This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
The study was designed to evaluate the efficacy of performing a second, repeat anterior maxillary distraction (AMD) to treat residual cleft maxillary hypoplasia.
Materials and Methods
Five patients between the ages of 12 to 15 years with a history of AMD and with residual cleft maxillary hypoplasia were included in the study. Inclusion was irrespective of gender, type of cleft lip and palate, and the amount of advancement needed. Repeat AMD was executed in these patients 4 to 5 years after the primary AMD procedure to correct the cleft maxillary hypoplasia that had developed since the initial procedure. Orthopantomogram (OPG) and lateral cephalograms were taken for evaluation preoperatively, immediately after distraction, after consolidation, and one year postoperatively. The data obtained was tabulated and a Mann Whitney U-test was used for statistical comparisons.
Results
At the time of presentation, a residual maxillary hypoplasia was observed with a well maintained distraction gap on the OPG which ruled out the occurrence of a relapse. Favorable movement of the segments without any resistance was seen in all patients. Mean maxillary advancement of 10.56 mm was achieved at repeat AMD. Statistically significant increases in midfacial length, SNA angle, and nasion perpendicular to point A distance was achieved (P=0.012, P=0.011, and P=0.012, respectively). Good profile was achieved for all patients. Minimal transient complications, for example anterior open bite and bleeding episodes, were managed.
Conclusion
Addressing the problem of cleft maxillary hypoplasia at an early age (12–15 years) is beneficial for the child. Residual hypoplasia may develop in some patients, which may require additional corrective procedures. The results of our study show that AMD can be repeated when residual deformity develops with the previous procedure having no negative impact on the results of the repeat procedure.
Go to :

Keywords: Cleft palate, Osteogenesis, Distraction, Maxilla
I. Introduction
Midface deficiency is a well-known problem in cleft lip and palate patients. The lack of growth of the midfacial structures leads to a flattened appearance of the middle third of the face and a concave profile, all of which have negative psychological impact on the patient. The traditional treatment for midfacial hypoplasia associated with cleft lip and palate is orthognathic surgery via Le Fort I osteotomy
1. With the advent of distraction osteogenesis (DO), there is another treatment modality available to treat midface hypoplasia. DO has lower relapse rates and better stability
2. However, both these methods advance the entire maxilla sagittally, which results in increased velopharyngeal incompetence because of the further separation of the soft palate from the posterior pharyngeal wall
3. Increased velopharyngeal incompetence is the biggest disadvantage of performing orthognathic surgery or Le Fort I distraction in cleft patients.
The first successful clinical application of anterior maxillary distraction (AMD) using an intraoral tooth-borne distractor was reported by Block and Brister
4 on dogs in 1994 and subsequently by Dolanmaz et al.
5 on humans in 2003. In AMD, the soft palate is not moved anteriorly and therefore there is no detrimental effect on the velopharyngeal sphincter. This makes it a suitable treatment option for midfacial hypoplasia in patients with cleft lip and palate since speech is a major concern in these patients
6. AMD can be done near the end of the mixed dentition period, after the second premolars erupt. There are no risks of performing AMD at an early age, for instance before the patient reaches skeletal maturity. In fact, it is desirable to correct the facial profile of these children as early as possible in order to provide these children with normal social lives.
Despite correction at an early age, many patients develop a concave profile again by the time they attain adulthood. The development of hypoplasia is thought to be due to the mandible continuing to grow at its normal rate through the remaining growth years while the maxilla ceases growth
7. Although overcorrection may be done at this stage, it often leads to an unappealing profile at a very crucial age and is best avoided.
For this reason, there is a need to find a treatment modality that can be performed again if residual deformity develops after the primary AMD had been performed. This study was conducted to understand the efficacy and feasibility of repeat AMD as a treatment option for correcting residual cleft maxillary hypoplasia.
