Abstract
Maxillary sinus lift for dental implant installation is a well-known and versatile technique; new techniques are presented based on the physiology of intrasinus bone repair. The aim of this review was to determine the status of graftless maxillary sinus lift and analyze its foundations and results. A search was conducted of the literature between 1995 and 2015 in the Medline, ScienceDirect, and SciELO databases using the keywords “maxillary sinus lift,” “blood clot,” “graftless maxillary sinus augmentation,” and “dental implant placement.” Ten articles were selected for our analysis of this technique and its results. Despite the limited information, cases that were followed for at least six months and up to four years had a 90% success rate. Published techniques included a lateral window, elevation of the sinus membrane, drilling and dental implant installation, descent of the membrane with variations in the installation of the lateral wall access and suturing. The physiology behind this new bone formation response and the results of the present research were also discussed. We concluded that this is a promising and viable technique under certain inclusion criteria.
The maxillary sinus lift is a well-known and versatile technique. It is widely used today to place implants in the posterior maxillary under different installation conditions. The maxillary sinus lift was initially proposed by Tatum1 and was then perfected by Boyne and James2 when they incorporated an iliac crest bone graft to attain bone formation and intrasinus stability. Since then, different materials and techniques have been explored for the installation of implants in the maxillary sinus area, demonstrating the success of these implants.
The anatomic variability of the maxillary sinus has demanded adaptation to different constraints. Mendoza et al.3 reported that a progressive increase in maxillary sinus volume may on some levels be associated with the amount of tooth loss, whereas De Moraes et al.4 demonstrated the relationship between different sinus volumes and the amount of fillings needed to cover a dental implant.
Proposed options for maxillary sinus lift include zygomatic implants and the use of angulated implants, which can adapt to atrophy of the posterior maxillary sector56. However, the maxillary sinus lift continues to be a viable technique with high success rates.
A wide variety of bone grafts have been used in the maxillary sinus with relative success7. In their study of 692 patients and 952 sinus lifts, Chiapasco et al.8 reported a reconstruction success rate that ranged from 93% to 100%, while the success of installed implants reached 95%. Olate et al.9 showed that in 91 sinus floor elevation surgeries, there were no significant differences in the results obtained after the use of different fillings, even in implants that were installed at different times.
Our understanding of new intrasinus bone formation, however, underwent no great advances until some studies suggested the possibility of new bone formation from a blood clot without the need for bone grafting10.
The aim of this review is to know the technique of graftless sinus floor reconstruction and to determine the physiology behind this technique.
A literature review was designed using a search of articles published between 1995 and 2015 in Medline, ScienceDirect, and SciELO using the terms “maxillary sinus lift,” “blood clot,” “graftless maxillary sinus augmentation,” and “dental implant placement.”
The inclusion criteria were 1) papers published in Spanish or English, 2) studies conducted in humans, and 3) graftless maxillary sinus lifts performed with a defined technique. The exclusion criteria were as follows: 1) use of autogenous bone or biomaterials in the maxillary sinus lift and 2) articles that were literature reviews or letters to the editor.
The selected publications were analyzed on the basis of the type of surgery, follow-up and implant stability, as well as on the anatomical conditions of the maxillary sinus as described in the article. All data were analyzed using Microsoft Excel ver. 2011 14.7.5 (Microsoft, Redmond, WA, USA) spreadsheets. Descriptive statistics were performed for the results analysis.
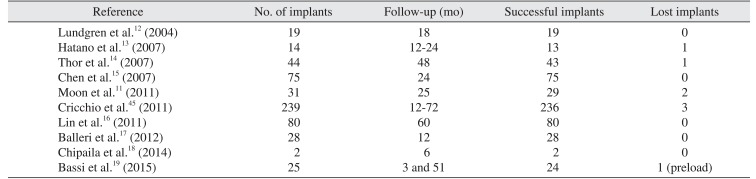
Ten articles were selected for this review; all pertained to studies conducted in humans. In all articles, implantation was carried out at the same time as lateral window maxillary sinus lift.
In nine articles, the follow-up included computed tomography alone; only one article11 used imaging in conjunction with a histological analysis of the newly formed bone. In five studies, both the sites of the sinus lift and the implant had adjacent teeth, whereas the area was completely edentulous in the other five.(Table 1)
