1. Elevator positioning
An elevator should be positioned such that the ventral surface of the tip contacts a hard point(s) on the tooth particle being extracted, while the dorsal surface of the elevator working end contacts a hard intra-oral point(s), such that if a force of a specific magnitude and direction is applied to the tooth particle at the ventral contact point of the elevator tip, the tooth particle will move progressively, but the force will not be enough to damage the ventral or dorsal contact point(s), which would cause loss of leverage at that elevator position. A useful dental elevator position is often described
278 as a “purchase point,” although this term is imprecise because a dental elevator tip must simultaneously contact at least two points, a dorsal and a ventral point, for the elevator to leverage a tooth particle. Alternatively, elevator positioning can be described as a combination of luxation parameters: the dorsal and ventral elevator tip contact points and the magnitude and direction of the tip force
9. Sectioning teeth or removing bone are claimed to “create a purchase point” for the elevator tip
23, but more precisely sectioning or removing bone increases the options for positioning an elevator tip, such that different combinations of hard dorsal and ventral tip contact points become available for luxation.
If the tip contact points are structurally weak and can be damaged by a large force, or if a neighboring tooth must be used as a dorsal tip contact point, only a small force should be applied to the elevator tip contact surfaces that are available for luxating. This non-ideal leverage may result in only a microscopic progressive movement of the tooth particle, which may only be detected with microscopes
9. However, this microscopic movement can lead to macroscopic movement of the tooth particle or permit microscopically deeper penetration of the elevator tip between the tooth particle and the alveolar bone, which can open access to other elevator tip contact points and could cause additional microscopic progressive tooth particle movements.
Luxating while using a neighboring healthy tooth as a dorsal elevator tip contact area is generally discouraged
123. The clinician should try different elevator tip positions and angles to minimize movement of neighboring teeth. A 330 bur can be used to remove the inter-proximal contacts on the tooth particle to be extracted, which increases the degrees of freedom of movement of the tooth particle, since the inter-proximal surfaces of neighboring teeth will not restrict tooth particle movement. This often helps when extracting primary teeth or healthy premolars that are extracted for orthodontic purposes.
2. Basic elevator force applications
One basic luxation motion results from placing a straight elevator tip around the superior perimeter of a tooth particle
3, such that the ventral surface contacts a maximum number of points on the tooth particle perimeter, and the elevator tip dorsal surface contacts various points on the alveolar bone or, less ideally, the neighboring tooth; the straight elevator axis is approximately coincident to or off-angle with the tooth long axis.(
Fig. 1) The dentist then oscillates the elevator tip with a short-amplitude, clockwise-to-counter-clockwise motion while pushing the elevator apically in order to sever the periodontal ligament apically along the tooth root, which allows further apical advancement of the elevator tip to increase elevator leverage. The straight elevator handle can also be moved apically, such that the elevator tip imparts a superiorly directed lifting force to the tooth particle. Each elevator tip contact point along the superior perimeter of the tooth particle applies a lever point force with a vector approximately perpendicular to the tooth long axis. The clockwise/counter-clockwise oscillating motion of the straight elevator tip results in multiple such pinpoint lever motions per unit time, rotating the tooth particle within the socket on the tooth long axis.
 | Fig. 1A straight elevator is used to luxate a carious root tip, with the elevator tip positioned at the root tip superior perimeter.
|
Another basic luxation motion is to impart a radial force to a tooth particle to move the tooth particle parallel to the curvature of the socket in which the particle root is embedded or parallel to an imaginary curved path of least resistance. A Cryer elevator
3 has a thick, curved, triangular working end with a pointy tip that can impart strong rotational forces to a tooth particle, where essentially only one point on the ventral surface of the tip contacts the tooth particle, and the applied force only moves along one rotational vector axis for each luxation movement. Frictional force, or a luxation force with a force vector perpendicular to the tooth surface, holds the tip in contact with the tooth particle.
