I. Introduction
The fear about dental treatment is relatively high, and minor oral surgeries such as surgical extraction of third molar give much anxiety and stress to patients. To solve this problem, a variety of stress reduction protocols and intravenous conscious sedation (IVS) methods have been developed
12. Among these, IVS using midazolam (MDZ) has been used widely in medical areas, including the dental department, because MDZ affects the vital signs minimally, easily imparts the adequate calming effect, causes intraoperative amnesia, and provides quick recovery time due to the short half-life of this medicine
34.
Although MDZ is a relatively safe medication, side effects such as respiratory depression can occur and recovery time after surgery may increase when overdose is injected
56. Therefore, the clinic, in which the surgeon is responsible for the whole process of sedation because the anesthesiologist is not resident, may prefer to inject a relatively low dose only once for safety. However, if the degree of sedation is insufficient, the operation cannot be performed normally, and additional medication needs to be administered during the operation. This causes increase of total operation time and dissatisfaction of both operator and patient. However, to date, there is a lack of research on the factors involved in the administration of additional medications due to insufficient sedation after initial dose, and what contributes to patient satisfaction.
In this study, we revealed factors related to additional administration of MDZ in the cases of insufficient sedation after initial dose. In addition, factors related to patient satisfaction were also analyzed. The ultimate goal of this study was to provide the guideline for adequate sedation with the minimum dose of MDZ.
Go to :

II. Materials and Methods
This study was approved by the Institutional Review Board of SMG-SNU Boramae Medical Center, Seoul, Korea (IRB No. 26-2014-139), and followed the Declaration of Helsinki on medical protocol and ethics. This is a case-control study that compared the case group with insufficient sedation to the control group with adequate sedation after infusion of only the initial dose of MDZ, and that compared the case group with dissatisfaction to the control group with satisfaction with the treatment under conscious sedation. The inclusion criteria were patients with American Society of Anesthesiology (ASA) physical status I, who have received surgical extraction of both lower third molars with or without simple extraction of upper third molars under IVS using MDZ in SMG-SNU Boramae Medical Center from August 2013 through July 2016. The exclusion criteria were patients with systemic diseases of ASA physical status II to V, renal or hepatic diseases that can affect the metabolism of MDZ, medications having the effect on cytochrome P 450 enzymes or gamma-aminobutyric acid receptors, histories of the recent use of sedatives, no presence of pericoronitis around the impacted third molar, or surgical cases with a total time of more than one hour.
1. Sedation protocol and clinical setting
The crystalloid solution (Plasma Solution A; CJ Health Care, Seoul, Korea) was administered through an 18-gauge intravenous line at a speed of 100 mL/h. After the confirmation of no allergic response through a skin test, a 1 g prophylactic antibiotics (Yamatetan Injection; Jeil Pharmaceutical, Seoul, Korea) was injected. Each patient's peripheral oxygen saturation (SpO
2), bispectral index score (BIS), heart rate, and noninvasive blood pressure (NIBP) were monitored during the whole sedation procedure. A 30 mg opioid analgesic (Pethidine HCl Injection; Bio & Chemical R&D, Seoul, Korea) was given for 30 seconds. The main sedative agent MDZ (Midazolam Injection; Bukwang Pharmaceutical, Seoul, Korea) was administered at the speed of 200 mg/h using an infusion pump (Syramed uSP 6000 syringe pump; Arcomed AG, Regensdorf, Switzerland) intravenously after the dose was determined according to body mass index (BMI) and weight. On the basis of BMI, patients were categorized as underweight (BMI <18.00 kg/m
2), normal weight (BMI 18.00–24.99 kg/m
2), or overweight (BMI ≥25.00 kg/m
2); according to this categorization, MDZ of 0.05 mg/kg was administered for underweight patient, 0.06 mg/kg for normal weight patient, or 0.07 mg/kg for overweight patient. Five minutes after the MDZ administration, the surgeon verified the slurred speech and drooping eyes of the patient, and performed the routine surgical aseptic draping. The surgery began 5 minutes after the injection of the local anesthetic agent (Lidocaine HCl 2% injection 1:100,000 epinephrine; Huons, Seoul, Korea). If the patient responded readily to his or her name being spoken in a normal tone and complained of great anxiety around the beginning of surgery, these signs were regarded as insufficient sedation, and an additional dose of 1 mg MDZ was administered at the same speed of the initial dosage. If the sedation was still insufficient 5 minutes after additional administration, the second additional administration of MDZ was carried out. If it was still insufficient, the same procedure was repeated, with the maximum number of additional administrations limited to four. On the contrary, if SpO
2 decreased below 95 and the patient did not respond after mild prodding or shaking, these signs were regarded as excessive sedation, and the surgeon awakened the patient by giving painful trapezius squeeze. In case this procedure had no effect, a 0.2 mg flumazenil (Flunil Injection; Bukwang Pharmaceutical) was administered for 15 seconds. If there was no effect after 1 minute, an additional 0.1 mg of flumazenil was administered. If this also did not work, the cardiovascular resuscitation procedure was initiated. The patient was discharged after the confirmation of having 9 points of the Aldrete post-anesthesia recovery score
7. The whole sedation protocol was controlled by one operating team, and all surgeries were performed randomly by one of the two surgeons with at least five years of clinical experience as specialists in oral and maxillofacial surgery.
