Abstract
Objectives
The purpose of this study is to compare the postoperative stability of conventional orthognathic surgery to a surgery-first orthognathic approach after bilateral sagittal split ramus osteotomy (BSSRO).
Materials and Methods
The study included 20 patients who underwent BSSRO for skeletal class III conventional orthognathic surgery and 20 patients who underwent a surgery-first orthognathic approach. Serial lateral cephalograms were analyzed to identify skeletal changes before surgery (T0), immediately after surgery (T1), and after surgery (T2, after 1 year or at debonding).
Results
The amount of relapse of the mandible in the conventional orthognathic surgery group from T1 to T2 was 2.23±0.92 mm (P<0.01) forward movement and −0.87±0.57 mm (non-significant, NS) upward movement on the basis of point B and 2.54±1.37 mm (P<0.01) forward movement and −1.18±0.79 mm (NS) upward movement on the basis of the pogonion (Pog) point. The relapse amount of the mandible in the surgery-first orthognathic approach group from T1 to T2 was 3.49±1.71 mm (P<0.01) forward movement and −1.78±0.81 mm (P<0.01) upward movement on the basis of the point B and 4.11±1.93 mm (P<0.01) forward movement and −2.40±0.98 mm (P<0.01) upward movement on the basis of the Pog.
Mandibular prognathism is one of the major maxillofacial deformities commonly seen in Asians, including Koreans12. Orthognathic surgery recovers the imbalanced maxilla and mandible with skeletal class III malocclusion, improving mastication, pronunciation, and facial esthetics, which can result in resolution of psychological problems. Recently, the demand of patients for improved esthetic results of orthognathic surgery has increased34.
Orthodontic treatment for orthognathic surgery can generally be divided into the following steps: orthodontic treatment before surgery, including arrangement of the dental arch and decompensation of the teeth; orthognathic surgery; and postsurgical orthodontic treatment for stable occlusion. Orthodontic treatment before surgery requires a relatively long treatment period of 12 months at least, during which the oral health, mastication, and facial esthetics of the patient can deteriorate567.
Recently, to fulfill the demand of patients for more rapid improvement in facial esthetics and to remedy a disadvantage of pre-surgery orthodontic treatment, a surgery-first orthognathic approach has been suggested. This method increases the satisfaction of patients by improving the esthetics with the first treatment and reduces total treatment time by minimizing the time required for orthodontic treatment after surgery. Additionally, effective decompensation can be attained by altering the relationship between the jaws and thus the strength of the tongue or lips8910. Furthermore, after surgery, the patient can benefit from accelerated teeth movement due to physiological changes in the jaws1112. However, there are difficulties in predicting the movement of teeth and instability of the jaw according to unstable occlusion.
Sagittal split ramus osteotomy (SSRO) of the mandible is a common surgery for various mandibular malformations including asymmetry. This surgery has the advantage of rapid recovery due to wide bone contact, and long-term outcomes have been reported in the literature.
Relapse after mandibular setback surgery in patients with mandibular prognathism remains a controversial issue 131415. Reports on the stability of orthognathic surgery have shown that mandibular setback surgery has a high relapse rate, although it is lower than that of maxillary downward positioning or transverse maxillary expansion. Additionally, since the surgery-first orthognathic approach does not involve presurgery orthodontic treatment, there is a risk of relapse due to unstable occlusion.
Thus, this study evaluated the stability after surgery using lateral cephalometric analyses pre- and postoperatively in mandibular prognathism patients who were treated with orthodontic treatment before surgery along with SSRO or a surgery-first orthognathic approach.
This study followed the Helsinki Declaration and was approved by Chosun University Dental Hospital Clinical Trial Center Institutional Review Board (CDMDIRB-1322-117). This study was conducted with patients who were diagnosed as skeletal class III malocclusion and underwent orthognathic surgery between January 2009 and June 2012 at Chosun University Dental Hospital (Gwangju, Korea). The study included 20 patients (10 males, 10 females, mean age 24.8 years) who underwent pre-surgery orthodontic treatment and 20 patients (10 males, 10 females, mean age 22.6 years) treated with a surgery-first orthognathic approach. Patients who received genioplasty and maxillary Le Fort I osteotomy and patients with mandibular chin point deviation greater than 5 mm were excluded. The criterion for the surgery-first approach was a pre-surgical orthodontic treatment without orthodontic alignment or leveling. The resin-wire splint was used in some of surgery-first patients without brackets for maxillomandibular fixation after surgery. Each patient underwent mandibular setback surgery via bilateral SSRO performed by a single surgeon. Semi-rigid fixation using miniplates was performed for all patients, and postsurgical maxillomandibular fixation with elastics was performed after surgery for 2 weeks. After the removal of maxillomandibular fixation, physical therapy including elastic traction and mouth opening exercise were performed.