Go to :

II. Materials and Methods
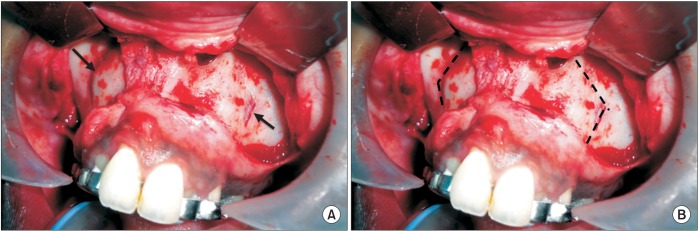
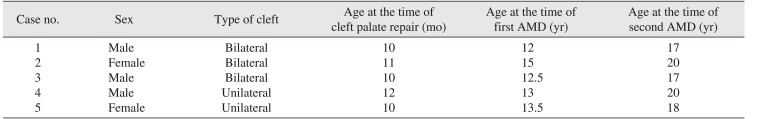
Richardsons Dental and Craniofacial Hospital's Institutional Ethical Committee approval was procured and an informed consent agreement was signed by all patients. Five patients were included in this retrospective study from June 2010 to March 2016. There were three cases of bilateral cleft palate and two cases of unilateral cleft palate that were previously repaired between 10–13 months of age. All patients had a history of a single AMD procedure done at the age group of 12–15 years. After the initial AMD, an orthopantomogram (OPG1) and a lateral cephalogram (LatCeph1) were taken. All patients developed residual midface hypoplasia requiring a second AMD by the time they attained 17–20 years of age. (
Table 1)
Table 1
Summary of patient details
|
Case no. |
Sex |
Type of cleft |
Age at the time of cleft palate repair (mo) |
Age at the time of first AMD (yr) |
Age at the time of second AMD (yr) |
|
1 |
Male |
Bilateral |
10 |
12 |
17 |
|
2 |
Female |
Bilateral |
11 |
15 |
20 |
|
3 |
Male |
Bilateral |
10 |
12.5 |
17 |
|
4 |
Male |
Unilateral |
12 |
13 |
20 |
|
5 |
Female |
Unilateral |
10 |
13.5 |
18 |

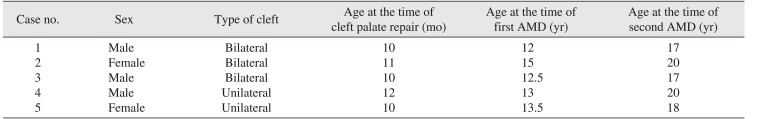
When patients presented with AMD a second time, they were evaluated with a new set of orthopantomograms and lateral cephalograms (OPG2 and LatCeph2, respectively). Because the new set of OPGs showed the maintenance of the previously created gap between the premolars and the molar, we determined that the midface hypoplasia was residual and not a relapse. The gap between the premolar and the molar was calculated using the Sidexis 4 software (Sirona Dental Company, Bensheim, Germany) as described here.
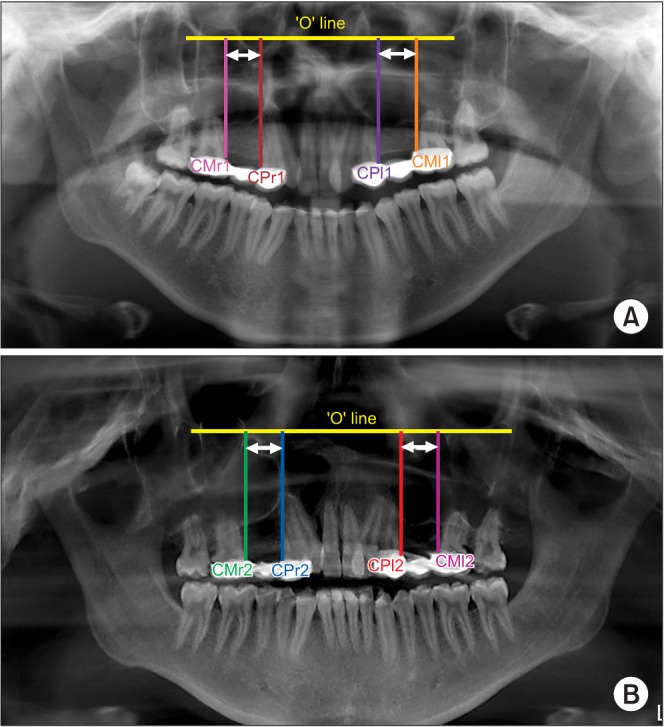
A line, termed the ‘O’ line, was made between the right and left orbitales on both the OPGs. The ‘O’ line was considered the stable line
8. The cemento-enamel junction of the distal border of the right and left premolars was marked in both OPGs as CPr1, CPl1, CPr2, and CPl2. Similarly, the cemento-enamel junction of the mesial border of the right and left molars was marked on both OPGs as CMr1, CMl1, CMr2, and CMl2. From all these points, perpendicular lines were drawn to the ‘O’ line and measurements between CPr1-CMr1, CPl1-CMl1, CPr2-CMR2 and CPl2-CMl2 were made in millimeters for every patient.(
Fig. 1) The means of CPr1-CMr1 and CPl1-CMl1 were calculated for every patient. The same method was repeated for CPr2-CMR2 and CPl2-CMl2, and the results were tabulated. IBM SPSS Statistics 19.0 for Windows (IBM Co., Armonk, NY, USA) was used for statistical analysis. A Mann-Whitney U-test was used to compare values, and the significance value was set at
P<0.05.