2. Variables
The predictor variables were sex, age, BMI, sleeping time ratio, dental anxiety score (DAS), Pederson scale
8, and initial dose of MDZ. BMI was calculated in weight (kg) divided by the square of the height (m). The information about sleeping time was acquired by asking the patient. The sleeping time ratio was defined as the ratio of the amount of sleep the night before the operation to the average amount of sleep in patient's daily life. DAS was collected by a questionnaire
9. DAS was categorized into one of two groups: lower dental anxiety, 4 to 12 points; higher dental anxiety, over 12 points. Pederson scale was calculated in panoramic radiograph by one independent investigator, and the average of both mandibular third molars was used as the final value.
The outcome variables were whether the additional MDZ was administered, observer's assessment of alertness/sedation scale (OAA/S)
10, the level of amnesia with the operation, patient satisfaction, SpO
2, BIS, heart rate, systolic and diastolic NIBP. OAA/S was recorded in the range of 0 to 5 points on the moment 20 minutes after local anesthesia. For information of amnesia, the patient was asked about whether the patient remembered three moments within the whole sedation procedure; injection of local anesthesia, a certain point in the operation itself, and the comment of the operator signaling the start of suturing. If the patient remembered each moment, each amnesia point was recorded as 0, and if not, the point was recorded as 1. The total amnesia score was the sum of each point. Immediately after being asked about amnesia, the patient was also asked about the degree of satisfaction; very dissatisfied, dissatisfied, moderate, satisfied, or very satisfied. Each rating was converted to a point, from 1 to 5. This scale was categorized into one of the two groups; dissatisfaction (from 1 to 3 points) or satisfaction (4 or more points). BIS was recorded with an electroencephalographic sensor (BIS Quatro Sensor; Covidien, Mansfield, MA, USA) attached to the forehead of the patient using an electroencephalographic monitoring system (BIS Vista Monitoring System; Aspect Medical Systems, Norwood, MA, USA). SpO
2, BIS, heart rate, systolic and diastolic NIBP were monitored continuously during the operation, and the records of five moments of each procedure were extracted and used for statistical analysis; the moment right before MDZ administration (T0), the moment 5 minutes after MDZ administration (T1), the time of injection of the local anesthetic agent (T2), the moment 20 minutes after local anesthesia (T3), and the time of the first stitch (T4).
3. Statistical analysis
Pearson's chi-square tests or Fisher's exact tests for categorical variables and Student's t-tests for continuous variables were conducted. Multivariable logistic regression tests were performed to identify factors related to additional administration of MDZ and patient satisfaction. A goodness-of-fit test and model selection were executed using the Hosmer-Lemeshow goodness-of-fit test and the Akaike information criterion. All statistical analyses were performed using the IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA), and probabilities less than 0.05 were considered to be statistically significant.