Lundgren et al.12 performed graftless sinus lifts in 11 patients, installing 19 implants immediately, of which no failures were reported. Hatano et al.13 placed 14 implants in 6 patients using venous blood extracted from the patients as filling and indicated the failure of only 1 implant.
Thor et al.14 performed graftless sinus lifts in 20 patients and installed a total of 44 implants, of which only one failed; new bone formation with an average height of 6.5 mm was also observed. In a study conducted by Chen et al.15 where 75 implants were installed as previously described, there was a 100% implant success rate; an average vertical bone increase of 4.5 mm was also observed.
In studies by Lin et al.16, Balleri et al.17, and Chipaila et al.18, a 100% implant success rate was observed, whereas in the prospective study by Bassi et al.19, only one of the 25 implants was lost.
The analyzed articles revealed interesting results regarding new bone formation. Bassi et al.19, showed 7.2 mm in bone increase at the first measurement (3 months after surgery) and a decrease of 1.57 mm at 51 months after surgery, with a final increase of 5.63 mm. Lin et al.16 reported 7.24 mm of gained bone height at 2 years and 7.44 mm at 5 years postoperatively. Thor et al.14 showed a mean bone height of 6.5 mm 4 years after implant installation. Chen et al.15 determined that patients experienced 4.5 mm in bone formation after 2 years. These measurements were obtained using computed tomography and indicated a good response in bone formation because they were greater than 4.5 mm on average.
Different treatment options exist for elevation of the sinus floor. Crestal access and lateral window approaches are the most frequently used in current implantology20. Alternatives that incorporate balloon installation and endoscopic techniques have also been described, but they have failed to offer the cost-effectiveness ratio of the previously mentioned options21.
Maxillary sinus pneumatization, or an increased volume in the maxillary sinus after tooth loss, has been previously described and remains controversial22; the conditions under which pneumatization occurs determine the need to increase intrasinus volume and also the need for reconstruction.
Intrasinus autogenous grafts have been successful since their inception. One of the disadvantages of this approach lies in the reduction in grafted volume over time and also in the need for a second surgical site for bone extraction. Arasawa et al.23 conducted a study on 11 maxillary sinuses where each was filled with bone extracted from the iliac crest, and they observed that there was close to a 24% loss in grafted volume during a 12-month period; all fillings fully covered the implant. The most important condition in this reconstruction is that the autogenous bone graft, when integrated into the receptor bed, must be subject to bone remodeling, where bone resorption is part of the remodeling24. After implant is covered by grafted bone, osseous remodeling will be in contact with the functional area (body) of the implant; therefore, is not necessary to maintain the grafted bone more high than the implant high. This observation could justify a decrease in bone highness from the first measurement (3 months after surgery) to the second measurement (51 months after surgery) observed in the study of Bassi et al.19, considering a decrease in 1.57 mm the patients treated with graftless maxillary sinus lift.
However, Nkenke and Stelzle25 presented a systematic review where they observed that the clinical evidence neither refutes nor promotes the use of autogenous grafts in sinus floor elevations, indicating that the recovery time of the graft may not be entirely related to the material used for bone grafting. Of the conclusions obtained from different biomaterials used in bone reconstruction, it has been observed that there is a triad of elements that coexist in the grafted site: newly formed bone, remnants of grafted material and fibrous connective tissue, which may be greater or smaller depending on the type of material and type of study26. In the same vein, Rickert et al.7 performed a systematic review, comparing autogenous bone and autogenous bone associated with growth factors or bone substitutes, but reported no significant differences in the various materials that were analyzed.
Meloni et al.27 examined the conventional technique of maxillary sinus lift using inorganic bovine bone alone or inorganic bovine bone mixed with autogenous bone in equal proportions and found no differences in periimplant bone formation at the time of insertion or after 6 and 12 months of follow-up. For their part, Garlini et al.28 conducted a study with x-ray analysis after 11 years of implant installation in maxillary sinuses elevated with alloplastic bone, considering a preoperative alveolar height of approximately 5 mm; the 47 implants had a 96% success rate. It is interesting to note that 5-mm remnants of bone height enable primary implant stability and with it the joint technique of implant installation and maxillary sinus lift.
