Abstract
A surgical approach involving the retromolar trigone, posterolateral maxilla, and pterygoid region is the most challenging in the field of maxillofacial surgery. The upper cheek flap (Weber-Ferguson incision) with subciliary extension and the maxillary swing approach have been considered as alternatives; however, neither approach provides sufficient exposure of the pterygoid region and the anterior portion of the mandibular ramus. In this report, we describe two cases in which a lower cheek flap approach was used for complete tumor resection in the retromolar trigone and the anterior mandibular ramus. This approach allows full exposure of the posterolateral maxilla and the pterygoid region as well as the retromolar trigone without causing major sensory disturbances to the lower lip. A mental nerve anastomosis after tumor resection was performed in one patient and resulted in approximately 90% sensory recovery in the lower lip. The lower cheek flap approach provides adequate exposure of the posterolateral maxilla, including the pterygoid, retromolar trigone, and mandibular ramus areas. If the mental nerve can be anastomosed during flap approximation, postoperative sensory disturbances to the lower lip can be minimized.
The posterior maxilla, pterygoid, and retromolar trigone are the most difficult areas to expose completely in the field of maxillofacial surgery. Tumors extending into this region pose a surgical challenge due to the anatomical complexity and the presence of various important structures. The upper cheek flap, known as the Weber-Ferguson approach, is one recommended surgical approach for this region; a subciliary extension increases the accessibility of the maxilla and maxillary sinus in this procedure1. However, this approach does not fully expose the pterygoid plate or the posterolateral maxilla. Recently, a modified lower cheek flap approach has been introduced, which allows exposure of the entire posterior maxilla and retromolar trigone. This method has been optimized to allow marginal resection of the anterior part of the mandibular ramus and full visualization of the posterolateral maxilla and pterygoid region2. One of the most serious risks of the modified lower cheek flap approach is persistent numbness of the lower lip due to injury to or severing of the mental nerve.
In this report, we describe two cases in which the modified lower cheek flap approach was used to approach tumors in the retromolar trigone, posterolateral maxilla, and/or anterior mandibular ramus. In one case, a mental nerve anastomosis was performed immediately following tumor resection. We report the long-term prognosis of these two cases as well as a review of the literature for surgical approaches to complicated anatomical areas, including the retromolar trigone, posterolateral maxilla, and pterygoid regions.
The ethical approval for this study was obtained from the Ethic Committee for Clinical Research at Gyeongsang National University Hospital (GNUH IRB-2012-09-004). Written informed consent was provided by all patients for use of their information, including clinical and radiological images.
A 50-year-old male presented to the Department of Oral and Maxillofacial Surgery at Gyeongsang National University Hospital (Jinju, Korea) complaining of difficulty opening his mouth for the past six months and an ulcerative lesion in the retromolar trigone area. He reported a history of hepatitis and diabetes mellitus and had been using tobacco and alcohol for more than 30 years. Clinical examination revealed an approximately 2-cm ulcerative lesion in the left retromolar trigone area.(Fig. 1. A) Computed tomography (CT) and magnetic resonance imaging scans confirmed the presence of a 2.8-cm contrast-enhancing lesion in the left maxilla and retromolar areas that extended to the left temporalis muscle. (Fig. 1. B, 1. C) Incisional biopsy of the primary site in the retromolar trigone area demonstrated poorly differentiated squamous cell carcinoma. Further assessment by positron emission tomography-CT scan showed no distant metastasis. The tumor was subsequently resected using a modified lower cheek flap approach with a maxillary vestibular extension incision. The level I, II, and III cervical lymph nodes were first removed using selective supraomohyoid neck dissection. Then, the tumor was excised from the primary site in conjunction with resection of the posterolateral maxillary and pterygoid regions and the anterior segment of the mandibular ramus.(Fig. 2) The exposed surgical field was covered by a skin graft. No malignant cells were observed in the frozen specimen harvested intra-operatively from the tumor bed. Following surgery, the patient was treated with concurrent chemo-radiotherapy (cisplatin, total 7,040 cGy/32 fraction) to prevent recurrence. Over a three-year follow-up period, there was no sign of tumor recurrence or distant metastasis, but the patient did develop a moderate mouth opening limitation (an approximately 30-mm maximum opening).(Fig. 3)