 | Fig. 1OPG1 and OPG2 showing maintenance of the bone formed after initial AMD procedure. A. Measuring distance between CMr1-CPr1 and CMl1-CPl1 in OPG1. B. Measuring distance between CMr2-CPr2 and CMl2-CPl2 in OPG2. CPr1/2=cemento-enamel junction of the distal border of the right premolar in OPG1/OPG2, respectively; CMr1/2=cemento-enamel junction of the mesial border of the right molar in OPG1/OPG2, respectively; CPl1/2=cemento-enamel junction of the distal border of the left premolar OPG1/OPG2, respectively; CMl1/2=cementoenamel junction of the mesial border of the left molar OPG1/OPG2, respectively. (OPG1: orthopantomogram taken after completion of intital AMD, OPG2: orthopantomogram taken at the second time of presentation)
|
The amount of advancement required for correction of the residual midface hypoplasia was based on the new radiographs (OPG2 and LatCeph2) taken at the time of presentation during adulthood. Cephalometric studies using McNamara's analysis
9 was performed using the Sidexis 4 software on two radiographs, LatCeph2, and on the one-year follow-up radiograph, LatCeph5. IBM SPSS Statistics 19.0 for Windows was used for statistical analysis. A Mann-Whitney U-test was used to compare values, and the significance value was set at
P<0.05.
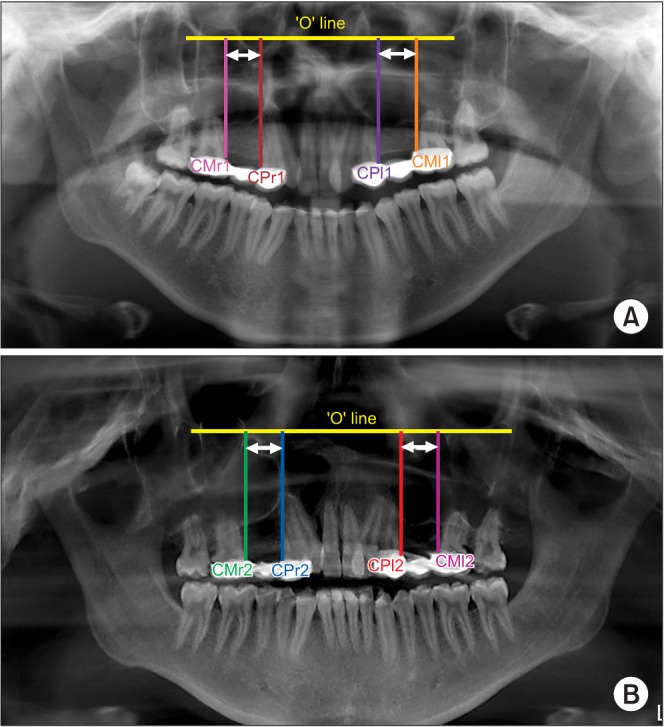
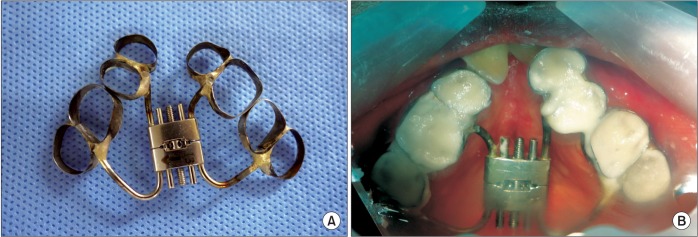
The appliance was fabricated as described previously on a dental model with the hyrax screw (Forestadent Co., Pforzheim, Germany) oriented parallel to the midpalatal raphe. The arms of the hyrax were soldered to bands and the appliance was cemented to the premolars anteriorly and molars posteriorly.(
Fig. 2. A) In one case, the premolar was missing and the band was cemented to the canine. This appliance was cemented preoperatively in the patient's mouth. (
Fig. 2. B) Then, acrylic bite blocks were prepared on the molars to open the bite and avoid any occlusal interference during distraction. An acrylic plate was fabricated separately around the anterior teeth, which included the premolars, and encompassed the teeth from the lingual, incisal/occlusal, and buccal sides in order to hold the anterior fragment firmly and distribute the forces of distraction.