Although autogenous bone has traits that are difficult to obtain with biomaterials, biomaterial has had interesting effects on the receptor bed. Chaves et al.29 reported that the use of Bio-Oss allows greater induction of the formation of osteocalcin, receptor activator of nuclear factor κB ligand (RANKL) and osteoprotegerin. Nevertheless, the vehicle used to place the biomaterial in the cavity generated in the maxillary sinus is also important; Stiller et al.30 presented a comparative analysis between β-tricalcium phosphate in granules or in paste. The granules were shown to be more efficient than the paste.
The conclusions drawn by the current literature indicate that implant installation times are not necessarily related to the material used in the bone reconstruction, or to the exclusive use of autogenous bone or to the combination of autogenous bone with biomaterials or growth factors. Therefore, other variables that also interact must exist to achieve the success that supports the lateral window maxillary sinus lift.
The influence of the biomaterial in maxillary sinus reconstruction and the carrier are components of the equation and others variables are involved. The periosteum, the quality and amount of surrounding bone tissue, the sinus membrane and the presence and type of dental implants have a role in the formula where the weight of each variable has not been established.
Lundgren et al.12 described spontaneous intrasinus bone formation from the removal of a cyst, whereas Jung et al.31 reported on the spontaneous intrasinus bone formation following the extraction of a tooth included in the maxillary sinus. These clinical findings indicate new directions in intrasinus bone regeneration, suggesting that the maintenance of the clot could lead to bone formation at this anatomical site.
Responses to this situation may concentrate on the sinus membrane. Srouji et al.32 performed a study where sinus membrane samples were obtained from 5 patients; cell cultivation was carried out by obtaining alkaline phosphatase expression. Application of the appropriate vehicle revealed a clear sequence of bone formation induction. Rong et al.33 defined 3 groups: a sinus floor lift using the conventional technique, the installation of an upper metallic mesh to isolate the sinus membrane, and a lower metallic mesh that divided the bone tissue of the inferior and lateral area. These fillings were done with Bio-Oss with evaluations 1 and 3 months later. Comparisons with the control group indicated that the group with upper blocking exhibited high inferior bone formation and low superior bone formation, whereas the lower blocking group demonstrated minimal inferior bone formation and low superior bone formation. Based upon these results, the role of the sinus membrane and the type and quality of peripheral bone appear to be relevant variables in this reconstruction formula.
The role of the walls of the adjacent bone in the intrasinus cavity has been poorly analyzed in previous studies; when the residual alveolar bone for implant installation is at least 4 to 5 mm wide and there are adjacent teeth, there must be well-defined superior and inferior cortical and cancellous bone, which permits adequate blood flow in the area. Thor et al.14 installed immediate implants and performed graftless maxillary sinus lift in areas with these characteristics, which could make this cavity-type defect behave similarly to a three-wall defect34. Such bone regeneration conditions were also assessed by Rubio and Mombrú35, who demonstrated that in wide cystectomy areas with cavities up to 2 cm in diameter, there was spontaneous regeneration in 88% of patients after at 6 months of follow-up without the installation of bone grafts; the bone quality and its irrigation capacity did allow for bone progression and regeneration.
In light of evidence suggesting the importance of the membrane and the surrounding bone, Moon et al.11 showed the efficiency of the maxillary sinus lift with implant installation and the simultaneous use of peripheral blood as intrasinus filling, and Thor et al.14 had already demonstrated the efficiency of the same technique keeping the blood in the maxillary sinus without bone filling. The biological foundation for this clinical condition may be supported by the results of Xu et al.36, who indicated the blood clot was the center of formation and that can be not stable in the initial phase.