Since the Cryer elevator generally only contacts a tooth at a single point, it is not capable of the basic oscillating motion described previously, since this oscillating motion requires multiple points of contact along the tooth particle perimeter. Instead, the Cryer elevator is used where the tip can contact a relatively wide, exposed area on the tooth
3 and from where a practically useful rotational force can be generated. A Cryer elevator tip is often placed several millimeters inside a socket such that the ventral tip point contacts the tooth, and the dorsal tip contact point(s) pushes against the alveolar wall, socket septum bone, tooth root of the tooth being extracted or, less ideally, the neighboring tooth.(
Fig. 2) The wide distal end of the Cryer elevator increases the probability of the dorsal tip surface contacting hard points for leverage, while the short, triangular tip facilitates penetration into the socket.
 | Fig. 2A model shows a Cryer elevator placed inside a socket such that the dorsal aspect of the tip contacts the neighboring tooth or socket wall, and the tip contacts an exposed flat surface on the tooth.
|
Cryer elevators can luxate a mandibular molar distal root after the coronal aspect of septum bone is removed in order to expose the mesial surface of the distal root. The Cryer elevator tip is placed on the exposed mesial root surface to luxate the root along a distal-radial path of least resistance
37.
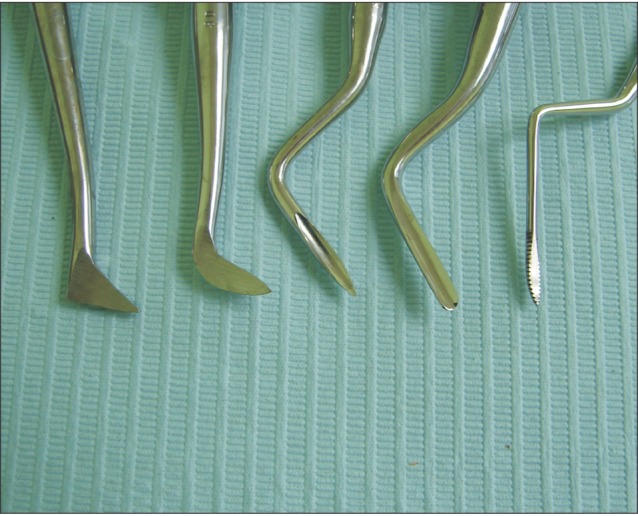
Generally, elevator instruments with a 45° to 90° bend of the working end function like Cryer elevators, since the bend prevents the ability to rotate the handle to create an oscillating luxation tip movement.(
Fig. 3) A root tip pick with a long, thin handle and a curved working end with a pointy or curved tip also essentially operates via a single ventral tip surface contact point that applies a rotational force vector to the tooth particle. A conventional triangle-shaped Cryer elevator might be less useful for extracting tiny root tips compared to a root tip pick since the short working end of the Cryer elevator prevents deep penetration into a socket to remove a root tip, and the Cryer tip is too thick to fit between the root tip and the alveolar bone.
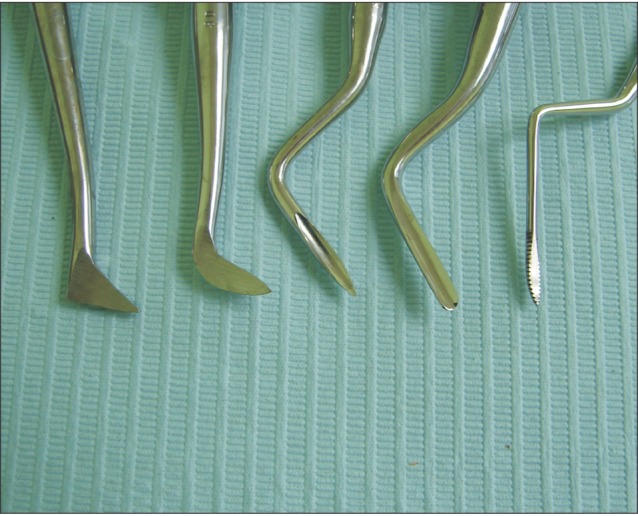 | Fig. 3A conventional Cryer elevator (left) displayed with other pointy-tipped elevators, some with 45° to 90° bends of the working end, that essentially apply Cryer elevator functionality.
|
A straight elevator can also impart a radially directed force to a tooth particle that, like the force imparted by the Cryer elevator, moves the tooth along a rotational path of least resistance. Here, the dentist places the straight elevator into the inter-proximal aspect of the tooth to be luxated, with the elevator shaft positioned approximately perpendicular
3 to the tooth long axis, with the ventral surface of the working end of the elevator facing the interproximal surface of the tooth to be luxated, and rotates the elevator.(
Fig. 4) The straight elevator contacts multiple ventral contact points, compared to the single ventral contact point of the Cryer elevator. Depending on the direction of rotation, either the apical long edge of the working end or the superior long edge will contact the tooth particle. If the apical edge is exerting force on the tooth being extracted, the dorsal tip surface can impart an apical force vector to the neighboring tooth
3. If the superior edge is exerting force on the tooth being extracted, the dorsal tip surface can impart a superior force vector to the neighboring tooth. The elevator angle can be changed to impart a buccal vector component to the force, potentially rotating the tooth out from a buccal path of least resistance. The dentist can supplement this radial motion with an apically-directed, oscillating elevator tip movement.