Pre-surgery (T0), immediately after surgery (T1, 2-4 weeks), and post-surgery (T2, after 1 year or at debonding), lateral cephalometric radiograph images were obtained using a cephalometric X-ray machine (PM2002 EC Proline; PLANMECA, Helsinki, Finland). During radiographic imaging, the patients remained in an upright posture while maintaining the Frankfort horizontal (FH) plane parallel to the ground, and images were obtained during maximum intercuspation. One of the researchers used Photoshop to overlap lateral cephalometric radiograph images (Fig. 1, 2, 3), created projections, and arranged measurement items by determining landmarks.
Lateral cephalometric radiograph images at T0, T1, and T2 were analyzed to examine the changes in horizontal and vertical movement of the B point and pogonion (Pog) point. (Table 1) To measure the horizontal movement of the mandible using sella (S) as a reference, a standard perpendicular line (S-perp) perpendicular to the FH plane was constructed. From this S-perp, the horizontal distance between the B point and Pog point was measured. For the vertical movement of the mandible, the vertical distance between the B point and Pog point was measured using the FH plane as a reference. Additionally, the differences between T0 and T1 at B point and Pog point were considered the setback amounts, and the difference between T1 and T2 was regarded as the amount of postoperative relapse.
Statistical analyses of measured distances at T0, T1, and T2 were performed, and the significance of the change in each group was determined using a paired t-test. A P-value less than 0.01 was considered statistically significant. The database and statistical analysis was performed using SPSS Statistics ver. 12.0 (SPSS Inc., Chicago, IL, USA).
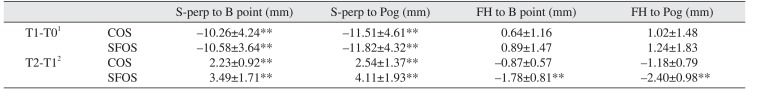
The mean moving distances of the mandible after orthognathic surgery from T0 to T1 using the B point as a reference were −10.26±4.24 mm (P<0.01) posteriorly and 0.64±1.16 mm (non-significant; NS) inferiorly; when using Pog point as reference, the moving distances were −11.51±4.61 mm (P<0.01) posteriorly and 1.02±1.48 mm (NS) inferiorly. (Table 2)
The relapse amounts after surgery from T1 to T2 with B point as reference were 2.23±0.92 mm (P<0.01) anteriorly and −0.87±0.57 mm (NS) superiorly; when using Pog point as reference, moving distances were 2.54±1.37 mm (P<0.01) anteriorly and −1.18±0.79 mm (NS) superiorly.
The mean moving distances of the mandible after orthognathic surgery from T0 to T1 with the B point as a reference were −10.58±3.64 mm (P<0.01) posteriorly and 0.89±1.47 mm (NS) inferiorly; when using the Pog point as a reference, moving distances were −11.82±4.32 mm (P<0.01) posteriorly and 1.24±1.83 mm (NS) inferiorly.(Table 2)
The relapse amounts during orthodontic treatment after surgery from T1 to T2 with the B point as a reference were 3.49±1.71 mm (P<0.01) anteriorly and −1.78±0.81 mm (P<0.01) superiorly; when using the Pog point as a reference, moving distances were 4.11±1.93 mm (P<0.01) anteriorly and −2.40±0.98 mm (P<0.01) superiorly.
Traditional orthodontic treatment before surgery in patients with skeletal class III malocclusion who require orthognathic surgery removes dentoalveolar compensation and reveals the actual skeletal imbalance, allowing sufficient movement to be made during the surgery. However, patients required 12 to 24 months of orthodontic treatment and 5 to 11 months of post-surgery orthodontic treatments, and the likelihood of oral health deterioration and sociopsychological problems increased as the treatment period extended 56716.
Recently, to satisfy the demands of patients for more rapid improvement of facial esthetics and to resolve the disadvantages regarding the pre-surgery orthodontic treatment, the surgery-first orthognathic approach has been emphasized. This method increased patient satisfaction by obtaining esthetic improvement at the beginning of treatment. The surgery-first orthognathic method allows the physiological movement of teeth during post-surgery orthodontic treatment by altering the relationship between the jaws and the strength of soft tissues8910. The orthodontic treatment period was reduced due to a regional acceleratory phenomenon that occurs after surgery. In other words, activation of osteoclasts and acceleration of bone metabolism after surgery accelerated the movement of teeth for 3 to 4 months12.
The major disadvantage of the surgery-first orthognathic approach is the unstable occlusion that occurs postoperatively. Consequently, at least three stable occlusion points of the upper and lower dentitions are required for the surgery-first approach17. For the surgery-first orthognathic approach, application of a thicker wafer than that used in traditional surgical orthodontic treatment is necessary for a long time, and occlusal adjustment and formation of an occlusal stop with resin are necessary to improve unstable occlusions. Liou et al.18 recommended the postsurgical usage of a chin cap to prevent skeletal relapse by unstable occlusion. The maximal occlusion stability was obtained by adding resin onto the occlusal surface of the molar area after removing the wafer.
Another disadvantage of the surgery-first orthognathic approach is the difficulty in predicting the results. As a result of post-surgical orthodontic treatment, significant movements of teeth and jaws have been observed. Thus, to predict and evaluate these variables in pre-surgical planning, setting the occlusion after surgery through a model surgery is necessary919, and expected problems should be evaluated by three-dimensional mock surgery using computed tomography20.