Based upon the premise of intrasinus augmentation with blood content alone, de Oliveira et al.37 conducted a study of maxillae with total edentulism and partial edentulism and reported complications due to the poor bone formation observed in the maxillary sinuses that underwent surgical procedures. They also reported causes for failure, which included the size of the elevated maxillary sinus, poor bone quality and the absence of a dental implant placed during the same surgery.
The size of the sinus cavity is likely also important. De Moraes et al.4 established the need for cavity reconstruction of up to 2 cm3 in cases of highly pneumatized maxillary sinuses and determined that large sinus cavities are considered critical defects38; as a result, the blood clot is incapable of contributing to bone regeneration, but the implant installation during the same surgery could stabilize the system, ensuring that the size of the defect is smaller and that the stabilized clot contributes to bone tissue formation.
An extensive volume of the maxillary sinus (intra-sinus cavity) show high cortical bone (less vascularization) than cancellous bone in the buccal side; the periosteum and cancellous bone that remain in edentulous maxillary sinuses contain a smaller number of osteoprogenitor cells39 and thus allow fewer options for new bone formation.
The anatomical context of the maxillary sinus is relevant because it influences the sinus membrane, bone quality, bone quantity and the presence or absence of adjacent teeth. The equation to establish intrasinus bone formation is not yet clear, so any analyses of intrasinus bone regeneration with different techniques and materials must be made with caution, as the order of relevance of the factors involved has yet to be ascertained.
The technique for graftless sinus lift use a lateral window approach with osteotomy and displacement of the sinus membrane; the bone wall is removed and ultrasonic systems can help in the osteotomy. Later, the perforation is made, and the implant is installed. Since the membrane may collapse on the implant, some authors recommend suturing the membrane to techthe top of the lateral window, although the importance of this step has not been determined40.
The use of immediate implant in graftless maxillary sinus lift has important foundations. Initially, implant installation requires a minimum bone height to ensure primary stability of the implant41, which guarantees the viability of the treatment and the option of integrating the device. When there is a minimum bone height of 3 mm, there is also clearly enough cancellous bone remaining to guarantee minimum blood supply levels. Thor et al.14 reported that immediate installation would also take advantage of the benefits of the surface treatment of the implant that could heighten thrombogenic potential together with greater stimulus for the proliferation of osteoblasts and greater expression of platelet-derived growth factor (PDGF) that increases mineralization.
However, the implant installation process causes surgical trauma in any bone surgery, and this increases the option of tissue regeneration42. Additionally, the implant would serve to support the sinus membrane that has been lifted by the implant. Haas et al.4344 conducted an interesting investigation that evaluated the visual behavior of implants installed in sinuses without filling and with autogenous, heterogeneous and homogeneous filling. Total membrane collapse onto the implant was observed in the sites without filling, whereas no such collapse was noted when the autogenous graft had been placed at an almost apical level of the implant and the other biomaterials were 2 to 4 mm over the apical limit of the implant. Membrane collapse in the graftless sites could also be related to the size of the implant installed in the elevated sinuses; in terms of new bone formed in the four groups, the greatest level was observed in the sites with the autogenous bone graft, followed by the implant installed in graftless sites, as the latter exceeded more than 10% of the bone formation compared to sites grafted with biomaterial, demonstrating that maintenance with a blood clot alone would aid in the formation of more bone tissue than the use of some intrasinus fillings. There were no significant differences in the mechanical load measurements.
The clinical results observed when the implant was immediately installed during the graftless maxillary sinus lift have been promising. Chen et al.15 described 47 cases that underwent surgery with 75 implants installed and were followed-up after 24 months; 74 were completed successfully. Cricchio et al.45 treated 84 patients with 239 implants; 236 of these were successful according to evaluations that took place at 12 to 72 months postoperatively. Bassi et al.19 treated 20 patients with 25 implants installed during a follow-up period that lasted from 3 to 51 months and 24 implants were successful. These conditions show the viability of the graftless implant installation. Cara-Fuentes et al.46 conducted a comparative study on groups with elevation with or without graft that found no short-term differences between the two groups.