 | Fig. 2The distractor appliance. A. The distractor appliance after its laboratory fabrication consisting of the hyrax screw and tooth bands. B. Appliance cemented intra-orally.
|
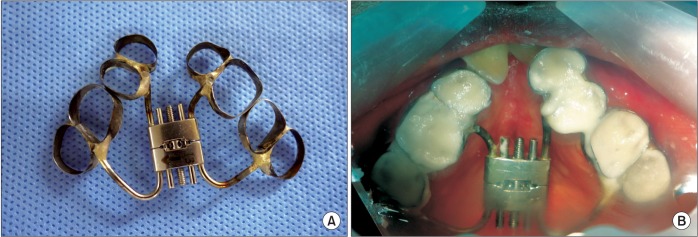
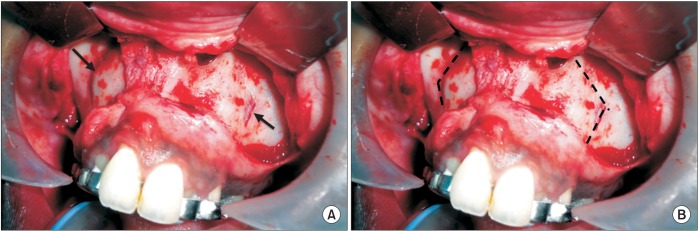
1. Surgical technique
Under general anesthesia, a maxillary degloving incision was performed between the molars. Subperiosteal dissection proceeded bilaterally up until the infraorbital foramen. After reflection of the mucoperiosteal flap, the previous osteotomy cuts were faintly visible in three cases and were utilized. In the other two cases, new osteotomy cuts were made horizontally, starting from the pyriform rim till a point where the deemed vertical cut would begin. Using a bur, vertical interdental cuts were made between the second premolar and first molar through the buccal cortex.(
Fig. 3) Lateral nasal osteotomes were used on both sides to separate the lateral nasal wall from the pyriform rim at the same level of the buccal cut. An elevator was used to protect the nasal mucosa. The palatal osteotomy was performed using a spatula osteotome, with particular care taken to avoid perforating the palatal mucosa. Gentle luxation was done between the cuts to ensure mobilization of the segment. The distractor screw was activated intraoperatively to check the symmetrical movement on both sides. Closure was performed with 3-0 Vicryl sutures (Ethicon Inc., Somerville, NJ, USA).
 | Fig. 3The osteotomy cuts. A. The arrows pointing towards the previous osteotomy cuts at the time of second anterior maxillary distraction (AMD). B. Fresh osteotomy cuts to be made for the AMD (dashed line).
|
2. Distraction protocol
We followed mean latency period of 5 to 7 days. Due to an accidental tear of the palatal mucosa intraoperatively in one case, we used an eight-day latency period. Following the latency period, the screw was turned three revolutions, twice daily. The pitch of the screw was 0.18 mm and therefore the amount of distraction achieved per day was 1.08 cm. Distraction proceeded until a positive overjet and the desired facial profile was achieved. Consolidation was carried out for a period of 8 to 10 weeks by keeping the appliance in situ. After removing the distractor, an acrylic plate was inserted for a period of 3 to 4 weeks in order for the occlusion to settle. Fixed prosthesis was fabricated in the space created between the distraction segments; crowding, if present, was corrected by orthodontics. Orthopantomograms and lateral cephalograms were taken immediately after distraction (OPG3 and LatCeph3), after the consolidation period (OPG4 and LatCeph4), and before the appliance removal at the one-year follow-up visit (OPG5 and LatCeph5).
Go to :

III. Results
There was a total of five patients in the study. Three were male and two were female. Three patients had a repaired bilateral cleft palate, and two had a unilateral repaired cleft palate. The mean age at the second presentation was 18.4 years. The minimum follow-up period was one year.
