial, cervical, and chest areas, but dyspnea and neck stridor were not observed. Routine laboratory testing showed normal complete blood count and blood chemistry. Anterior-posterior chest radiograph revealed pneumomediastinum (arrows) and subcutaneous emphysema (arrowheads) with streaky radiolucencies.(Fig. 1) Diffuse soft tissue emphysema in the masticator space, neck space, anterior chest wall, and superior mediastinum were observed on computed tomography.(Fig. 2, 3)
The patient was admitted to the hospital for treatment of this emphysema. Specifically, she received conservative treatment with prophylactic antibiotics (ampicillin/sulbactam and metronidazole) and oxygen administered at 3 L/min via nasal prong. Daily observations revealed her facial, cervical, and chest swelling improved gradually, and chest radiograph also showed decrease of the soft tissue emphysema. Eight days after the onset of the emphysema, the patient's symptoms had fully improved, and thus, she was discharged.
In common dental treatment, most subcutaneous facial emphysema occurs after the use of high-speed hand pieces and air-water syringes; high-pressure air can be forced into the surrounding soft tissue. As the emphysema progresses, the facial, cervical, and anterior chest walls and superior mediastinum can be involved12. If the cause of the emphysema is only the dental procedure, the pleural cavities are mostly not involved in the air invasion, and thus pneumothorax rarely occurs1. When dental treatment is performed under general anesthesia, anesthesia factors such as mechanical ventilation, airway injury, and subclavian catheterization can lead to pneumothorax78.
There are two different pathways by which high-pressure air invades subcutaneous tissue. First, high-pressure air can be spread through osseous tissue, for instance, subcutaneous facial emphysema after endodontic treatment4. Particularly, bone destruction caused by pathologic lesions or iatrogenic injury may carry a high risk for subcutaneous facial emphysema.
Another pathway is through the periosteal and submucosal tissue. Excessive reflection of the mucoperiosteal flap during surgical extraction of the third molar can cause emphysema by subperiosteal dissection with high-pressure air910. The use of a gingival retraction cord and having a periodontal disease also cause the loosening of the gingival sulcus and junctional epithelium. The weakness of the gingival attachment can help the high-pressure air to invade subcutaneous soft tissue511. In the present case a gingival retraction cord was used to retract the gingival tissue. In addition, the right lower first premolar had a deep periodontal pocket that exceeded 5 mm. Thus, the high-pressure air might have easily invaded through the gingival sulcus and then spread to the adjacent soft tissue.
Most cases of subcutaneous facial emphysema do not require a specific treatment. It generally resolves spontaneously in approximately one week1. However, in severe cases when the emphysema spreads to the neck, mediastinum, and thorax areas, it can lead to life-threatening problems; subcutaneous cervical emphysema can induce difficulty breathing by narrowing the airway, and pneumomediastinum and pneumothorax can affect normal heart and lung function due to air compression. In emergency cases, surgical intervention using a small incision, needle puncture, and chest tube can be required to drain the air1.
In the previous literature on subcutaneous facial emphysema, more cases used prophylactic antibiotics than did not. Thus, in the present case prophylactic antibiotics (ampicillin/sulbactam and metronidazole) were used to prevent local or systemic infection by oral flora. Though the possibility of infection exists as a consequence of this emphysema, its occurrence is in fact rare irrespective of the use of prophylactic antibiotics1, and thus, using them is not essential for these patients. However, if the use of antibiotics is not contraindicated, it is safe to use them because the possibility of infection cannot completely be ruled out. Moreover, although there is a low probability that the mediastinum will become involved in acute infection, cases of acute mediastinitis have been associated with a 25% to 50% mortality rate12.
Oxygen administration at a high flow rate can also be considered for conservative treatment of subcutaneous emphysema. It may help with resorption of trapped nitrogen by decreasing the surrounding partial nitrogen pressure13. The present case used oxygen at 3 L/min via nasal prong to rapidly decrease the trapped air volume.
This case showed severe subcutaneous cervicofacial emphysema with pneumomediastinum after class V restoration. The causes were (1) high-pressure air from a high-speed hand piece and (2) a weakened gingival attachment due to use of a gingival retraction cord and existing chronic periodontitis. In addition, due to the sterile covering drape, the dentist did not recognize the gradual progression of the subcutaneous emphysema until the patient complained of her symptoms. This case indicated that dentists should be careful of the occurrence of subcutaneous emphysema when they use high-speed hand pieces and gingival retraction cords in common dental procedures.
References
1. McKenzie WS, Rosenberg M. Iatrogenic subcutaneous emphysema of dental and surgical origin: a literature review. J Oral Maxillofac Surg. 2009; 67:1265–1268. PMID: 19446214.

2. Heyman SN, Babayof I. Emphysematous complications in dentistry, 1960-1993: an illustrative case and review of the literature. Quintessence Int. 1995; 26:535–543. PMID: 8602428.
3. Kung JC, Chuang FH, Hsu KJ, Shih YL, Chen CM, Huang IY. Extensive subcutaneous emphysema after extraction of a mandibular third molar: a case report. Kaohsiung J Med Sci. 2009; 25:562–566. PMID: 19767263.

4. Smatt Y, Browaeys H, Genay A, Raoul G, Ferri J. Iatrogenic pneumomediastinum and facial emphysema after endodontic treatment. Br J Oral Maxillofac Surg. 2004; 42:160–162. PMID: 15013551.

5. Chan DC, Myers T, Sharaway M. A case for rubber dam application--subcutaneous emphysema after Class V procedure. Oper Dent. 2007; 32:193–196. PMID: 17427830.