Go to :

IV. Discussion
IVS using MDZ helps patients have comfortable treatment and surgeons concentrate on the operations. However, there are occasionally cases that require additional dosing of sedative during surgery due to the lack of sedation. In an outpatient setting where an anesthesiologist does not reside, additional dosing puts a lot of pressure on surgeons because it might increase the complication of sedative itself and recovery time after sedation treatment. Therefore, from the surgeon's point of view, it is helpful to identify factors related to the need for extra doses before initiation of treatment. Ultimately, one of the major purposes of sedation is to satisfy the patient with the whole process of treatment. Thus, from the patient's point of view, it is helpful to identify factors related to patient satisfaction with the sedation treatment. In this study, several factors affecting addition of sedative dose and satisfaction of patient were analyzed. These factors have not been studied previously in the areas of oral and maxillofacial surgery.
In the previous studies, the initial doses of MDZ varied from 0.03 to 0.1 mg/kg, and the methods of sedation were also diverse, for example, titration until the emergency of signs like ptosis or slurred speech, continuous administration of small doses after initial doses, or dose control by patients themselves
11121314. In this study, the authors have designed the sedation protocol as the initial slow administration of the customized dose combined by an additional dose as necessary under the surgeon's decision. In most previous studies, the initial doses were adjusted by the body weight only; however, several other factors were also related to the adequate doses. Among these, higher BMI cases needed more doses of sedative agents and showed shorter recovery time than lower BMI cases
1516. Moreover, in overweight patients, the blood concentrations of sedatives were lower than in normal or underweight patients because of the high central and peripheral volumes of distribution; therefore, a longer time for sedatives to reach the blood concentration was needed for sufficient sedations
17. On the basis of these studies, the authors designed the sedation protocol that determined the initial dose according to three ranges of BMI
