Abstract
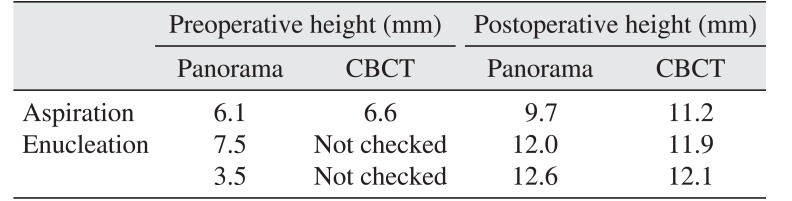
This case series study demonstrates the possibility of successful implant rehabilitation without bone augmentation in the atrophic posterior maxilla with cystic lesion in the sinus. Sinus lift without bone graft using the lateral approach was performed. In one patient, the cyst was aspirated and simultaneous implantation under local anesthesia was performed, whereas the other cyst was removed under general anesthesia, and the sinus membrane was elevated in a second process, followed by implantation. In both cases, tapered 11.5-mm-long implants were utilized. With all of the implants, good stability and appropriate bone height were achieved. The mean bone level gain was 5.73 mm; adequate bone augmentation around the implants was shown, the sinus floor was moved apically, and the cyst was no longer radiologically detected. Completion of all of the treatments required an average of 12.5 months. The present study showed that sufficient bone formation and stable implantation in a maxilla of insufficient bone volume are possible through sinus lift without bone materials. The results serve to demonstrate, moreover, that surgical treatment of mucous retention cyst can facilitate rehabilitation. These techniques can reduce the risk of complications related to bone grafts, save money, and successfully treat antral cyst.
Lack of bone volume and poor bone quality in the posterior region of the maxilla have been thought to impede dental implantation rehabilitation. Many reports have introduced maxillary bone augmentation techniques12. Among them, sinus lift with bone graft has been regarded as the best. The conventional treatment is a lateral approach procedure with bone graft and immediate or delayed implantation23456. This necessitates a 6 to 8 months healing period for new bone formation as well as an additional 3 to 4 months of implant osseointegration4567. Thus, bone grafting in the sinus cavity prolongs the time needed for implantation success, which inconveniences patients. Furthermore, single stage implantation is practically difficult. Bone grafting entails the use of expensive graft materials and complicated, technically demanding procedures that incur higher morbidity rates18. Finally, there are no clear guidelines on which types of graft materials or implants are superior9. Consequently, some researchers have studied and devised methods of sinus augmentation that do not require bone materials.
The lateral approach without bone grafting materials for implant positioning in the maxillary sinus with cystic lesion has, to the best of our knowledge, not been reported in the literature. Maxillary cysts are unclear in nomenclature, with an unknown role in pathogenesis; in the literature10, it may not arrange which sinus with cyst could be underwent sinus augmentation. This present report introduces two patients with a shrinkage ridge in the maxilla and a mucous retention cyst in the paranasal sinus, both of whom were treated by lateral approach sinus lift without bone graft.
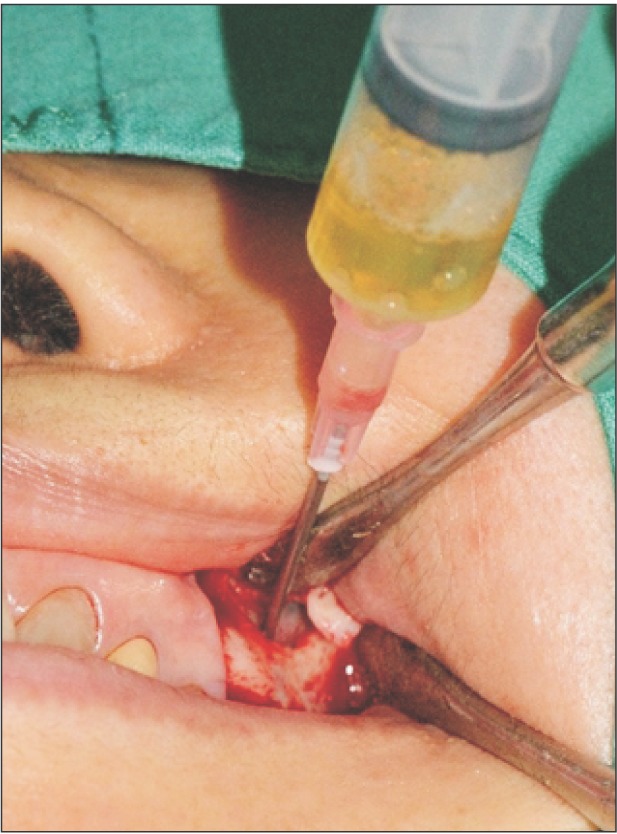
A 56-year-old woman visited our clinic with a complaint of repeated decementation of a gold crown on the left maxillary second molar. No specific condition was found in her oral cavity. She has good overall health and no medical history. In the panoramic view, the left upper second molar was in an incomplete endodontic treatment state, and the left maxillary sinus was pneumatized. The left posterior maxillary bone height was measured at 6.1 mm. Preoperative cone-beam computed tomography (CBCT) revealed a bone width of 13.7 mm and length of 6.6 mm, as well as a mucous retention cyst on the left maxillary sinus.(Fig. 1, Table 1) Under local anesthesia (2% lidocaine hydrochloride with 1:100,000 epinephrine), the left upper second molar was extracted. Vertical and horizontal incisions were performed, and the flap was lifted using a periosteal elevator. After drilling of the cortical bone of the left maxillary lateral wall, the bone cover was removed, and the Schneiderian membrane and cystic lesion were observed. Exudate was aspirated from the cyst with a syringe, after which the membrane was elevated.(Fig. 2) A 4.7×11.5 mm diameter implant (Zimmer; Zimmer Dental Inc., Carlsbad, CA, USA) was inserted in the extraction site with a torque of 40 Ncm. Guided bone regeneration was performed around the extraction site (Oss-guide 15×20 mm; Bioland, Cheonan, Korea) with autogenous bone. The incision line was sutured by 3-0 black silk. Postoperatively, the patient was administered second-generation cephalosporin antibiotics, nonsteroidal anti-inflammatory drugs, antihistamine, and 0.1% chlorohexidine for 7 days. On postoperative day 7, the sutures were removed. During the 7 months healing period, there were no complications or complaints, and the second surgery was performed. In the panoramic view, a bone height of 9.7 mm was determined.(Fig. 3, Table 1) An SCRP type prosthesis (porcelain fused metal, PFM) was implanted. There was no follow-up on this patient.