Studies of horizontal relapse after mandible surgery for skeletal class III malocclusion have reported various results, including amount of setback of the mandible 4.80 to 8.70 mm (mean, 6.49 mm), anterior movement 0.60 to 2.87 mm (mean, 1.49 mm), and relapse rate 7.1% to 51.4% (mean, 22.6%)21. Numerous reports have suggested that various factors affect the relapse after orthognathic surgery, including locational change of the condyle, alterations of connective tissue such as masticatory muscle and periosteum, amount of movement of the mandible, and method of fixation. However, the actual cause of relapse after surgery remains unclear13
141521. The factors such as large overbite, a deeper curve of Spee, a greater negative overjet, and amount of setback can decrease stability of a surgery-first approach for the correction of skeletal class III malocclusion22.
To evaluate relapse after orthognathic surgery, most studies have used a standard parallel plane with the FH plane or SN plane rotated clockwise 7° at the nasion point and used a standard perpendicular plane that passed through a landmark above and perpendicular to the standard parallel plane. The SN plane is useful in evaluating the craniofacial relationship, and the FH plane is appropriate for assessing the face23; however, because of the low reproducibility and accuracy of the porion and orbitale, reference points of the FH plane, the SN plane is used as a standard in many studies24. Photoshop was utilized in this research to overlap lateral cephalometric radiographic images. Thus, errors were reduced, and an accurate movement pattern of the landmark was determined regardless of the standard plane used. As a result, the amount of mean setback movements of the mandible in the conventional orthognathic group and surgery-first orthognathic approach group at B point were −10.26±4.24 mm and −10.58±3.64 mm, respectively, and at Pog point were −11.51±4.61 mm and −11.82±4.32 mm; no significant difference was observed. However, the horizontal anterior movement amounts at T1 to T2 in the conventional orthognathic group were 2.23±0.92 mm at the B point and 2.54±1.37 mm at the Pog point; in the surgery-first orthognathic approach group, these were 3.49±1.71 mm at the B point and 4.11±1.93 mm at the Pog point. The surgery-first orthognathic approach group exhibited a greater amount of mandible relapse during orthodontic treatment. Although the conventional orthognathic group did not show significant changes in the amount of vertical movement at T0, T1, and T2, the surgery-first orthognathic approach group showed inferior movements of 0.89±1.47 mm (NS) at the B point and 1.24±1.83 mm (NS) at the Pog point from T0 to T1 and superior movements of −1.78±0.81 mm at the B point and −2.40±0.98 mm at the Pog point at T1 to T2. The vertical dimension was increased to avoid occlusional interference of the upper and lower molars at T1. As the vertical dimension of occlusion was decrease during orthodontic treatment after surgery, the mandible was moved anterosuperiorly by the counter-clockwise rotation of the mandible.
Light crowding and little discrepancy in arch width or weak skeletal class III without extraction are the most probable indications for use of the surgery-first orthognathic approach1822. Additionally, reduced skeletal stability due to extraction and potential incomplete enclosure of the tooth extraction space should be considered. If extraction is required in cases of skeletal class III malocclusion with asymmetry, achieving decompensation and space closure by pre-surgical orthodontic treatment is necessary. Minimum orthodontic treatment before surgery in skeletal class II patients is important to avoid crossbite, because advancing a retrognathic mandible will create a temporary anterior crosstie25.
To obtain an ideal result using the surgery-first orthognathic approach, an accurate analysis of each case with the assistance of an oral and maxillofacial surgeon and orthodontist and consideration of the many factors that could affect the result of the surgery are necessary. In an occlusion setting after surgery, the movement of teeth to minimize occlusion interference, mandibular movement due to counterclockwise rotation of the mandible after surgery, face shape, and the shape of the dental arch should be considered. In addition, consistent skeletal stabilization during post-surgical orthodontic treatment must be secured using an elastic or chin cup.
Patients with skeletal class III malocclusion who were treated with a surgery-first orthognathic approach showed greater horizontal and vertical relapses due to the counter-clockwise rotation of the mandible than did patients treated with orthodontic treatment before surgery. Since these relapses can affect facial alteration after surgery, careful examination is necessary, and the amount of mandibular movement and skeletal stabilization after surgery considering relapse should be planned thoroughly.
References
1. Kang HK, Ryu YK. A study on the prevalence of malocclusion of Yonsei university students in 1991. Korean J Orthod. 1992; 22:691–701.
2. Baik HS, Han HK, Kim DJ, Proffit WR. Cephalometric characteristics of Korean Class III surgical patients and their relationship to plans for surgical treatment. Int J Adult Orthodon Orthognath Surg. 2000; 15:119–128. PMID: 11307422.
3. Bos A, Hoogstraten J, Prahl-Andersen B. Expectations of treatment and satisfaction with dentofacial appearance in orthodontic patients. Am J Orthod Dentofacial Orthop. 2003; 123:127–132. PMID: 12594417.