The application of growth factors in the implantation technique without filling has also been analyzed in animal and human models. Jeong et al.47 used a canine model for implant installation with a maxillary sinus lift filled with platelet-rich fibrin (PRF); they concluded that the histological results would be variable and therefore of low consistency and low predictability. These conclusions, which are somewhat unclear to many clinicians, have been consistent with the findings of studies by Mooren et al.48, who compared filling with Bio-Oss and Bio-Oss with PRF in critical defects and concluded there were no differences between the two techniques.
Choukroun et al.49 showed results that were obtained from the PRF applied to the maxillary sinus lifts either with or without the use of an allograft, concluding that PRF use could reduce the recovery time of the maxillary sinus to 4 months to leave it ready for implant installation; nevertheless, in this study there was no control group with the exclusive application of PRF or the exclusive application of an allograft evaluated during the same 4 months, there being only a group with an allograft analyzed at 8 months that presented similar bone conditions. Grageda et al.50 conducted a study on sheep using a maxillary sinus lift with an allograft in one sinus and an allograft with platelet-rich plasma (PRP) in the other. They performed comparative histological studies at 3 and 6 months and confirmed there were no differences between the groups in terms of newly formed bone and the percentage of bone present in the two sinuses. Thus, their conclusion was that there was no correlation between the use of PRP and new formation of intrasinus bone.
These results regarding PRF applied to a maxillary sinus are likely related to the fact that the osteoblast capacity of the PRF has not yet been verified. Baslarli et al.51 installed PRF in sites of extracted third molars and compared these sites to sites without bone filling (divided mouth model); on nuclear medicine analysis, the lack of difference in bone metabolism between the two sites was confirmed. Kumar et al.52 carried out a similar investigation and concluded there were no differences in the bone formation, but improvements in the periodontal insertion of the second molar in cases of PRF use had been made. Although the present study does not attempt to analyze the status of PRF or other derivatives, it was important to do some observations related to the graftless technique.
In light of the clinical conditions described in prior reviews, case series and clinical trials in the past 10 years, there may be variables in sinus reconstruction that have not been correctly assessed. Gurtner et al.53 indicated that essential elements for bone regeneration include stem cells, anchoring elements and growth factors; the presence of a blood clot in the sinus cavity combined with dental implants may satisfy these requirements.
Physiological mechanisms of intrasinus bone regeneration have not confirmed the value of each variable in the equation used for bone reconstruction. Local anatomical factors and those of the implanted device along with those related to the surgery itself all contribute to the success of maxillary sinus lift surgery, which makes the graftless technique possible in certain cases. Based on these analyses, the role of the filling material in maxillary sinus lift is not clear.
References
1. Tatum H Jr. Maxillary and sinus implant reconstructions. Dent Clin North Am. 1986; 30:207–229. PMID: 3516738.
2. Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980; 38:613–616. PMID: 6993637.
3. Mendoza G, Morales P, Reyes F, Navarro P, Garay I, Olate S. The alveolar bone high in posterior area of maxilla and the relation with tooth loss. Int J Morphol. 2013; 31:822–825.
4. De Moraes PH, Costa VOC, Olate S, Caria PHF, Barbosa JRA. Morphometric study of maxillary sinus by computed tomography. Assessment of sinus floor bone reconstruction. Int J Morphol. 2012; 30:592–598.
5. Rodríguez-Chessa JG, Olate S, Netto HD, Shibli J, de Moraes M, Mazzonetto R. Treatment of atrophic maxilla with zygomatic implants in 29 consecutives patients. Int J Clin Exp Med. 2014; 7:426–430. PMID: 24600500.
6. Cidade CP, Olate S, Pozzer L, Pimentel MJ, Nóbilo M, Albergaria-Barbosa JR. Stress analysis in maxillary all-on-four model. Int J Odontostomat. 2015; 9:205–211.