A 51-year-old male was referred to our department with swelling of the left cheek and a large radiolucent lesion in the left mandibular ramus visible on routine radiographs. CT scan revealed a wide destructive lesion on the left mandibular body and the anterior part of the ramus.(Fig. 4) No malignant cells were seen on fine-needle aspiration cytology. However, to completely excise the tumor from the mandibular body and ramus, a lower cheek flap approach with intentional mental nerve resection was planned. Anastomosis of the intentionally resected mental nerve was achieved through end-to-end suturing of the epineurium.(Fig. 5) Histopathology of the tumor was consistent with a multicystic ameloblastoma. Lower lip numbness was scored as 70% immediately after the procedure, which improved to 10% (90% sensory recovery) 24 months postoperatively. There was no disease recurrence during a 30-month follow-up period, after which dental implants were placed, and masticatory function was recovered.(Fig. 6)
Various surgical approaches to the posterolateral maxilla and retromolar trigone areas have been proposed. A non-invasive transoral approach is the first choice for relatively small intraoral lesions234. More extensive approaches are required to access the maxillary sinus, posterior maxilla, and/or pterygoid plates. These include the mandibular swing, Le Fort I osteotomy of the maxilla, upper cheek flap, and lower cheek flap12345678. Usually the upper cheek flap, a modified Weber-Ferguson incision with subciliary extension, is preferred for exposure of the posterior maxilla8. However, the upper cheek flap approach alone does not provide sufficient accessibility to the posterolateral wall of the maxillary sinus and the pterygoid plates2. Alternative approaches to consider are the maxillary swing and/or Le Fort I osteotomy for exposure of the deep portion of the maxilla4567. These methods are best suited for tumors located in the posterior wall of the maxilla and the retromaxillary areas and therefore do not fully expose the pterygoid and retromolar regions.
The lower cheek flap approach is suitable for exposure of the posterolateral maxilla and the anterior part of the mandibular ramus2. Balm et al.2 described the use of a lower cheek flap approach to resect tumors in the posterolateral maxillary and pterygoid regions. The flap was a modification of the routine submandibular incision used for selective neck dissection of level I, II, and III cervical lymph nodes2. The lower cheek flap approach allowed access to the retromolar trigone and pterygoid region; even the infratemporal fossa could be accessed when the proper upper vestibular releasing incision was added. This method produces a better cosmetic result than the upper cheek flap (Weber-Ferguson incision with subciliary extension). The lower cheek flap approach also allows for selective neck dissection for level I, II, and III cervical lymph node excision.
Unfortunately, severing of the mental nerve is required for complete flap elevation, which theoretically leads to lower lip numbness. In case 2 of this study, the mental nerve was intentionally severed and then anastomosed after tumor resection. The patient demonstrated approximately 90% recovery of the sensation to the lower lip two years postoperatively. When the inferior alveolar nerve can be preserved in the surgical field, the intentional severing then anastomosis of the mental nerve should reduce postoperative lower lip numbness.
In conclusion, the modified lower cheek flap approach provides optimal surgical exposure of the anterior portion of the mandibular ramus and the retromolar trigone areas. When proper upper vestibular releasing incisions are added, access to the posterolateral maxilla and pterygoid plates can be achieved. This method allows for a better cosmetic result than the upper cheek flap approach. If the inferior alveolar nerve is preserved, intentional severing and anastomosis of the mental nerve can reduce postoperative lower lip sensory disturbance.
Acknowledgements
The authors would like to thank the faculty members of the Department of Anesthesiology and the nursing staff at Gyeongsang National University Hospitals in Jinju and Changwon in Korea, who were involved in the management and care of the patients who took part in this study.
Notes
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (NRF-2014R1A1A2058807).
Authors' contributions: YHK collected and analyzed the patient data and substantially contributed to writing the manuscript. JHB and SJS assisted in the treatment of the patients and performed patient care. BWP carried out patient management and operations, collected the literature, and was another major contributor in writing the manuscript. All authors read and approved the final manuscript.
References
1. Lore JM, Medina JE. Partial and radical maxillectomy. In : Lore JM, Medina JE, editors. An atlas of head & neck surgery. 4th ed. Philadelphia: Elsevier Saunders;2005. p. 236–249.
2. Balm AJ, Smeele LE, Lohuis PJ. Optimizing exposure of the posterolateral maxillary and pterygoid region: the lower cheek flap. Eur J Surg Oncol. 2008; 34:699–703. PMID: 18029135.

3. Alves FRA, Granato L, Maia MS, Lambert E. Surgical approaches to juvenile nasopharyngeal angiofibroma: case report and literature review. Int Arch Otorhinolaryngol. 2006; 10:e162–e166.