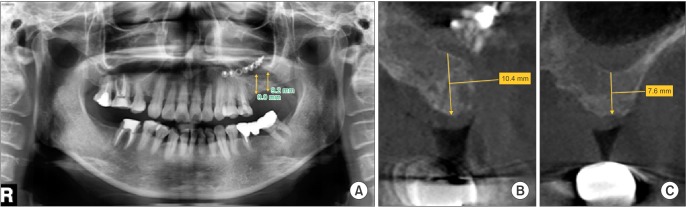
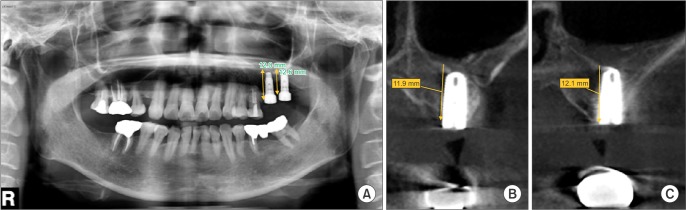
A 55-year-old woman presented at our clinic due to continual discomfort of the right maxillary first molar. She suffered from rheumatoid arthritis, but took no medication for that condition. The panoramic view showed generalized alveolar bone resorption on the maxilla, especially the left first molar; an edentulous left maxillary second molar; and a pneumatized left maxillary sinus with a dome-shaped cystic lesion in its lower area.(Fig. 4, Table 1) After treating the other teeth, the cyst was found to have grown larger and was scheduled for removal. Under general anesthesia, the left upper first molar was extracted, incision was performed vertically and horizontally, and the flap was dissected. Then, a bony window allowed visualization of the cystic lesion. After separating the cyst from the membrane, enucleation was performed, followed by curettage. The detached cortical bone was reattached with an 8-hole plate and 5 screws.(Fig. 5) The cyst was determined to be a mucous retention type. Eight months later, we decided to proceed with implant surgery.(Fig. 6) The left posterior maxillary bone heights were measured at 9.0 mm and 9.2 mm in panorama. Under local anesthesia (2% lidocaine hydrochloride with 1:100,000 epinephrine), the left maxillary first and second molar buccal gingiva was incised vertically and horizontally, and the flap was elevated. After removal of the cortical bone of the left maxillary lateral wall using a low speed hand piece, the Schneiderian membrane, which had completely recovered, was detected and elevated. Two implants (Zimmer) of 4.7×11.5 mm diameter were inserted at the operated site. The insertion torques were 37 Ncm and 23 Ncm, respectively. Additionally, the plate and screws were removed. The patient was administered second-generation cephalosporin antibiotics, acetaminophen, antihistamine, and 0.1% chlorohexidine for 7 days. The sutures were removed 7 days postoperatively. After 7 months, a panoramic x-ray confirmed good ridge gain (bone heights of 12.0 mm and 12.6 mm), so the second implantation surgery was performed.(Fig. 7, Table 1) An SCRP type prosthesis (PFM) was then placed. As of the 1-year follow-up, the implant was stable, and bone height was maintained.
In cases of atrophic maxillary ridge11, bone augmentation via maxillary sinus lift with grafting materials has been considered to be a complication-free method for successful implantation.
In a retrospective analysis of 127 patients treated with sinus lift by bone-graft augmentation, however, Moreno Vazquez et al.12 found significantly high intraoperative complication rates. Schneiderian membrane perforation had occurred in 50 patients (25.7%) and wound infection, abscess, or dehiscense with drainage in 30 others (14.9%). Acute maxillary sinusitis occurred in 6 cases, onlay graft exposure in 6 cases, and loosening of graft materials in 2 others. Furthermore, one study showed that, if sinus membrane perforation occurs, graft materials can aggravate maxillary sinusitis13. Such infection can lead to orbital cellulitis, meningitis, osteomyelitis, or cavernous sinus thrombosis14.
Almost all patients desire the least invasive, shortest, and cost-effective treatment. This has spurred the invention of new and better techniques. In 1980, Boyne and James5 introduced a lateral window approach to facilitate implantation in an atrophic maxillary ridge. To maintain the volume of the elevated membrane, they utilized considerable amounts of bone. Some authors considered this to be time and money-wasting as well as producing inflammation. Palma et al.15 compared bone grafting with no bone grafting in elevated space and found no differences in new bone formation, implant stability, or bone implant contact. They also discovered that implantation and blood clotting play volume maintenance roles prior to new bone formation. Lundgren et al.16 argued that the important factor for formation of new bone, regardless of the membrane material employed, is to maintain a space for blood clotting and the Schneiderian