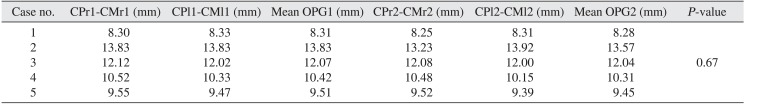
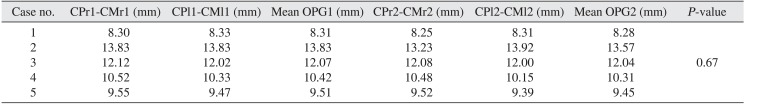
The results of the Mann-Whitney U-test showed no significant change in the measurements taken on OPG1 and OPG2 (
P=0.67). The lack of a significant change demonstrated that the cleft maxillary hypoplasia at presentation was residual since the gap created by the initial distraction procedure was still maintained.(
Fig. 4,
Table 2)
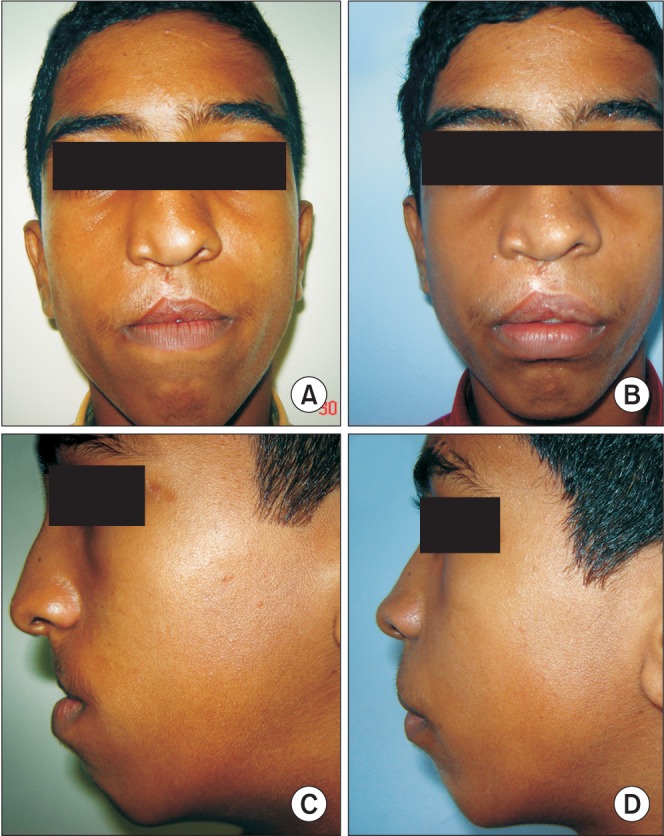
Fig. 5 shows the cephalogram taken after the completion of the first AMD procedure.
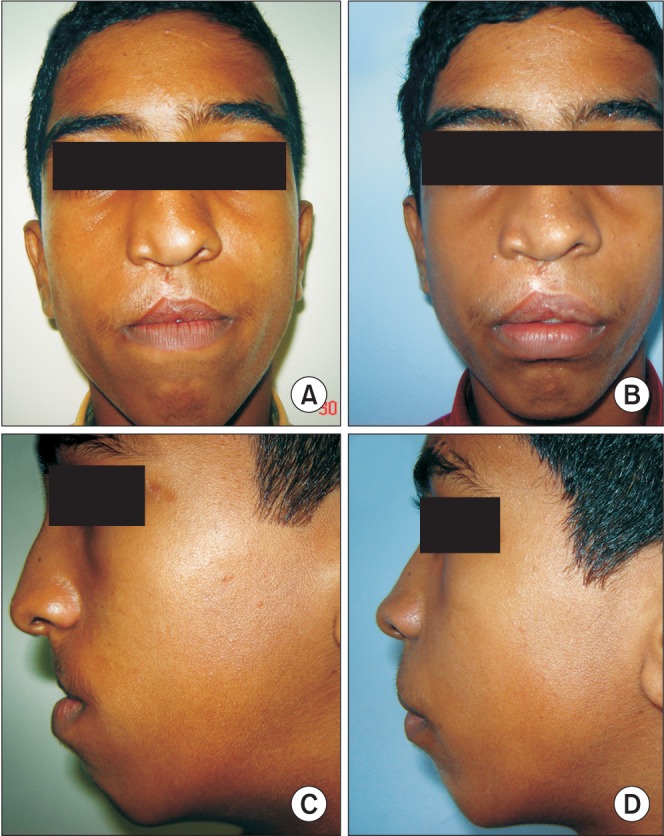 | Fig. 4Clinical photographs of the initial anterior maxillary distraction procedure (at 12 years). A. Frontal view pre-distraction. B. Frontal view post-distraction. C. Side profile pre-distraction. D. Side profile post-distraction.