 | Fig. 4A straight elevator luxates a maxillary third molar with a rotational force, with the elevator shaft positioned approximately perpendicular to the tooth long axis.
|
Another basic luxation motion is to insert the elevator tip into the socket, turn the elevator handle in an oscillating clockwise-counter-clockwise motion, and use the longitudinal edge of the elevator working end to apply a rotational force to the tooth particle in order to rotate the tooth particle on the long axis, and push the tooth particle away from the socket wall.(
Fig. 5) Microscopes and co-axial illumination facilitate observation inside the socket to determine if this luxation is progressive.
 | Fig. 5A straight elevator, placed inside a socket, luxates a root tip using the longitudinal edge of the working end of the elevator after removing bone mesial to the root tip to create space for luxation.
|
Another basic elevator motion occurs when an elevator tip dorsal contact point cannot be identified due to difficult access to the tooth particle. In this case, non-leveraged manual force is used to push the elevator tip ventral surface into a tooth particle to impart a force vector that is essentially perpendicular to the tooth particle long axis. This motion might not provide as much force as a leveraged force, but can be effective if minimal force is needed to remove the tooth particle, or if the translational movement peels the tooth particle from the alveolar bone such that a more effective elevator instrument can be placed between the tooth particle and the alveolar bone. Sometimes, the tooth particle can be drilled with a surgical bur to shift the particle, and then the bur is used to apply a force perpendicular to the tooth particle long axis.
3. Elevator working end
Different shapes, widths, and curvatures of elevator working ends influence which points of contact are made with both the ventral and dorsal elevator tip surfaces and affect elevator functionality.(
Fig. 6) If the elevator tip center is too protrusive, when the tip center is placed between the tooth and the alveolar bone, the tip points that are lateral to the tip center can be positioned superior to, and not in contact with, the tooth particle perimeter. In addition, a small elevator tip can be so small in diameter that few tip points lateral to the tip center can contact the tooth particle. Consequently, clockwise-counter-clockwise oscillating movements of the tip will be minimally effective, since the elevator tip center point imparts minimal rotational force vectors to the tooth particle.
 | Fig. 6Examples of straight elevator tip shapes (left to right): a flat tip without longitudinal side curvature, a tip with slightly too much curvature per unit length, a tip whose center protrudes compared to points lateral to the center, a large elevator with less curvature per unit of tip length and where the tip center is minimally protrusive, and a small elevator with a dorsal curvature of the entire working end.
|
The elevator tip curvature determines how similar is the tip shape to the curvature of the tooth particle superior perimeter and affects the number of contact points between the elevator tip ventral surface and the tooth particle superior perimeter. A precise fit of the tip curvature with the tooth particle perimeter curvature ensures that the lateral points of the tip impart torquing forces to the tooth during oscillation movements. If there is too much tip curvature, the elevator tip curvature will be smaller than the curvature of the tooth particle superior perimeter, resulting in the superior surface of the tooth particle blocking the tip from fitting between the alveolar bone and the tooth particle perimeter. If there is no tip curvature, it is possible that only the center of the elevator tip ventral surface will contact the tooth particle, resulting in minimally useful oscillating movements.(
Fig. 6)
A posterior curve of the entire working end of the elevator can improve elevator tip access to tooth particles located on socket walls or to the mesial surface of a mandibular molar root. A thinner, sharper elevator tip facilitates apical penetration into the periodontal ligament around the tooth particle superior perimeter, although if the tip is too thin, it can eventually chip. If the tip is too thick, it might not penetrate the thin space between the tooth particle and the alveolar bone, or it might not penetrate between teeth embrasure spaces. The elevator tip curvature can extend 5 to 10 mm longitudinally up the elevator working end, which allows the lateral curved sides of the working end to contact a tooth particle for luxation.(
Fig. 6)
4. Small and large straight elevators
An elevator edge may only be able to penetrate a fraction of a millimeter between strong alveolar bone and a tooth particle. Consequently, each elevator contact point provides minimal leverage due to the longer distance to the tooth apex, which results in a longer, less effective lever arm. Therefore, a large number of contact points is needed to provide sufficient total force and leverage to luxate the tooth particle. Here, a large straight elevator with a large number of contact points along the tooth particle perimeter might be more effective for luxating the tooth particle compared to a small straight elevator. However, any size straight elevator tip can progressively luxate a tooth particle if the tip contacts multiple points on a significant fraction of the tooth particle perimeter.
