Abstract
Peripheral odontogenic myxoma is a rare odontogenic tumor representing an extra osseous counterpart of central odontogenic myxoma. It is commonly seen in gingiva between the 3rd and 4th decades of life and appears predominantly in females. Compared to central odontogenic myxoma, it is a less aggressive, slow-growing lesion with a low recurrence rate. However, close postoperative follow-up is required because of the unlimited growth potential of incompletely removed lesions. It shares many features with other soft tissue myxoid proliferations occurring in the oral cavity and hence needs to be differentiated from them. Very few cases of peripheral odontogenic myxomas have been reported and, to the best of our knowledge, no case has been reported in a pediatric patient. We present an unusual case of peripheral odontogenic myxoma occurring in a 12-year-old girl located in the anterior mandibular gingiva, with an emphasis on differential diagnosis.
Odontogenic myxomas are relatively rare benign odontogenic tumors that arise from the ectomesenchyme of the tooth-forming apparatus and are composed of spindle shaped/rounded/angular cells embedded in abundant mucoid stroma. Odontogenic myxomas can be categorized into central and peripheral variants1234. Very few case reports of peripheral odontogenic myxomas (POMs) are available in the literature. Clinically and histologically, POMs resemble many other soft tissue lesions. Hence, recognizing and diagnosing POMs is necessary for the careful planning of conservative treatment and follow-up to rule out intraosseous extension5. This article presents a rare case of POM in a pediatric patient with a special emphasis on differential diagnosis.
A 12-year-old girl presented with a growth on the mandibular gingiva between tooth #31 and #32 (Fig. 1. A) that appeared three months prior. It was 1×1.5 cm in size, firm in consistency, and adherent to the mandibular gingiva but not fixed. The overlying mucosa was normal in color and texture.(Fig. 1. A) Radiologically, the intraoral periapical view showed drifting of tooth #31 and #32 without any erosion of alveolar bone.(Fig. 1. B) Based upon the clinical and radiographic findings, the lesion was provisionally diagnosed as a pyogenic granuloma. The lesion was completely excised and curetted under local anesthesia.
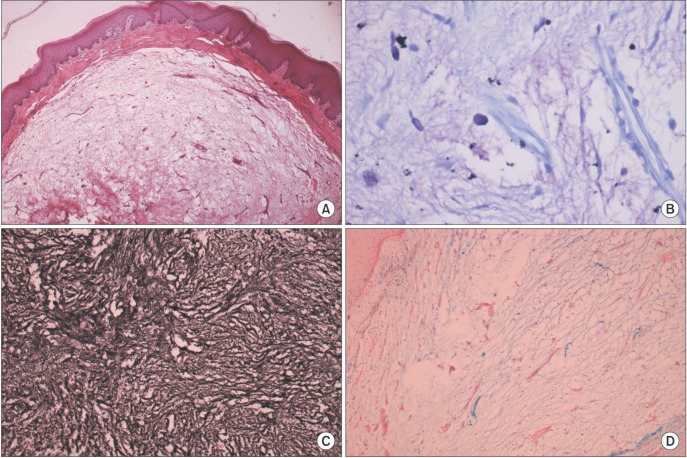
Gross examination of the excised tissue revealed a soft-to-firm grayish white pedunculated mass. Microscopically, an H&E stained section showed well-circumscribed lesional tissue separated from the overlying stratified squamous parakeratinized epithelium by fibrous tissue. The lesional tissue consisted of relatively acellular loose myxoid stroma with scattered spindle-to-stellate-shaped cells and many delicate proliferating capillaries. A minimal amount of collagen fibers was seen.(Fig. 2. A) The presence of numerous mast cells (MCs) was confirmed by toluidine blue staining.(Fig. 2. B) The lesional tissue was strongly positive for reticulin staining and showed alcinophilia.(Fig. 2. C, 2. D, respectively)
Lesional tissue showed vimentin positivity and S-100 negativity. Based on these findings, a final diagnosis of POM was established. After excision of the lesion, the migrated teeth reverted to their normal position. The two-year follow-up period was uneventful.
Odontogenic myxoma is a mesenchymal lesion of uncertain histogenesis that microscopically mimics dental pulp or follicular connective tissue12. Odontogenic myxomas are classified as central/intraosseous and peripheral/extra osseous variants23.
POM is a very rare lesion with a reported incidence less than that of other peripheral odontogenic tumors4; data on POM clinicopathologic features remain scarce4.
Relevant literature suggests that peripheral myxomas of the intraoral tissues should be named POMs because soft tissue myxomas are usually seen extrafacially in skeletal muscles, dermal and subcutaneous tissues and do not occur in the oral cavity5.
Several theories have been put forth regarding the pathogenesis of POM. One hypothesis states that altered primitive fibroblast/myofibroblasts produce excess mucopolysaccharides. And most of these cells are incapable of forming mature collagen. Other authors have suggested an origin derived from mesenchymal cells, such as dental papilla, dental follicle, or periodontal ligament56.
POMs most commonly present clinically as pedunculated or sessile, painless, exophytic masses located in the gingiva45. Most of the reported cases of POMs occur in 4th to 6th decade of life4578910. In contrast, our case was found in a 12-year-old girl. POMs show a predilection for females and most reported cases have occurred in the maxilla245789, with only a few cases including the present case reported in the mandible.