membrane superiorly. Other researchers have reported that only peripheral blood and clotting can sufficiently maintain elevated membrane for bone formation and osseointegration17. Thor et al.1 demonstrated that contact of blood with the implant surface can increase the amount of thrombin and platelets, thereby enhancing bone formation and osseointegration after the first stage of surgery. However, if very large amounts of bone enlargement are needed, immediate implantation is not feasible18. Takata et al.19 positioned an absorbable collagen membrane for a bony window, showing that rapid resorption of this membrane could be implicated in connective tissue invasion that prevents successful new bone formation.
Bone formation in the maxillary cavity is similar to that in an extraction socket20. Blood clotting under the Schneiderian membrane serves as a scaffold for bone formation16. Platelets activate thrombin, thus aiding osteoblast growth and preventing apoptosis around implants2122. Additionally, platelet-derived growth factors, insulin-like growth factors, transforming growth factor-β, vascular endothelial growth factors, and fibroblast growth factors lead to revascularization and osseointegration23. Exposure of the sinus wall by membrane elevation is essential to bone augmentation: mesenchymal cells coming from the medial and inferior wall of the sinus differentiate into osteoblasts. The periosteal membrane of the sinus is another source of these cells. However, this is uncertain, as some researchers have argued that the periosteal membrane contains few osteoblasts compared with other membranes above the cortical bone of both jaws20.
In the present cases, both patients had a mucous retention cyst in their left maxillary sinus, but only one was removed, while the other was only aspirated. In the removal case, perhaps the surgical trauma helped enlarge the residual bone volume24. In fact, when the cyst was enucleated, the vertical bone length grew from 7.5 to 9.0 and from 3.5 mm to 9.2 mm in the panoramic view. The effects of aspiration were uncertain since simultaneous sinus lift was performed; however, bone height increased after surgical intervention. Generally, it is thought that aspiration helps to decrease internal pressure by removing liquid, thus contributing to reduce lesion size and membrane perforation risk by thickening the sinus membrane10. Such cysts, which have an incidence rate of 1.4% to 9.6%, are identified on panorama or CBCT2526. Ziccardi and Betts27 pointed out that sinus grafting generally is prohibited in cases of mucous retention cyst. However, if bone augmentation is needed, it is better that removal or aspiration of the cyst precedes surgery. Others have argued that maxillary mucous retention cyst shows no symptoms and has nothing to do with the obstructive sinus phenomenon28. Reports on sinus lift in patients with these diseases are insufficient, and this is the reason for choosing the present cases for analysis. However additional studies are necessary.
In neither of these cases was any material used to elevate the membrane; instead, implants were placed. The initial, low-density maxillary bone heights in the enucleation case were 7.5 mm and 3.5 mm, while that in the aspiration case was 6.1 mm; appropriate bone height and stable implantation were achieved. According to the follow-up panorama image, there was adequate bone augmentation around the implants. A mean of all bone level gains was 5.73 mm in the panoramic view. Nevertheless, due to the limitations of the panoramic view, exact anatomical reference points are difficult to determine and measure and so might have been incorrect. In both of the present cases, there were no complaints or side-effects at the operating sites, and the implant stability quotient was high (Case 1: 81, Case 2: 79, 83).
In conclusion, sinus lift without bone materials shows new bone formation and implant stability according to radiographic and clinical evaluation. Especially, surgical procedures including aspiration and enucleation of cysts of the maxillary sinus stimulated increased bone volume. Which method is better is not yet clear. However, in the present case, aspiration of cyst was simple, time and cost effective, and did not require general anesthesia. Further evaluation should be based on long term observation of larger sample sizes.
References
1. Thor A, Rasmusson L, Wennerberg A, Thomsen P, Hirsch JM, Nilsson B, et al. The role of whole blood in thrombin generation in contact with various titanium surfaces. Biomaterials. 2007; 28:966–974. PMID: 17095084.