18. In the cases of severe overweight patients with concomitant systemic diseases like fatty liver, the clearances of MDZ could be affected and the dose reduction was essential
19. Therefore, the patients with these kinds of systemic diseases were excluded in this study.
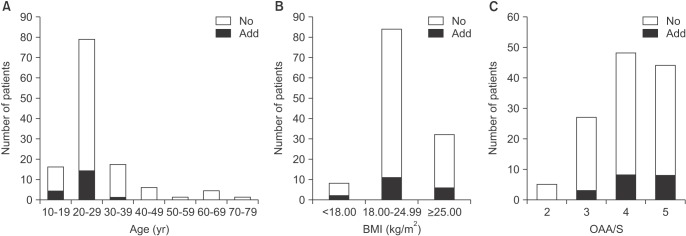
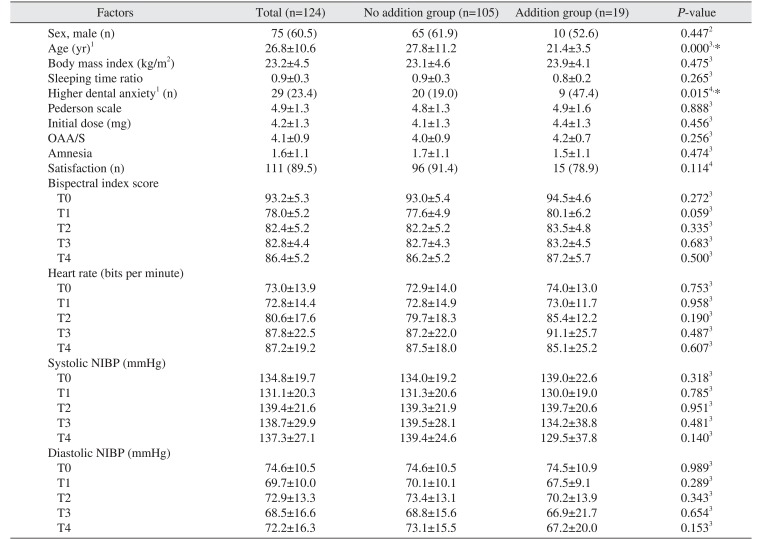
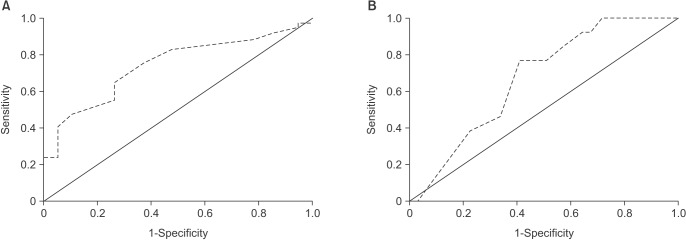
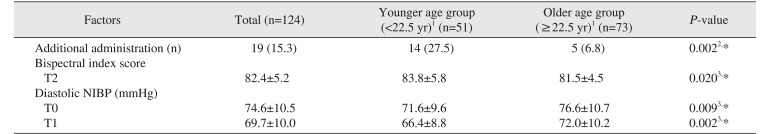
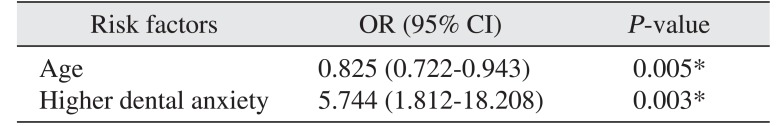
The adequate levels of sedation were observed in most patients of this study; however, 19 patients (15.3%) had additional administration of MDZ because of insufficient sedation. Among them, 9 patients had the additional administration more than once. Additional administration was related with the lower age; in other words, decreasing age needed more dosages. This could be a result of increased metabolism or decreased sensitivity to the sedatives in the younger patient. Czwornog and Austin
20 also reported that patients with low age and female gender needed a greater dose of MDZ for adequate sedation. Although there were no direct relationship between sex and additional administration of MDZ in the present study, OAA/S of women was larger than men (4.3±0.7 vs. 3.9±0.9;
P=0.028), which proved the relation between sex and the level of consciousness. Higher dental anxiety was related to additional administration. Seto et al.
21 also reported that the dose of sedative agents increased with increasing fear of the dental treatment. In addition, women showed higher dental anxiety than men in this study (36.7% vs. 14.7%;
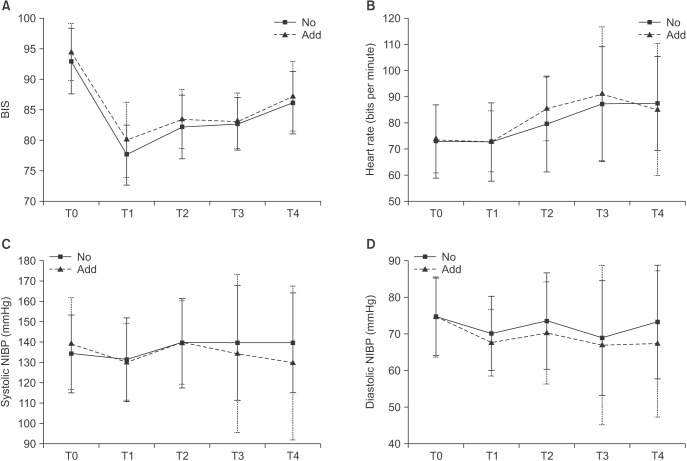
P=0.005). Taken together these factors, for sedation of young women patient with higher dental anxiety, increasing the initial dose or early administration of additional dose may help reduce the delay of operation due to waiting time for onset of effect of additional sedatives. Furthermore, with decreasing age, BIS on T2 increased in this study. The time of additional administration was around the start of operation after the injection of the local anesthesia, therefore, BIS during local anesthesia may be an indirect reference for determining whether to administer additional doses.