|
 | Fig. 5Lateral cephalogram taken after the completion of the initial anterior maxillary distraction procedure (LatCeph1).
|
Table 2
Comparison of the created distraction gap in OPG's taken after the first distraction (OPG1) and after the subsequent presentation (OPG2)
|
Case no. |
CPr1-CMr1 (mm) |
CPl1-CMl1 (mm) |
Mean OPG1 (mm) |
CPr2-CMr2 (mm) |
CPl2-CMl2 (mm) |
Mean OPG2 (mm) |
P-value |
|
1 |
8.3 |
8.33 |
8.31 |
8.25 |
8.31 |
8.28 |
|
|
2 |
13.83 |
13.83 |
13.83 |
13.23 |
13.92 |
13.57 |
|
|
3 |
12.12 |
12.02 |
12.07 |
12.08 |
12.00 |
12.04 |
0.67 |
|
4 |
10.52 |
10.33 |
10.42 |
10.48 |
10.15 |
10.31 |
|
|
5 |
9.55 |
9.47 |
9.51 |
9.52 |
9.39 |
9.45 |
|

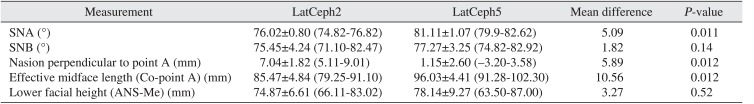
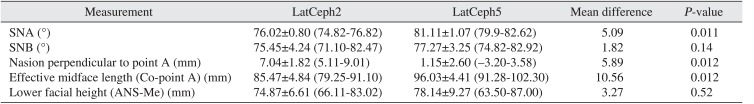
Cephalometric analysis showed significant improvement of most parameters in LatCeph5 when compared to LatCeph2. (
Table 3) The mean increases in the midfacial length (10.56 mm), in the SNA angle (5.09°), and the distance between the nasion perpendicular to point A (5.89 mm) were all statistically significant (
P=0.012,
P=0.011, and
P=0.012, respectively). The changes in the SNB angle (1.82°) and lower facial height (3.27 mm) were not statistically significant (
P=0.14 and
P=0.52, respectively). A straight profile was maintained for all patients, and a positive overjet was achieved.(
Fig. 6) There was also evidence of solid bone formation between the osteotomy site on LatCeph5, which was taken after completion of the second AMD.(
Fig. 7) Dental rehabilitation for the created gap was conducted on four of the patients by fixed prosthesis. One patient underwent orthodontic treatment to fill the created gap by moving the crowded teeth to an optimal position. No complications from the surgical procedures were observed either intraoperatively or postoperatively.
 | Fig. 6Clinical photographs of anterior maxillary distraction procedure the second time (at 17 years). A. Front view showing residual maxillary hypoplasia (pre-distraction). B. Front profile after distraction. C. Side profile before distraction. D. Side profile after distraction.
|
 | Fig. 7Lateral cephalogram taken after the second anterior maxillary distraction was completed (LatCeph5).
|
Table 3
McNamara analysis performed on LatCeph2 and LatCeph5 to assess the skeletal changes after the second anterior maxillary distraction (AMD)
|
Measurement |
LatCeph2 |
LatCeph5 |
Mean difference |
P-value |
|
SNA (°) |
76.02±0.80 (74.82–76.82) |
81.11±1.07 (79.9–82.62) |
5.09 |
0.011 |
|
SNB (°) |
75.45±4.24 (71.10–82.47) |
77.27±3.25 (74.82–82.92) |
1.82 |
0.14 |
|
Nasion perpendicular to point A (mm) |
7.04±1.82 (5.11–9.01) |
1.15±2.60 (−3.20–3.58) |
5.89 |
0.012 |
|
Effective midface length (Co-point A) (mm) |
85.47±4.84 (79.25–91.10) |
96.03±4.41 (91.28–102.30) |
10.56 |
0.012 |
|
Lower facial height (ANS-Me) (mm) |
74.87±6.61 (66.11–83.02) |
78.14±9.27 (63.50–87.00) |
3.27 |
0.52 |

Go to :

IV. Discussion
Maxillary hypoplasia is a common deformity in cleft lip and palate patients, and approximately 25% of these patients require orthognathic surgery to correct
10. Sagittal advancement of the entire maxilla has a relapse rate of 20% to 60%
11. Sagittal advancement of the maxilla also alters the speech of the patient
12.