2. Esposito M, Grusovin MG, Worthington HV, Coulthard P. Interventions for replacing missing teeth: bone augmentation techniques for dental implant treatment. Cochrane Database Syst Rev. 2006; (1):CD003607. PMID: 16437460.

3. Garg AK. Augmentation grafting of the maxillary sinus for placement of dental implants: anatomy, physiology, and procedures. Implant Dent. 1999; 8:36–46. PMID: 10356455.
4. Chanavaz M. Maxillary sinus: anatomy, physiology, surgery, and bone grafting related to implantology--eleven years of surgical experience (1979-1990). J Oral Implantol. 1990; 16:199–209. PMID: 2098563.
5. Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980; 38:613–616. PMID: 6993637.
6. Schwartz-Arad D, Herzberg R, Dolev E. The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J Periodontol. 2004; 75:511–516. PMID: 15152813.

7. Tong DC, Rioux K, Drangsholt M, Beirne OR. A review of survival rates for implants placed in grafted maxillary sinuses using meta-analysis. Int J Oral Maxillofac Implants. 1998; 13:175–182. PMID: 9581402.
8. Thor A, Sennerby L, Hirsch JM, Rasmusson L. Bone formation at the maxillary sinus floor following simultaneous elevation of the mucosal lining and implant installation without graft material: an evaluation of 20 patients treated with 44 Astra Tech implants. J Oral Maxillofac Surg. 2007; 65(7 Suppl 1):64–72. PMID: 17586351.