4. Girish Rao S, Sudhakara Reddy K, Sampath S. Le Fort I access for juvenile nasopharyngeal angiofibroma (JNA): a prospective series of 22 cases. J Craniomaxillofac Surg. 2012; 40:e54–e58. PMID: 21458288.
5. Sumi T, Tsunoda A, Shirakura S, Kishimoto S. Partial maxillary swing approach for removal of the tumors in the retromaxillary area. Auris Nasus Larynx. 2009; 36:567–570. PMID: 19261408.

6. Wei WI, Ho CM, Yuen PW, Fung CF, Sham JS, Lam KH. Maxillary swing approach for resection of tumors in and around the nasopharynx. Arch Otolaryngol Head Neck Surg. 1995; 121:638–642. PMID: 7772315.

7. Fee WE Jr, Moir MS, Choi EC, Goffinet D. Nasopharyngectomy for recurrent nasopharyngeal cancer: a 2- to 17-year follow-up. Arch Otolaryngol Head Neck Surg. 2002; 128:280–284. PMID: 11886344.
8. Jian XC, Liu JP. A new surgical approach to extensive tumors in the pterygomaxillary fossa and the skull base. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 95:156–162. PMID: 12582354.

Fig. 1
Preoperative clinical and radiographic views of Case 1. A. Arrow indicates the firm mass on the left side of the retromolar trigone. B, C. Positron emission tomography-computed tomography and magnetic resonance imaging show an isolated hot spot involving the anterior mandibular ramus, posterolateral maxilla, and retromolar trigone (arrows).
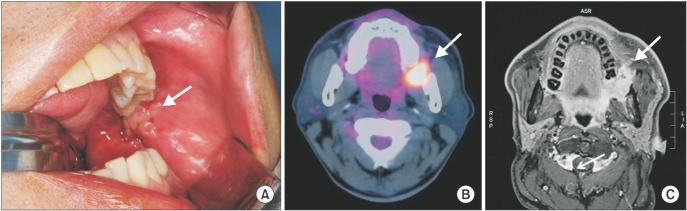
Fig. 2
Intraoperative photographs of Case 1. A. Lower cheek flap with upper vestibular incision allowing complete exposure of posterolateral maxilla, mandibular ramus, and retromolar trigone. A, B. Surgical field showing excision of the primary tumor along with a partial posterior maxillectomy and a marginal posterior (ramus) mandibulectomy. This approach also allows selective neck dissection I-III. C-E. Photographs show the surgical specimens of the selective neck dissection (C), posterior maxillectomy with pterygoid plate excision (arrow) (D), and marginal mandibulectomy with coronoid process excision (E).
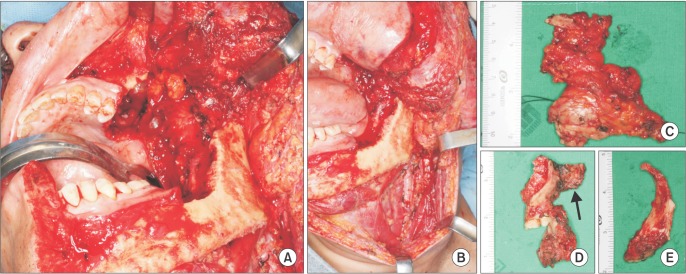
Fig. 3
Postoperative clinical and radiographic views of Case 1. A, B. Six months after the operation, the patient showed approximately 40 mm of maximum mouth opening and an acceptable facial scar. C. Two-year postoperative panoramic view indicating an intact inferior alveolar canal and mental foramen (arrows).