The size of the lesions ranges from one centimeter to several centimeters, with two reported cases being very large4.
Radiologically, some of the reported cases of POMs showed displacement of the associated teeth without root resorption. Localized erosion of alveolar bone was also observed in some cases458. In our case, the lesion caused tooth displacement without any bony erosion.
Clinically, POMs may mimic similar lesions like peripheral odontogenic lesions, peripheral giant cell granuloma, fibroma, lipoma, pyogenic granuloma, giant cell fibroma, traumatic fibroma, neurofibroma, focal oral mucinosis and other malignant and metastatic connective tissue tumors24571011. Histological examination is necessary to differentially diagnose these lesions.
POMs are poorly circumscribed myxoid proliferations outside the bone. They show little encapsulation and their rapid growth may be due to an accumulation of mucoid ground substance mimicking an aggressive neoplasm. The neoplasm is composed of haphazardly arranged stellate, spindle shaped and round cells in a loose myxoid stroma. Typically, a delicate vascular network and stellate fibroblasts are diagnostic of POM4. Odontogenic epithelial rests may not be obvious in most lesions and are not necessary for establishing a final diagnosis5.
Interestingly, in our case of POM, we found a scattered distribution of MCs. MCs may also play an important role in the growth and expansion of odontogenic tumors and their presence is associated with poor prognosis1213.
It has been suggested that the MCs are associated with remodeling of the extracellular matrix in neoplastic alterations as they produce and release proteolytic enzymes favoring the migration of both endothelial and tumor cells as well as the release of angiogenic factors stored within the stromal tissue, leading to a higher degree of aggressiveness of odontogenic myxoma1214. However, the presence of MCs has not been reported previously in POMs.
Histologically, the differential diagnosis of POM should include myxoid neurofibroma, myxoid chondrosarcoma, and myxoid liposarcoma, chondromyxoid fibroma, myxoid chondrosarcoma, a myxoid change in fibrosarcoma, botryoid type embryonal rhabdomyosarcoma and pleomorphic adenoma4. Awareness of the potential diagnostic pitfalls as well as careful evaluation of the clinical, radiological and characteristic histopathologic findings can narrow down the differential diagnosis7. Nerve sheath myxoma typically exhibits lobulated mucoid tissue containing stellate and spindle shaped cells, and condensed connective tissue representing perineurium surrounding the lesion. MCs are characteristically present in this lesion11. Oral focal mucinosis is clinically indistinguishable from other similar lesions; however, the connective tissue is alcinophilic and lacks reticulin fibres15. Our case showed strong positivity for reticulin staining, thus ruling out oral focal mucinosis.
In our case, we confirmed the results of other studies with respect to S-100 negativity and vimentin positivity. The diagnostic value of immunohistochemistry (IHC) in odontogenic myxomas is limited as the neoplastic cells share antigenic characteristics with many non-odontogenic myxoid proliferations and a specific marker for cells of dental ectomesenchymal origin is lacking4. However, IHC findings help to differentiate these lesions from other myxoid lesions.
If left untreated, POMs have unlimited growth potential. POMs without bone destruction are treated by simple excision while those with bone destruction require excision and marginal curettage. POM has a much lower recurrence rate (3%-8%) than central odontogenic myxoma (10%-33%). Therefore, a carefully planned conservative enucleation or semi-radical approach is justified24516. Close follow-up of these lesions is necessary to rule out intraosseous extension and recurrence.
We conclude that special stains and IHC are valuable tools for the differential diagnosis of these lesions. Overtreatment of POMs should be avoided through the use of definitive diagnosis, especially in pediatric patients, as it may affect the alignment and eruption of teeth. The role of MCs in POMs needs to be further evaluated, since POMs with MCs have not been reported previously.
Acknowledgements
The authors would like to thank Bharati Vidyapeeth Deemed University Dental College and Hospital, Sangli, for the necessary support. The authors are also thankful to Dr. Jaydeep Pol, M.D. Pathology, Mahatma Gandhi Cancer Institute, Miraj, for IHC analysis.
References
1. Brannon RB. Central odontogenic fibroma, myxoma (odontogenic myxoma, fibromyxoma), and central odontogenic granular cell tumor. Oral Maxillofac Surg Clin North Am. 2004; 16:359–374. PMID: 18088737.