9. Li J, Wang HL. Common implant-related advanced bone grafting complications: classification, etiology, and management. Implant Dent. 2008; 17:389–401. PMID: 19077576.

10. Mardinger O, Manor I, Mijiritsky E, Hirshberg A. Maxillary sinus augmentation in the presence of antral pseudocyst: a clinical approach. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:180–184. PMID: 17234532.

11. Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants. 2007; 22(Suppl):49–70. PMID: 18437791.
12. Moreno Vazquez JC, Gonzalez de Rivera AS, Gil HS, Mifsut RS. Complication rate in 200 consecutive sinus lift procedures: guidelines for prevention and treatment. J Oral Maxillofac Surg. 2014; 72:892–901. PMID: 24583086.

13. Kasabah S, Krug J, Simůnek A, Lecaro MC. Can we predict maxillary sinus mucosa perforation? Acta Medica (Hradec Kralove). 2003; 46:19–23. PMID: 12747535.

14. Timmenga NM, Raghoebar GM, Boering G, van Weissenbruch R. Maxillary sinus function after sinus lifts for the insertion of dental implants. J Oral Maxillofac Surg. 1997; 55:936–939. discussion 940. PMID: 9294502.

15. Palma VC, Magro-Filho O, de Oliveria JA, Lundgren S, Salata LA, Sennerby L. Bone reformation and implant integration following maxillary sinus membrane elevation: an experimental study in primates. Clin Implant Dent Relat Res. 2006; 8:11–24. PMID: 16681489.

16. Lundgren S, Andersson S, Gualini F, Sennerby L. Bone reformation with sinus membrane elevation: a new surgical technique for maxillary sinus floor augmentation. Clin Implant Dent Relat Res. 2004; 6:165–173. PMID: 15726851.

17. Moon JW, Sohn DS, Heo JU, Shin HI, Jung JK. New bone formation in the maxillary sinus using peripheral venous blood alone. J Oral Maxillofac Surg. 2011; 69:2357–2367. PMID: 21719179.

18. de Oliveira GR, Olate S, Cavalieri-Pereira L, Pozzer L, Asprino L, de Moraes M, et al. Maxillary sinus floor augmentation using blood without graft material. Preliminary results in 10 patients. J Oral Maxillofac Surg. 2013; 71:1670–1675. PMID: 23891012.

19. Takata T, Wang HL, Miyauchi M. Migration of osteoblastic cells on various guided bone regeneration membranes. Clin Oral Implants Res. 2001; 12:332–338. PMID: 11488862.

20. Misch CE. The maxillary sinus lift and sinus graft surgery. In : Misch CE, editor. Contemporary implant dentistry. 2nd ed. St. Louis: CV Mosby;1999. p. 482–493.
21. Frost A, Jonsson KB, Ridefelt P, Nilsson O, Ljunghall S, Ljunggren O. Thrombin, but not bradykinin, stimulates proliferation in isolated human osteoblasts, via a mechanism not dependent on endogenous prostaglandin formation. Acta Orthop Scand. 1999; 70:497–503. PMID: 10622485.

22. Pagel CN, de Niese MR, Abraham LA, Chinni C, Song SJ, Pike RN, et al. Inhibition of osteoblast apoptosis by thrombin. Bone. 2003; 33:733–743. PMID: 14555279.

23. Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. 2004; 91:4–15. PMID: 14691563.

24. Lundgren S, Andersson S, Sennerby L. Spontaneous bone formation in the maxillary sinus after removal of a cyst: coincidence or consequence? Clin Implant Dent Relat Res. 2003; 5:78–81. PMID: 14536041.

