III. Discussion
There are many treatment options for management of mandibular condylar fractures, including open reduction through an intraoral or extraoral approach and closed reduction. The prognosis for each treatment is very controversial
1.
Hidding et al.
2 compared ORIF (20 cases) and CRMMF (14 cases) and found that deviation on mouth opening occurred in 64% of cases in the CRMMF group compared with 10% in ORIF group. In addition, anatomic reconstruction of the condyle was seen in 93% of the ORIF group but only 7% of the CRMMF group.
According to Zide and Kent
3 and Zide
4, there are absolute and relative indications for open reduction, such as bilateral condylar fracture, extracapsular dislocation, and displacement of the condyle. This seems to be supported by the work of Silvennoinen et al.
5, who have demonstrated an increased frequency in temporomandibular joint (TMJ) dysfunction and occlusal disorders when unilateral condyle fracture demonstrating dislocation or significant loss of ramus height as treated nonoperatively with inter-maxillary fixation only.
Open reduction and fixation are necessary to maintain the anatomic reduction of the condyle and the height of the ramus. However, in cases of high condyle fracture or displacement or dislocation of the condyle to the antero-medial side, it can be difficult to secure a field of vision during open reduction. Although a preauricular or endaural approach is used to obtain field of vision, there is a possibility of nerve damage due to the adjacent facial nerve. Also, surgical difficulty remains an issue due to the narrow field of view and work space
6.
Extracorporeal reduction is one possible method to solve this problem. Through removal of the ramal part by vertical ramal osteotomy, this procedure can obtain a view of the condylar fracture site and easy handling of the instrument. It is also accurate and relatively easy because reduction and internal fixation are performed out of body
7.
However, extracorporeal reduction implies that fractured condylar fragments are separated from the TMJ capsule. In other words, the soft tissues including the lateral pterygoid muscle are completely detached, increasing the risk of condylar resorption, such as with a free graft
89.
Davis et al.
8 reported that advanced condylar resorption occurred in 3 out of 10 patients who underwent free-grafting of the fractured condyle. Iizuka et al.
10 reported less encouraging results in 10 free-grafted patients with miniplate fixation for high condylar fractures, reporting ‘significant resorption’ in 85% of cases.
In 1995, Pereira et al.
9 reported the clinical and radiological results of surgical treatment of 17 patients with 21 dislocated fractures of the condylar process of the mandible. In this series, in all cases in which the lateral pterygoid muscle remained attached to the fractured segment, x-ray and tomography images confirmed a normal shape and contour of the condylar process. On the other hand, in those cases in which the fractured segment was maintained as a free graft, the majority (12 of 13 patients) showed signs of resorption of the condylar process with resulting shortening of the vertical dimension of the mandible and signs of remodeling, especially of the mandibular fossa, which became flat or even convex.
Therefore, prevention of condyle resorption can be expected if intracorporeal reduction of condylar fracture was performed using both pedicled condylar and separated ramal fragments after vertical ramal osteotomy. Reduction of a condylar fragment to a separated ramal fragment in the intracorporeal state without detaching the lateral pterygoid muscle from the condylar fragment can be more difficult than in the extracorporeal state. However, displacing the ramal part medially and pulling down the condylar fragment can provide a field of view and work space even though it is not convenient.
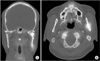
In our study, Case 1 had undergone SPECT at postoperative 1 week. Blood supply to the condylar and osteotomized ramal fragments was suspected due to hot spots on the left fragments in SPECT.(
Fig. 5) Tc-99m accumulates in areas of increased bone formation and increased angiogenesis, allowing visualization of inflammation. Because fracture healing involves inflammation, reparative, and remodeling phases, the hot spots are believed to be evidence of angiogenesis in the inflammation phase of fracture healing.
However, there are very few studies using SPECT for condylar fractures. Therefore, comparative studies with extracorporeal reduction or long-term follow-up studies are necessary.