Compared to a small elevator, a large elevator can accommodate a larger number of elevator tip surface contact points along tooth particle perimeters. Consequently, the total force the dentist puts on the elevator is divided among many contact points, resulting in less force per contact point. Less force per contact point reduces the risk that the force per contact point will be large enough to damage either the intra-oral surfaces contacted by the elevator tip dorsal surfaces or the tooth surfaces contacted by the elevator tip ventral surfaces, which would result in loss of elevator leverage. If the same force is applied on a small elevator that has fewer tip contact points, the higher force per contact point can result in the small elevator tip fracturing the tooth particle, compressing or damaging the dorsal contact point, or increasing the distance between the alveolar bone and the tooth particle, resulting in loss of leverage. Putting a smaller force on the small elevator reduces the force per contact point, but the total force on the small elevator might not be sufficient to progressively luxate the tooth particle.
A small straight elevator can be placed into an inter-proximal embrasure space to luxate a tooth particle while applying minimal force on the neighboring tooth not planned for extraction. After the small elevator has luxated the tooth particle and widened the space between the tooth particle and the alveolar bone, the large elevator can be used to further luxate the tooth particle. If a tooth root is tightly bound to the alveolar bone, a dentist can sometimes use an explorer tip to create an initial apical penetration between the tooth particle and the alveolar bone, use a small elevator to expand this initial access, and then use a large straight elevator for luxation.
5. Sectioning and bone removal
Tooth particle luxation might require slots to be created between teeth roots or within a single root in order to provide elevator tip insertion points and to allow access to combinations of elevator tip ventral and dorsal contact points
78. Creating a slot permits more apical penetration of a luxation instrument into the socket, such that the luxation instrument contacts the tooth closer to the root apex, which increases the leverage forces on the root compared to a more coronal elevator contact point. A surgical bur should be thin in cross section in order to facilitate creation of a thin slot that will snugly fit an elevator tip and have multiple ventral and dorsal tip contact points for leverage. Teeth that are embedded in strong alveolar bone, where an elevator tip cannot penetrate between the tooth and the alveolar bone, might require sectioning from the earliest stage of the extraction procedure due to lack of elevator tip insertion points. Sectioning can sometimes begin by cutting off the crown at the gingiva, if the tooth crown obstructs visibility of and access to roots and furcations. Ideally, the supra-gingival tooth structure will remain for grasping if forceps are needed to complete the extraction.
With clinical experience, a dentist may develop an intuition for determining which teeth should be sectioned within minutes of beginning an extraction. Attempting to extract a nonsectioned tooth can sometimes be more inefficient and time-consuming, and uncomfortable for the patient, compared to extracting the same tooth sectioned. A tooth might require sectioning or bone removal if forceps or luxation forces cannot cause progressive tooth movement; if elevator instruments cannot be used without exerting excessive force on a neighboring tooth; if a tooth root is ankylosed, particularly with endodontically treated root tips, and needs intra-root sectioning to create an elevator insertion slot; if tooth roots are dilacerated, which often occurs with impacted mandibular third molars; or if the tooth particle is close to a major nerve and should be sectioned to minimize stress on the bone around the nerve. If a root is weak or thin, removal of septum bone around the roots and sectioning the roots through the furcation reduces the risk of root fracture during luxation. Circumferential bone removal around tooth particles is sometimes required to facilitate tooth mobility in response to luxation forces
37.
Luxating tooth roots that are connected by a furcation might require heavy forces, which can create stress planes within the surrounding alveolar bone that can fracture the bone or result in compression-induced necrosis of osteoblasts within the socket
456. These stress planes can theoretically extend beyond the volume of alveolar bone that the dentist has anesthetized, resulting in pain due to nerve stimulation within the un-anesthetized jawbone volumes located beyond the anesthetized bone. Sectioning the furcation, such that each root moves independently of the other roots in response to luxation forces, results in less force required to luxate the roots and in smaller stress planes propagated to the surrounding alveolar bone.