With the application of DO to facial structures in the 1990s, maxillary distraction has become a viable alternative to osteotomy for correcting midfacial hypoplasia. Distraction can be achieved using a cranially attached rigid distractor, an orthodontic facemask, or by using internal distractors
13. Usually distraction is performed using a rigid external device or an intraoral distractor at a Le Fort I level. This procedure also has a negative impact on speech
14. Since both Le Fort I osteotomy and a LeFort I DO involve moving the entire maxilla off the posterior pharyngeal wall, the risk of velopharyngeal insufficiency is similar in both procedures
14.
AMD is a method of advancing only the anterior part of the maxilla. It relieves dental crowding of the upper arch, allows normal eruption of canines, and corrects the retrusion of the maxilla
15. Since the advancement only affects the anterior part of the maxilla, the velopharyngeal muscles are not affected and velopharyngeal closure is maximally preserved
16. Not only is the velopharyngeal sphincter preserved, it has been found that all parameters of speech, such as velopharyngeal incompetence, nasal air emission, resonance, articulation errors, and intelligibility, are significantly improved after AMD
6. This is the biggest advantage that AMD has over the other conventional treatment modalities. Another advantage is that the new bone deposition between the osteotomy cuts create space in the arch to correct crowding and to assist in the eruption of the canines without the need for tooth extraction
1015.
There are only two treatment options available to treat cleft maxillary hypoplasia for patients 11 to 13 years; total maxillary distraction or AMD. Orthognathic surgery can be performed only after growth completion and face-mask therapy should be provided for the younger age group
1617. Although total maxillary distraction can be done at any age, its negative impact on velopharyngeal function makes it the least viable of the two alternatives. It may be preferred when advancements greater than 13 mm are required since the maximum movement achieved with AMD is 13 mm due to the limitation of the screw used.
As seen in our study, all five patients had undergone AMD once before at mean age of 13 years. At the time of the first procedure we had achieved good facial profile and positive overjet. No overcorrection was done. Over time, the rest of the patient's facial skeleton (in particular, the mandible) continued to grow normally and the patient developed a retrusive midfacial appearance. Cleft maxillary hypoplasia is thought to occur due to both the inherent developmental deficiency of the cleft structures and due to the ill effects of surgies done in childhood to treat the primary cleft
18. Although relapse is also encountered after AMD, those cases were excluded from our study. Radiographic analysis proved that it was a residual deformity, and not a relapse, since the distraction gap was maintained.
At presentation, a negative overjet and a concave facial profile was observed in the five patients. Repeat AMD was planned and we achieved satisfactory results in all cases. There were no negative effects from the previous AMD in our results. One-year follow-up showed stable results. There were significant improvements in the cephalometric parameters. The parameters pertaining to the maxilla (midface length), SNA angle, and the nasion perpendicular line distance to point A increased significantly.
There was minor variation in the surgical technique when performing the procedure for the second time. First, nasal septal separation from the maxillary crest was not required. Second, in most cases the previous osteotomy line, if visible, could be followed. Also, if there was sufficient space created from the primary AMD between the second premolar and first molars, the buccal vertical osteotomy cuts could be safely used a second time without injuring the teeth. After completion of the final AMD, dental rehabilitation could be performed using a crown or implant.
A few disadvantages of AMD were as follows. 1) The lack of effective vector controls, which caused anterior open bite in a few cases but was corrected with the application of box elastics before the completion of consolidation. 2) Minor bleeding episodes were encountered during the patient recovery period, which were managed conservatively.
Our findings are encouraging and suggest that AMD could be a preferred treatment modality to treat cleft maxillary hypoplasia at our center since it can be performed as early as 11 years of age and can be repeated later without complication. Treating cleft maxillary hypoplasia at a young age provides the child with an opportunity to live normally and does not jeopardize future treatments that may be done once the child attains skeletal maturity.
Go to :

V. Conclusion
Children suffering from cleft maxillary hypoplasia do not have to wait for skeletal maturity to be treated. We have found AMD to be an effective treatment modality that can correct the facial deformities as early as 11 years and can be repeated again at any stage if residual deformity develops.
Go to :








 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download