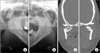
In Cases 2 and 3, diagnosed as bilateral condylar fractures, there were signs of condylar displacement accompanied by plate fractures and screw loosening on 1- or 5-month radiographs. However, postoperative 8-month or 2-year radiographs showed bone remodeling at the displaced fracture site with increased radiodensity. This suggests that the fragments had vitality due to maintained blood supply at the fracture site. As a result, complete remodeling of condylar fragments with restored anatomic appearance was observed on all final follow-up radiographs.(
Fig. 7. D,
9. D) There were no symptoms of condylar dysfunction during the healing and remodeling periods.
Condylar resorption is avascular necrosis with consequent shortening and loss along the vertical dimension of the mandible. In this paper, the definition of condylar resorption was resorption of more than one-third of the condyle length compared with the condyle dimension immediately after treatment or on the opposite side of the condyle
11.
Remodeling is a state of healing after fracture. The shapes of condylar fragments can be changed by a mechanical element, but the vertical dimension of the mandible is maintained.
Complete detachment of the soft tissue from the ramal and condylar fragments increases the risk of avascular necrosis as with a free graft, which can lead to condylar resorption. To prevent avascular necrosis, intracorporeal reduction of a condylar fracture using both pedicled condylar and separated ramal fragments after vertical ramal osteotomy was performed. As a result, despite displacement of fragments in the bilateral condylar fractures, condylar resorption was not observed on postoperative 8-month or 2-year radiograph, and anatomical appearance was maintained.
When calcification is increased, a hard callus can be observed in the panorama, indicating that hard callus forms 20 to 60 days after surgery. The remodeling phase, the last stage of healing, is a long, slow process that lasts from months to years. Davis et al.
8 reported that, of 10 patients who had undergone 11 free graft procedures, three required secondary costochondral reconstruction due to advanced resorption of the free-grafted condylar segment, occurring from 3 to 9 months following the initial trauma surgery.
Therefore, follow-up is needed at 3 months postoperatively because radiological changes can be observed and also at 1 year postoperatively to assess the remodeling phase.
Case 1 might require a longer follow-up period to evaluate condylar resorption. No condylar resorption was observed on postoperative 8-month or 2-year radiograph, and anatomical appearance was maintained in Cases 2 and 3, respectively.
It is obvious that restoring the vertical height through anatomical reduction and preventing avascular necrosis will reduce the risk of complications such as deviation on mouth opening and TMJ dysfunction.
Meanwhile, there were signs of condylar displacement accompanied by plate fractures and screw loosening on 1- or 5-month radiograph in Cases 2 and 3, respectively.
There are two major causes of plate fracture or screw loosening. The first cause is the force generated by the masticatory muscles; the second is the force produced by biting. In particular, the condylar fragments were loaded with direct force from the lateral pterygoid muscle, and the mandibular body and angle are also affected by the medial pterygoid muscle and the masseter muscle. Therefore, various forces such as bending and torsion are loaded onto the fracture line and the plate
12.
Double plate fixation can be considered as a solution to this problem. In Case 2, a single plate was used. Some authors reported plate fracture or screw loosening after application of a single miniplate for condylar fracture and mentioned that single miniplate fixation might be insufficient for reduction and fixation of condylar fracture
1012.
Tominaga et al.
12 reported that double adaptation plate fixation resulted in superior biomechanical stability in both fracture conditions in a laboratory setting.
However, in Case 3, plate fracture and screw loosening occurred after double plate fixation. In Case 3, we started mouth movement exercise two week after surgery to reduce TMJ complications, which is thought to be the stage of soft callus. Early mouth opening exercise can reduce TMJ complications, but can also reduce the stability of the internal fixation. Therefore, if the intermaxillary fixation period is increased to more than 2 weeks, the stage of soft callus can be prolonged, and the mechanical support can be increased, which could be a solution to the complication observed in Case 3.
In conclusion, all cases exhibited good healing aspects with no signs or symptoms of mandibular condylar dysfunction during the postoperative remodeling period after intracorporeal reduction of condylar fracture.











 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download