7. Rickert D, Slater JJ, Meijer HJ, Vissink A, Raghoebar GM. Maxillary sinus lift with solely autogenous bone compared to a combination of autogenous bone and growth factors or (solely) bone substitutes. A systematic review. Int J Oral Maxillofac Surg. 2012; 41:160–167. PMID: 22099314.

8. Chiapasco M, Zaniboni M, Rimondini L. Dental implants placed in grafted maxillary sinuses: a retrospective analysis of clinical outcome according to the initial clinical situation and a proposal of defect classification. Clin Oral Implants Res. 2008; 19:416–428. PMID: 18266875.

9. Olate S, Pozzer L, Luna AHB, Mazonetto R, de Moraes M, Barbosa JRA. Estudio retrospectivo de 91 cirugías de elevación de seno maxilar para rehabilitación sobre implantes. Int J Odontostomat. 2012; 6:81–88.

10. Lundgren S, Cricchio G, Palma VC, Salata LA, Sennerby L. Sinus membrane elevation and simultaneous insertion of dental implants: a new surgical technique in maxillary sinus floor augmentation. Periodontol 2000. 2008; 47:193–205. PMID: 18412582.

11. Moon JW, Sohn DS, Heo JU, Shin HI, Jung JK. New bone formation in the maxillary sinus using peripheral venous blood alone. J Oral Maxillofac Surg. 2011; 69:2357–2367. PMID: 21719179.

12. Lundgren S, Andersson S, Gualini F, Sennerby L. Bone reformation with sinus membrane elevation: a new surgical technique for maxillary sinus floor augmentation. Clin Implant Dent Relat Res. 2004; 6:165–173. PMID: 15726851.

13. Hatano N, Sennerby L, Lundgren S. Maxillary sinus augmentation using sinus membrane elevation and peripheral venous blood for implant-supported rehabilitation of the atrophic posterior maxilla: case series. Clin Implant Dent Relat Res. 2007; 9:150–155. PMID: 17716259.

14. Thor A, Sennerby L, Hirsch JM, Rasmusson L. Bone formation at the maxillary sinus floor following simultaneous elevation of the mucosal lining and implant installation without graft material: an evaluation of 20 patients treated with 44 Astra Tech implants. J Oral Maxillofac Surg. 2007; 65(7 Suppl 1):64–72. PMID: 17586351.

15. Chen TW, Chang HS, Leung KW, Lai YL, Kao SY. Implant placement immediately after the lateral approach of the trap door window procedure to create a maxillary sinus lift without bone grafting: a 2-year retrospective evaluation of 47 implants in 33 patients. J Oral Maxillofac Surg. 2007; 65:2324–2328. PMID: 17954333.

16. Lin IC, Gonzalez AM, Chang HJ, Kao SY, Chen TW. A 5-year follow-up of 80 implants in 44 patients placed immediately after the lateral trap-door window procedure to accomplish maxillary sinus elevation without bone grafting. Int J Oral Maxillofac Implants. 2011; 26:1079–1086. PMID: 22010092.
17. Balleri P, Veltri M, Nuti N, Ferrari M. Implant placement in combination with sinus membrane elevation without biomaterials: a 1-year study on 15 patients. Clin Implant Dent Relat Res. 2012; 14:682–689. PMID: 21176096.

18. Chipaila N, Marini R, Sfasciotti GL, Cielo A, Bonanome L, Monaco A. Graftless sinus augmentation technique with contextual placement of implants: a case report. J Med Case Rep. 2014; 8:437. PMID: 25515949.

19. Bassi AP, Pioto R, Faverani LP, Canestraro D, Fontão FG. Maxillary sinus lift without grafting, and simultaneous implant placement: a prospective clinical study with a 51-month follow-up. Int J Oral Maxillofac Surg. 2015; 44:902–907. PMID: 25896082.

20. Stern A, Green J. Sinus lift procedures: an overview of current techniques. Dent Clin North Am. 2012; 56:219–233. PMID: 22117952.

21. Garbacea A, Lozada JL, Church CA, Al-Ardah AJ, Seiberling KA, Naylor WP, et al. The incidence of maxillary sinus membrane perforation during endoscopically assessed crestal sinus floor elevation: a pilot study. J Oral Implantol. 2012; 38:345–359. PMID: 22913307.

22. Raja SV. Management of the posterior maxilla with sinus lift: review of techniques. J Oral Maxillofac Surg. 2009; 67:1730–1734. PMID: 19615589.

23. Arasawa M, Oda Y, Kobayashi T, Uoshima K, Nishiyama H, Hoshina H, et al. Evaluation of bone volume changes after sinus floor augmentation with autogenous bone grafts. Int J Oral Maxillofac Surg. 2012; 41:853–857. PMID: 22551647.

24. Thomas MV, Puleo DA. Infection, inflammation, and bone regeneration: a paradoxical relationship. J Dent Res. 2011; 90:1052–1061. PMID: 21248364.

25. Nkenke E, Stelzle F. Clinical outcomes of sinus floor augmentation for implant placement using autogenous bone or bone substitutes: a systematic review. Clin Oral Implants Res. 2009; 20(Suppl 4):124–133. PMID: 19663959.