4. Juggins KJ, Nixon F, Cunningham SJ. Patient- and clinician-perceived need for orthognathic surgery. Am J Orthod Dentofacial Orthop. 2005; 128:697–702. PMID: 16360908.

5. Dowling PA, Espeland L, Krogstad O, Stenvik A, Kelly A. Duration of orthodontic treatment involving orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1999; 14:146–152. PMID: 10686838.
6. Luther F, Morris DO, Hart C. Orthodontic preparation for orthognathic surgery: how long does it take and why? A retrospective study. Br J Oral Maxillofac Surg. 2003; 41:401–406. PMID: 14614870.

7. Proffit WR, White RP, Sarver DM. Contemporary treatment of dentofacial deformity. St. Louis: Mosby;2003.
8. Nagasaka H, Sugawara J, Kawamura H, Nanda R. “Surgery first” skeletal Class III correction using the Skeletal Anchorage System. J Clin Orthod. 2009; 43:97–105. PMID: 19276579.
9. Baek SH, Ahn HW, Kwon YH, Choi JY. Surgery-first approach in skeletal class III malocclusion treated with 2-jaw surgery: evaluation of surgical movement and postoperative orthodontic treatment. J Craniofac Surg. 2010; 21:332–338. PMID: 20186090.
10. Yu CC, Chen PH, Liou EJ, Huang CS, Chen YR. A surgery-first approach in surgical-orthodontic treatment of mandibular prognathism--a case report. Chang Gung Med J. 2010; 33:699–705. PMID: 21199616.
11. Yaffe A, Fine N, Binderman I. Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery. J Periodontol. 1994; 65:79–83. PMID: 8133418.