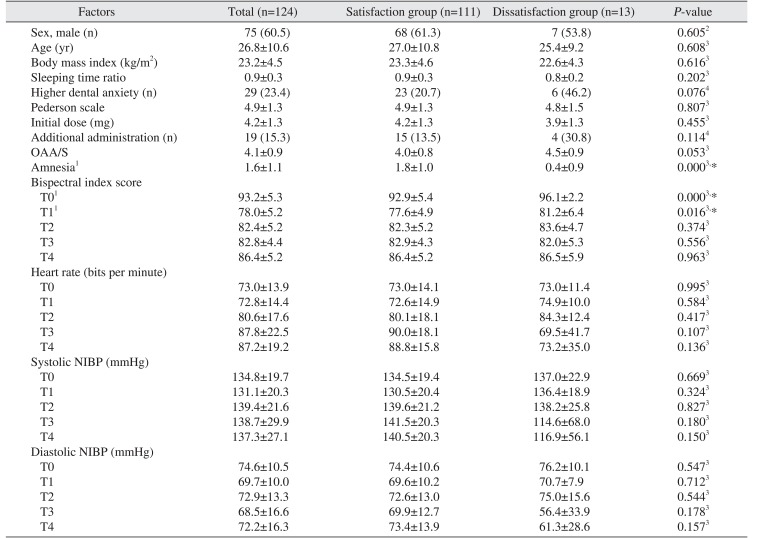
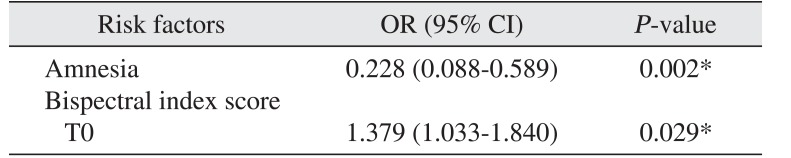
The subjective factors, such as the postoperative satisfaction, are also important for evaluating the adequacy of sedation. In this study, the average satisfaction score was 4.5±0.8 on a five-point scale, and 89.5% of patients were very satisfied or satisfied with the treatment under sedation. Amnesia during the operation and BIS on T0 affected satisfaction significantly. High level of amnesia resulted in high satisfaction of patients. Intraoperative amnesia is the marked characteristics of MDZ compared with other sedatives
12. In the present study the mean amnesia point was 1.6±1.1 on a three-point scale. Zacharias et al.
14 reported that 70% of patients experienced amnesia using the continuous infusion of MDZ. Meanwhile, Levitzky et al.
22 reported that old age was related with high satisfaction; however, there was no significant relationship between these two factors in this study. High BIS on T0 may reflect the high nervousness about the surgery. It implies that preoperative relaxation therapy is as important as sedation procedure itself
23.
There have been several methods measuring the state of consciousness during sedation. Among these, BIS based on electroencephalogram has been used frequently
2425. The state of consciousness reading BIS under 60 is regarded as the general anesthesia, from 61 to 70 as deep or moderate sedation, and from 71 to 90 as light or moderate sedation
262728. In this study, BIS was also used to evaluate the level of consciousness. Bower et al.
29 reported that 82 of BIS value was adequate for the endoscopy. Therefore, the authors set the target value of BIS as 80, and actually values of BIS maintained around 80 through all operational procedures. Other than the objective methods like BIS, subjective methods like OAA/S or Ramsay score based on observation of operators have been used
10. Chisholm et al.
26 reported that the OAA/S and Ramsay scores showed a similar tendency and had the positive relationship with BIS. In this study, the target value of OAA/S was 4, and this goal was achieved in most patients.
This case-control study had several limitations. First, there may have been performance bias. Although the sedation protocol and clinical setting have been established, not all extraction procedures of the two surgeons could be fully standardized. Second, confounding bias may have influenced the results. Although the data were controlled via multivariable logistic regression analysis after data collection, there may be other confounding factors that were not collected, such as exact total operation time, the presence of temporomandibular joint disorder, the amount of maximum mouth opening, elasticity of facial skin. Third, there may have been information bias. In this study, only previous medical records were used. Thus, errors that occurred at the time these records were made could not be detected. Fourth, there may have been over-interpretation. Since this study was a case-control study, the odds ratio was presented instead of the relative risk. In addition, the rate of additional administration of MDZ was 15.3%, and dissatisfaction rate was 10.5%, which was comparatively high. Thus, this study provides a weaker basis for causality than a cohort study does. Consequently, the odds ratio calculated in this study was predicted to be higher than the actual relative risk. Fifth, for more accurate respiratory monitoring, measurement of end tidal pressure of carbon dioxide using capnography was required rather than SpO2, although there were no patients with respiratory depression in this study. Further research using capnography is needed. Finally, the operation using an electric drill or saw, such as block bone graft, might need higher intensity of sedation and larger additional dose than surgical tooth extraction. Further research is needed on the sedation treatment of more aggressive surgery.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download