26. Proussaefs P, Lozada J. Use of titanium mesh for staged localized alveolar ridge augmentation: clinical and histologic-histomorphometric evaluation. J Oral Implantol. 2006; 32:237–247. PMID: 17069168.

27. Meloni SM, Jovanovic SA, Lolli FM, Cassisa C, De Riu G, Pisano M, et al. Grafting after sinus lift with anorganic bovine bone alone compared with 50:50 anorganic bovine bone and autologous bone: results of a pilot randomised trial at one year. Br J Oral Maxillofac Surg. 2015; 53:436–441. PMID: 25796408.

28. Garlini G, Redemagni M, Donini M, Maiorana C. Maxillary sinus elevation with an alloplastic material and implants: 11 years of clinical and radiologic follow-up. J Oral Maxillofac Surg. 2010; 68:1152–1157. PMID: 20156662.

29. Chaves MD, de Souza Nunes LS, de Oliveira RV, Holgado LA, Filho HN, Matsumoto MA, et al. Bovine hydroxyapatite (Bio-Oss(®)) induces osteocalcin, RANK-L and osteoprotegerin expression in sinus lift of rabbits. J Craniomaxillofac Surg. 2012; 40:e315–e320. PMID: 22513050.

30. Stiller M, Kluk E, Bohner M, Lopez-Heredia MA, Müller-Mai C, Knabe C. Performance of β-tricalcium phosphate granules and putty, bone grafting materials after bilateral sinus floor augmentation in humans. Biomaterials. 2014; 35:3154–3163. PMID: 24439419.

31. Jung YS, Chung SW, Nam W, Cho IH, Cha IH, Park HS. Spontaneous bone formation on the maxillary sinus floor in association with an extraction socket. Int J Oral Maxillofac Surg. 2007; 36:656–657. PMID: 17367999.

32. Srouji S, Ben-David D, Lotan R, Riminucci M, Livne E, Bianco P. The innate osteogenic potential of the maxillary sinus (Schneiderian) membrane: an ectopic tissue transplant model simulating sinus lifting. Int J Oral Maxillofac Surg. 2010; 39:793–801. PMID: 20417057.

33. Rong Q, Li X, Chen SL, Zhu SX, Huang DY. Effect of the Schneiderian membrane on the formation of bone after lifting the floor of the maxillary sinus: an experimental study in dogs. Br J Oral Maxillofac Surg. 2015; 53:607–612. PMID: 26025764.

34. Choi JY, Jung UW, Lee IS, Kim CS, Lee YK, Choi SH. Resolution of surgically created three-wall intrabony defects in implants using three different biomaterials: an in vivo study. Clin Oral Implants Res. 2011; 22:343–348. PMID: 20831755.

35. Rubio ED, Mombrú CM. Spontaneous bone healing after cysts enucleation without bone grafting materials: a randomized clinical study. Craniomaxillofac Trauma Reconstr. 2015; 8:14–22. PMID: 25709749.

36. Xu H, Shimizu Y, Ooya K. Histomorphometric study of the stability of newly formed bone after elevation of the floor of the maxillary sinus. Br J Oral Maxillofac Surg. 2005; 43:493–499. PMID: 15908076.

37. de Oliveira GR, Olate S, Cavalieri-Pereira L, Pozzer L, Asprino L, de Moraes M, et al. Maxillary sinus floor augmentation using blood without graft material. Preliminary results in 10 patients. J Oral Maxillofac Surg. 2013; 71:1670–1675. PMID: 23891012.

38. Callan DP, Rohrer MD. Use of bovine-derived hydroxyapatite in the treatment of edentulous ridge defects: a human clinical and histologic case report. J Periodontol. 1993; 64:575–582. PMID: 8393110.

39. Bruder SP, Fink DJ, Caplan AI. Mesenchymal stem cells in bone development, bone repair, and skeletal regeneration therapy. J Cell Biochem. 1994; 56:283–294. PMID: 7876320.
40. Riben C, Thor A. The maxillary sinus membrane elevation procedure: augmentation of bone around dental implants without grafts--a review of a surgical technique. Int J Dent. 2012; 2012:DOI: 10.1155/2012/105483.