12. Liou EJ, Chen PH, Wang YC, Yu CC, Huang CS, Chen YR. Surgery-first accelerated orthognathic surgery: postoperative rapid orthodontic tooth movement. J Oral Maxillofac Surg. 2011; 69:781–785. PMID: 21353934.

13. Trauner R, Obwegeser H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg Oral Med Oral Pathol. 1957; 10:677–689. PMID: 13441284.
14. Dal Pont G. Retromolar osteotomy for the correction of prognathism. J Oral Surg Anesth Hosp Dent Serv. 1961; 19:42–47. PMID: 13719390.
15. de Villa GH, Huang CS, Chen PK, Chen YR. Bilateral sagittal split osteotomy for correction of mandibular prognathism: long-term results. J Oral Maxillofac Surg. 2005; 63:1584–1592. PMID: 16243174.

16. Proffit WR, Turvey TA, Phillips C. Orthognathic surgery: a hierarchy of stability. Int J Adult Orthodon Orthognath Surg. 1996; 11:191–204. PMID: 9456622.
17. Villegas C, Uribe F, Sugawara J, Nanda R. Expedited correction of significant dentofacial asymmetry using a “surgery first” approach. J Clin Orthod. 2010; 44:97–103. PMID: 20552809.
18. Liou EJ, Chen PH, Wang YC, Yu CC, Huang CS, Chen YR. Surgery-first accelerated orthognathic surgery: orthodontic guidelines and setup for model surgery. J Oral Maxillofac Surg. 2011; 69:771–780. PMID: 21257249.

19. Bailey L, Cevidanes LH, Proffit WR. Stability and predictability of orthognathic surgery. Am J Orthod Dentofacial Orthop. 2004; 126:273–277. PMID: 15356484.

20. Jacobs JD, Sinclair PM. Principles of orthodontic mechanics in orthognathic surgery cases. Am J Orthod. 1983; 84:399–407. PMID: 6579841.

21. Costa F, Robiony M, Politi M. Stability of sagittal split ramus osteotomy used to correct Class III malocclusion: review of the literature. Int J Adult Orthodon Orthognath Surg. 2001; 16:121–129. PMID: 11482290.
22. Ko EW, Lin SC, Chen YR, Huang CS. Skeletal and dental variables related to the stability of orthognathic surgery in skeletal Class III malocclusion with a surgery-first approach. J Oral Maxillofac Surg. 2013; 71:e215–e223. PMID: 23455415.

23. Downs WB. Variations in facial relationships; their significance in treatment and prognosis. Am J Orthod. 1948; 34:812–840. PMID: 18882558.

24. Burstone CJ, James RB, Legan H, Murphy GA, Norton LA. Cephalometrics for orthognathic surgery. J Oral Surg. 1978; 36:269–277. PMID: 273073.
25. Kim JH, Mahdavie NN, Evans CA. Guidelines for “Surgery First” orthodontic treatment. In : Bourzgui F, editor. Orthodontics: basic aspects and clinical considerations. Rijeka, Croatia: InTech;2012. p. 265–300.
Fig. 1
Superimposition of lateral cephalograms at the pre-surgery stage (T0; blue) and immediately after surgery (T1; red): B point and pogonion (Pog) point move backward and downward.
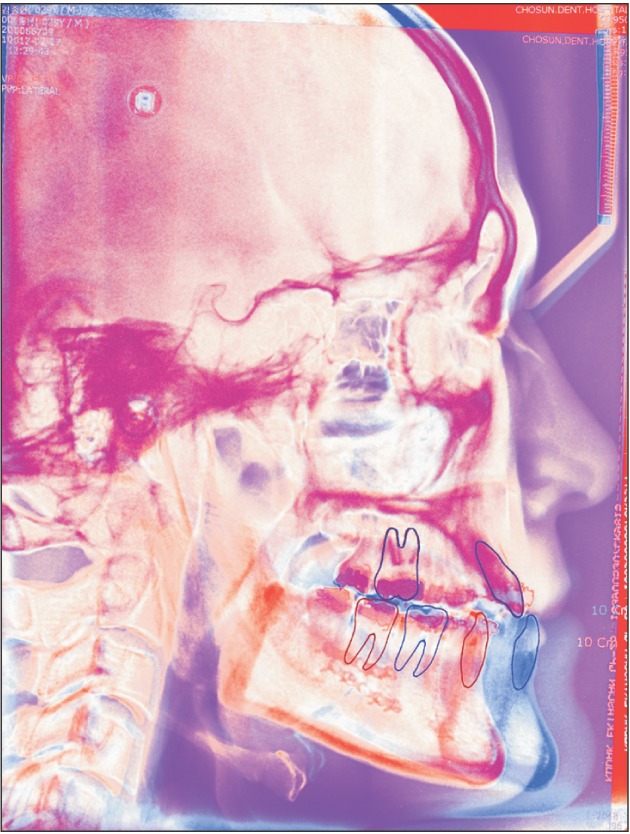
Fig. 2
Superimposition of lateral cephalograms immediately after surgery (T1; blue) and long-term after surgery (T2; orange): B point and pogonion (Pog) point move anterior and upward.