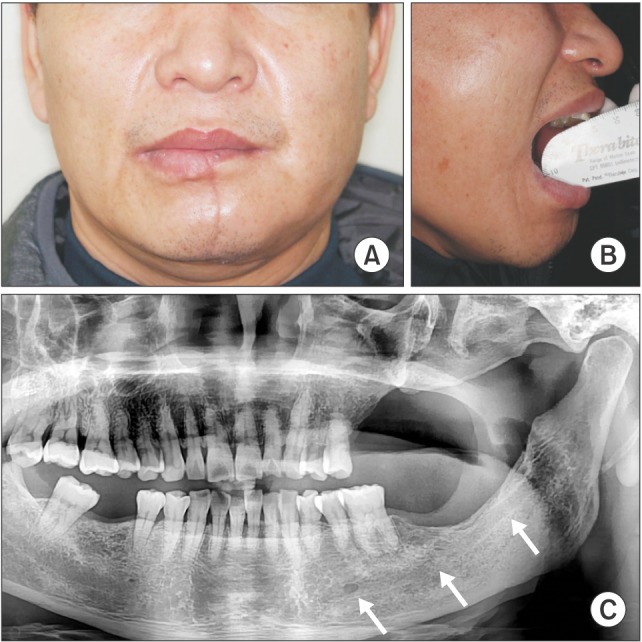
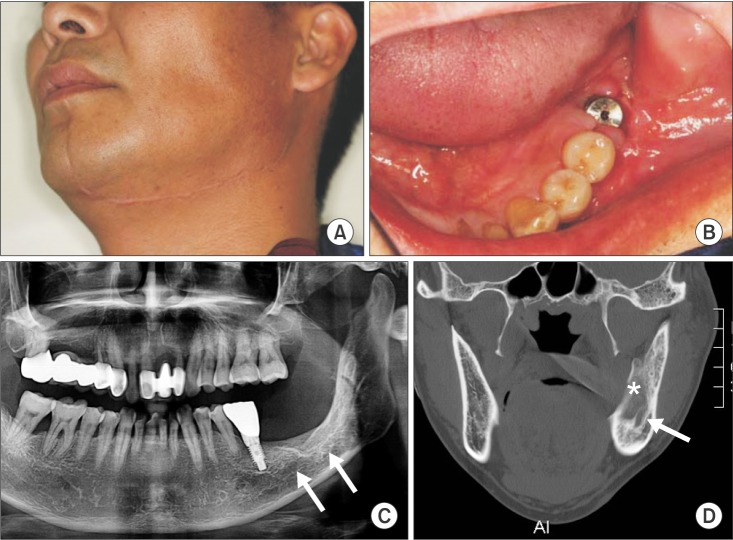
Fig. 4
Preoperative radiographs of Case 2. A-C. Large radiolucent lesion evident in the left mandibular body and ramus (arrows).
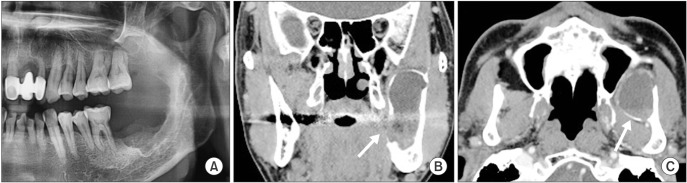
Fig. 5
Intraoperative photographs of Case 2. A. During creation of the lower cheek flap, the mental nerve was ligated and marked with suture material (arrow), then it was severed and the flap was elevated. B, C. The tumor (arrow) was completely excised from the anterior mandibular ramus while preserving the inferior alveolar nerve. D. Following excision of the tumor, the mental nerve was anastomosed using 7-0 nylon suture (arrow).
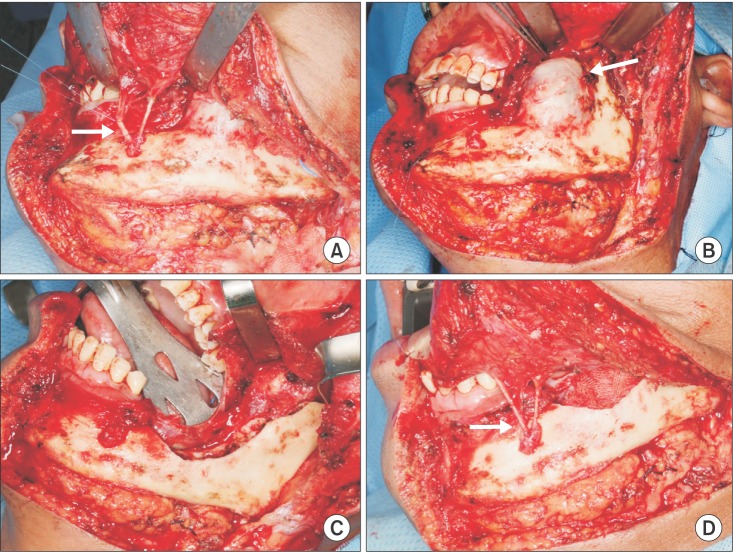
Fig. 6
Postoperative clinical and radiographic views of Case 2. A, B. Six months postoperative, the surgical wounds had healed and a dental implant was placed at the surgical site. C, D. On panoramic and computed tomography views obtained 1-year postoperative, regenerated new bone tissue (asterisk) and an intact inferior alveolar canal were detected (arrows). In addition, a dental prosthesis was visible at the site of the left mandibular first molar.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download