Bone removal should be minimized to reduce volume loss of the eventually healed socket and performed using irrigation in order to prevent temperature necrosis of bone remaining in the socket after tooth removal
1011. Removing the coronal aspect of septum bone increases the leverage of tooth particle movement, since the tooth particle can then be luxated into the space once occupied by the septum bone with increased degrees of freedom of rotational movement. The septum bone inside a socket can curl around roots, which can block tooth particle movement unless removed.
6. Luxating teeth with ellipsoid cross sections
Sectioning roots with ellipsoid cross sections results in the remaining tooth particles having more circular cross sections, which facilitates rotation within the socket on the tooth root long axis in response to luxation forces. Premolars are often ellipsoid in cross section, and are easier to remove if sectioned at the furcation and if the dentist removes alveolar bone within mesial or distal root concavities.
A maxillary molar palatal root with an ellipsoid cross section might be blocked from moving in response to luxation forces due to alveolar bone that curls around the lateral aspects of the palatal root. In these cases, the lateral curling bone can be removed, and the palatal root can be cut in an occlusal-to-apical direction in order to create a vertical slot. A straight elevator placed in the slot luxates one palatal root piece against the other, with the pieces providing both the dorsal and ventral elevator tip contact points. Luxation can cause a piece of the root to crack off, creating a space that provides increased freedom of movement for remaining palatal root pieces.
A canine can have a long root, be ellipsoid in cross section, and be bounded by thin buccal bone that can fracture during luxation, since heavy force might be needed to luxate a nonsectioned canine. The dentist can section the canine by drilling a mesial-to-distal slot approximately midway between the buccal and lingual dimension of the canine, ideally to the depth of the canine apex. The dentist then places an elevator into the slot and oscillates the elevator in a clockwise-to-counter-clockwise direction, which can fracture the root into one piece that is fractured from the canine apex and another piece that is connected to the apex. Hopefully, this luxation will not fracture or excessively compress the buccal bone. The piece that is not connected to the apex can be removed, and the other piece will have a more circular cross section and increased degrees of freedom of movement inside the socket due to the space created.
However, a single mesial-to-distal slot might not result in elevator-induced fracture of the canine root if the socket walls block the buccal and lingual aspects of the canine from shifting enough to cause a fracture. Here, a large amount of luxation force may be needed to fracture the canine pieces, which can result in fracture of the buccal plate. To prevent this, a second slot can be drilled into the canine in a buccal-to-lingual direction, located midway between the mesial and distal dimensions of the canine. This cuts the canine root longitudinally into four separate pieces, each with a relatively circular cross section, which can be split or luxated while exerting minimal force on the buccal bone, and the socket walls would minimally obstruct the movement of the pieces within the socket.(
Fig. 7)
 | Fig. 7A 4-way split of the coronal aspect of a maxillary central incisor with an ellipsoid cross section that is bounded by thin buccal bone that could fracture under luxation forces.
|
The piece that is attached to the canine apex will hopefully not fracture from the apex during luxation. If a fracture occurs, a root tip pick or a small straight elevator, ideally with a posterior curve of the working end, can be used to luxate the canine apical tip. Some sectioning with a surgical bur might be needed to remove bone around the root tip and to create a slot in the coronal aspect of the root tip in order to allow straight elevator access or a root tip pick to the root tip. Occasionally, drilling might be needed to access the root tip via an opening in the buccal bone, located approximately at the level of the root tip.
7. Luxating carious root tips
When extracting a root tip with coronal decay
3, the coronal root aspect might crumble under the forces of a straight elevator, resulting in loss of the elevator tip ventral contact points.(
Fig. 1) If the decay is removed until only hard tooth structure remains, the hard tooth structure might be subgingival, possibly with a concave occlusal surface, such that it can be difficult to fit a straight elevator tip between the root tip and the alveolar bone. Here, the root tip can be sectioned longitudinally to create one (or two) slots to allow elevator tip insertion.(
Fig. 7) The alveolar bone mesial and/or distal to the root tip might need to be removed to increase the degrees of freedom of root tip movement in response to luxation forces. If two neighboring carious root tips require extraction, removing the alveolar bone between them allows insertion of a straight elevator tip to a depth where both the dorsal and ventral tip surfaces contact hard tooth structure for leverage.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download