6. Zemann W, Feichtinger M, Kärcher H. Cervicofacial and mediastinal emphysema after crown preparation: a rare complication. Int J Prosthodont. 2007; 20:143–144. PMID: 17455433.
7. Reiche-Fischel O, Helfrick JF. Intraoperative life-threatening emphysema associated with endotracheal intubation and air insufflation devices: report of two cases. J Oral Maxillofac Surg. 1995; 53:1103–1107. PMID: 7643284.
8. Maestrello CL, Campbell RL, Campbell JR. Pneumothorax with soft tissue emphysema following abrupt wake-up and self-extubation. Anesth Prog. 2001; 48:27–31. PMID: 11495402.
9. Olate S, Assis A, Freire S, de Moraes M, de Albergaria-Barbosa JR. Facial and cervical emphysema after oral surgery: a rare case. Int J Clin Exp Med. 2013; 6:840–844. PMID: 24179581.
10. Horowitz I, Hirshberg A, Freedman A. Pneumomediastinum and subcutaneous emphysema following surgical extraction of mandibular third molars: three case reports. Oral Surg Oral Med Oral Pathol. 1987; 63:25–28. PMID: 3543796.

11. Snyder MB, Rosenberg ES. Subcutaneous emphysema during periodontal surgery: report of a case. J Periodontol. 1977; 48:790–791. PMID: 271225.

12. Athanassiadi KA. Infections of the mediastinum. Thorac Surg Clin. 2009; 19:37–45. PMID: 19288819.

13. Ali A, Cunliffe DR, Watt-Smith SR. Surgical emphysema and pneumomediastinum complicating dental extraction. Br Dent J. 2000; 188:589–590. PMID: 10893812.

Fig. 1
Anterior-posterior chest radiograph revealed pneumomediastinum (arrows) and subcutaneous emphysema (arrowheads) with streaky radiolucencies.
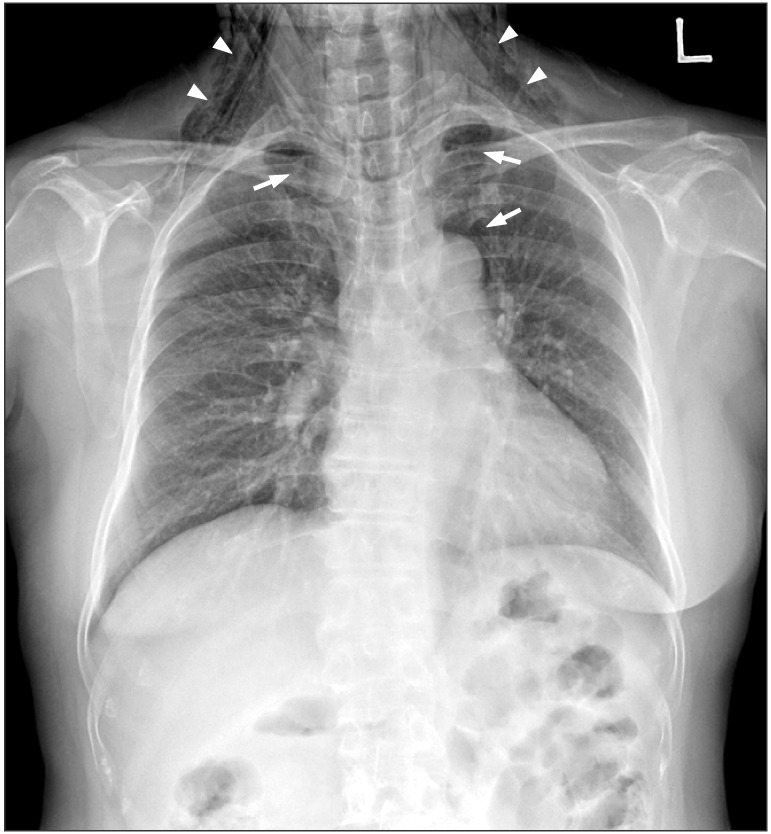
Fig. 2
Diffuse soft tissue emphysema in the masticator space, peripharyngeal space, and superior mediastinum was observed on computed tomography. A. Coronal view at the mental foramen level: the facial emphysema extended into the right orbital cavity. B. Coronal view at the pharyngeal and laryngeal regions: the cervical emphysema was observed in the peripharyngeal space and superior mediastinum.
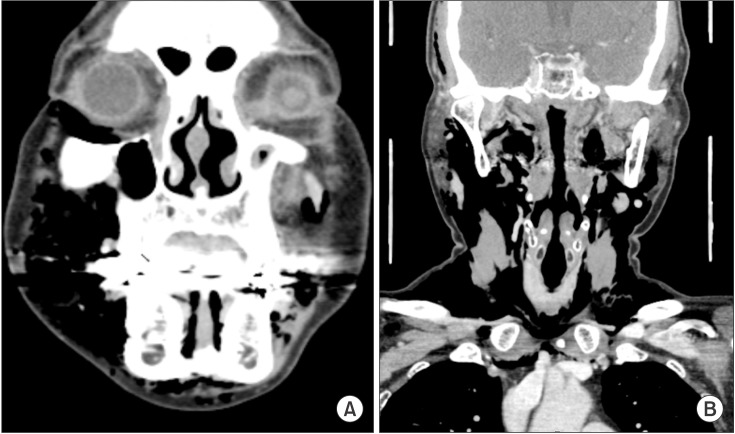
Fig. 3
Diffuse soft tissue emphysema in the peripharyngeal space, both the anterior and posterior triangles of the neck, the anterior chest wall, and the superior mediastinum was observed on computed tomography. A. Axial view at the thyroid gland and clavicle: the cervical emphysema was observed in the peripharyngeal space, both the anterior and posterior triangles of the neck, and the anterior chest wall. B. Axial view at the aortic arch: the emphysema was observed on the anterior chest wall and the superior mediastinum.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download