25. Paparella MM. Mucosal cyst of the maxillary sinus. Arch Otolaryngol. 1963; 77:650–670. PMID: 13941289.

26. MacDonald-Jankowski DS. Mucosal antral cysts observed within a London inner-city population. Clin Radiol. 1994; 49:195–198. PMID: 8143412.

27. Ziccardi VB, Betts NJ. Complications of maxillary sinus augmentation. In : Jensen OT, editor. The sinus bone graft. Chicago: London: Quintessence Publishing;1999. p. 201–208.
28. Bhattacharyya N. Do maxillary sinus retention cysts reflect obstructive sinus phenomena? Arch Otolaryngol Head Neck Surg. 2000; 126:1369–1371. PMID: 11074835.

Fig. 1
Removed #27 gold crown. The maxillary sinus was pneumatized. Bone height of 6.1 mm (panorama, A), 6.6 mm (cone-beam computed tomography, B) was measured.
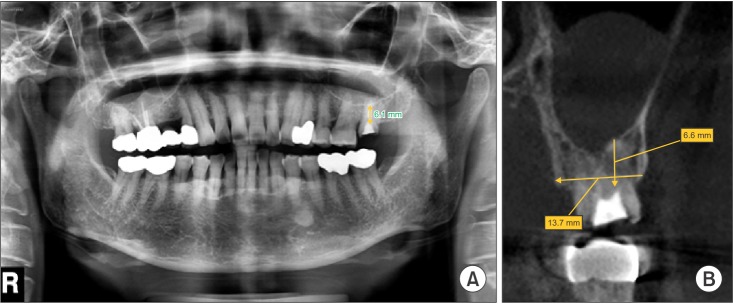
Fig. 3
Ten months postoperatively; bone height of 9.7 mm (panorama, A), 11.2 mm (cone-beam computed tomography, B) had been achieved.
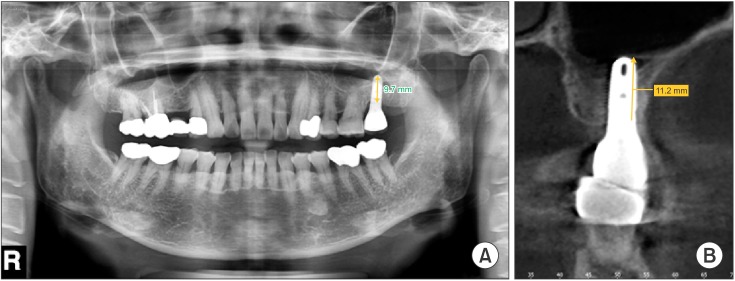
Fig. 4
Identification of cystic lesion in left maxillary sinus. The #27 crown was in the edentulous state. Bone heights of 7.5 mm (#26) and 3.5 mm (#27) were measured.
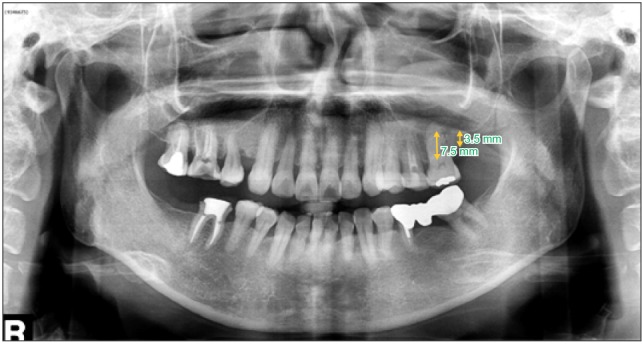
Fig. 5
Immediate after surgery: enucleation of cyst & fixation of bended 8-hole plate and five screws; extraction of #26.

Fig. 6
Eight months postoperatively: extraction socket was filled with new bone, and bone levels were elevated to 9.0 mm (panorama, A), 10.4 mm (cone-beam computed tomography [CBCT], B) (#26) and 9.2 mm (panorama, A), 7.6 mm (CBCT, C) (#27).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download