41. Esposito M, Grusovin MG, Rees J, Karasoulos D, Felice P, Alissa R, et al. Effectiveness of sinus lift procedures for dental implant rehabilitation: a Cochrane systematic review. Eur J Oral Implantol. 2010; 3:7–26. PMID: 20467595.
42. Dimitriou R, Jones E, McGonagle D, Giannoudis PV. Bone regeneration: current concepts and future directions. BMC Med. 2011; 9:66. PMID: 21627784.

43. Haas R, Haidvogl D, Donath K, Watzek G. Freeze-dried homogeneous and heterogeneous bone for sinus augmentation in sheep. Part I: histological findings. Clin Oral Implants Res. 2002; 13:396–404. PMID: 12175377.
44. Haas R, Haidvogl D, Dörtbudak O, Mailath G. Freeze-dried bone for maxillary sinus augmentation in sheep. Part II: biomechanical findings. Clin Oral Implants Res. 2002; 13:581–586. PMID: 12519331.
45. Cricchio G, Sennerby L, Lundgren S. Sinus bone formation and implant survival after sinus membrane elevation and implant placement: a 1- to 6-year follow-up study. Clin Oral Implants Res. 2011; 22:1200–1212. PMID: 21906186.

46. Cara-Fuentes M, Machuca-Ariza J, Ruiz-Martos A, Ramos-Robles MC, Martínez-Lara I. Long-term outcome of dental implants after maxillary augmentation with and without bone grafting. Med Oral Patol Oral Cir Bucal. 2016; 21:e229–e235. PMID: 26827071.

47. Jeong SM, Lee CU, Son JS, Oh JH, Fang Y, Choi BH. Simultaneous sinus lift and implantation using platelet-rich fibrin as sole grafting material. J Craniomaxillofac Surg. 2014; 42:990–994. PMID: 24503388.
48. Mooren RE, Dankers AC, Merkx MA, Bronkhorst EM, Jansen JA, Stoelinga PJ. The effect of platelet-rich plasma on early and late bone healing using a mixture of particulate autogenous cancellous bone and Bio-Oss: an experimental study in goats. Int J Oral Maxillofac Surg. 2010; 39:371–378. PMID: 20129756.

49. Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part V: histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:299–303. PMID: 16504861.

50. Grageda E, Lozada JL, Boyne PJ, Caplanis N, McMillan PJ. Bone formation in the maxillary sinus by using platelet-rich plasma: an experimental study in sheep. J Oral Implantol. 2005; 31:2–17. PMID: 15751383.

51. Baslarli O, Tumer C, Ugur O, Vatankulu B. Evaluation of osteoblastic activity in extraction sockets treated with platelet-rich fibrin. Med Oral Patol Oral Cir Bucal. 2015; 20:e111–e116. PMID: 25475771.

52. Kumar N, Prasad K, Ramanujam L, K R, Dexith J, Chauhan A. Evaluation of treatment outcome after impacted mandibular third molar surgery with the use of autologous platelet-rich fibrin: a randomized controlled clinical study. J Oral Maxillofac Surg. 2015; 73:1042–1049. PMID: 25659357.

53. Gurtner GC, Callaghan MJ, Longaker MT. Progress and potential for regenerative medicine. Annu Rev Med. 2007; 58:299–312. PMID: 17076602.

Table 1
Description of the studies included in this analysis of the graftless maxillary sinus lift procedure
| Reference | No. of implants | Follow-up (mo) | Successful implants | Lost implants |
|---|---|---|---|---|
| Lundgren et al.12 (2004) | 19 | 18 | 19 | 0 |
| Hatano et al.13 (2007) | 14 | 12-24 | 13 | 1 |
| Thor et al.14 (2007) | 44 | 48 | 43 | 1 |
| Chen et al.15 (2007) | 75 | 24 | 75 | 0 |
| Moon et al.11 (2011) | 31 | 25 | 29 | 2 |
| Cricchio et al.45 (2011) | 239 | 12-72 | 236 | 3 |
| Lin et al.16 (2011) | 80 | 60 | 80 | 0 |
| Balleri et al.17 (2012) | 28 | 12 | 28 | 0 |
| Chipaila et al.18 (2014) | 2 | 6 | 2 | 0 |
| Bassi et al.19 (2015) | 25 | 3 and 51 | 24 | 1 (preload) |




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download