Fig. 3
Landmarks, reference planes, and measurements for cephalometric analysis. The landmarks: sella (S), porion (Por), orbitale (Or), pogonion (Pog), B point. The reference plane: Frankfort horizontal (FH) plane (Or-Por), perpendicular line of S to FH plane (S-perp). The linear measurements (mm): a, S-perp to Pog; b, S-perp to Pog; c, FH to B point; d, FH to Pog.
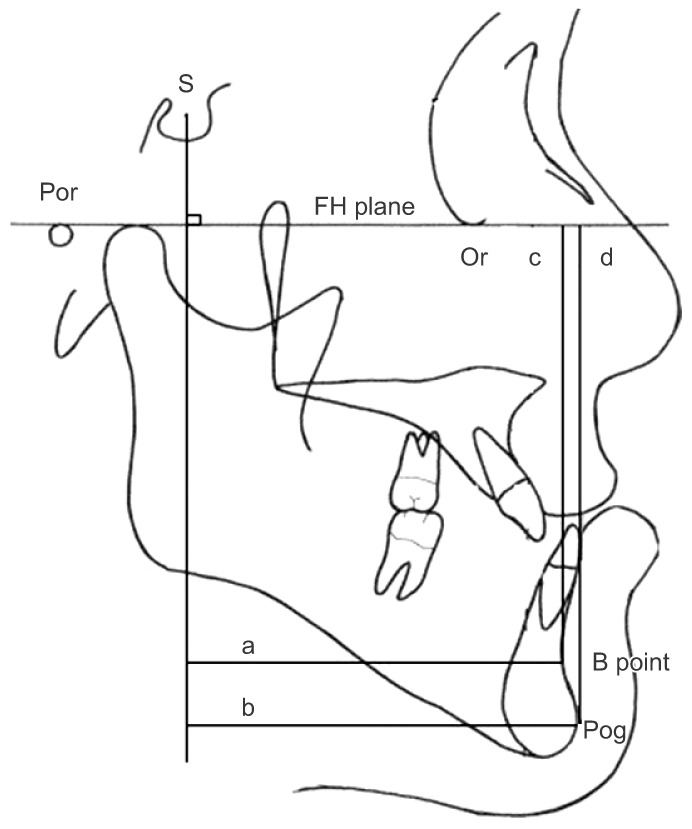
Table 1
Horizontal and vertical positions of B point and pogonion (Pog) at the pre-surgery (T0), immediately after surgery (T1), and long-term post-surgery (T2) stages
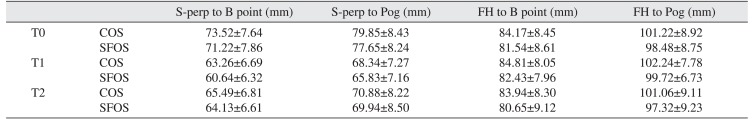
Table 2
Post-surgical change (T1-T0) and relapse change (T2-T1) of the B point and pogonion (Pog)




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download