2. Jain VK, Reddy SN. Peripheral odontogenic myxoma of maxillary gingiva: a rare clinical entity. J Indian Soc Periodontol. 2013; 17:653–656. PMID: 24174762.

3. Reichart PA, Philipsen HP. Odontogenic tumors and allied lesions. London: Quintessence Publishing;2004. p. 189–196.
4. Raubenheimer EJ, Noffke CE. Peripheral odontogenic myxoma: a review of the literature and report of two cases. J Maxillofac Oral Surg. 2012; 11:101–104. PMID: 23449257.

5. Aytac-Yazicioglu D, Eren H, Görgün S. Peripheral odontogenic myxoma located on the maxillary gingiva: report of a case and review of the literature. Oral Maxillofac Surg. 2008; 12:167–171. PMID: 18642035.

6. Mehendiratta M, Rehani S, Solomon MC. The histological spectrum of myxoma, myxofibroma/fibromyxoma and odontogenic fibroma: “a chicken and egg situation”. IOSR J Dent Med Sci. 2012; 1:3–5.
7. Perrotti V, Rubini C, Fioroni M, Piattelli A. Soft tissue myxoma: report of an unusual case located on the gingiva. J Clin Periodontol. 2006; 33:76–78. PMID: 16367860.

8. Shimoyama T, Horie N, Kato T, Tojo T, Nasu D, Kaneko T, et al. Soft tissue myxoma of the gingiva: report of a case and review of the literature of soft tissue myxoma in the oral region. J Oral Sci. 2000; 42:107–109. PMID: 10989594.

9. Whitt J, Barker B, Cobb C. Peripheral odontogenic myxoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 100:187–188.

11. Regezi JA, Sciubba JJ, Jordan RCK. Oral pathology: clinical pathologic correlations. 5th ed. St. Louis: Saunders Elsevier;2008. p. 272–273.
12. de Assis Caldas Pereira F, Gurgel CA, Ramos EA, Vidal MT, Pinheiro AL, Jurisic V, et al. Distribution of mast cells in benign odontogenic tumors. Tumour Biol. 2012; 33:455–461. PMID: 22125027.
13. Mosqueda-Taylor A. New findings and controversies in odontogenic tumors. Med Oral Patol Oral Cir Bucal. 2008; 13:E555–E558. PMID: 18758398.
14. Martínez-Mata G, Mosqueda-Taylor A, Carlos-Bregni R, de Almeida OP, Contreras-Vidaurre E, Vargas PA, et al. Odontogenic myxoma: clinico-pathological, immunohistochemical and ultrastructural findings of a multicentric series. Oral Oncol. 2008; 44:601–607. PMID: 17996487.

15. Barnes L, Eveson JW, Reichart P, Sidransky D. World Health Organization classification of tumors. Pathology and genetics of head and neck tumours. Lyon: IARC Press;2005. p. 197.
16. Choi SH, Jeong JC, Song MS, Seo JH, Kim SB, Jun CH. A case of odontogenic myxoma related to both impacted canine teeth in the mandible. J Korean Assoc Oral Maxillofac Surg. 2003; 29:64–67.
Fig. 1
A. Clinical photograph showing the gingival mass extending buccolingually between teeth #31 and #32. B. Occlusal radiograph showing drifting of #31 and #32 without bone involvement.
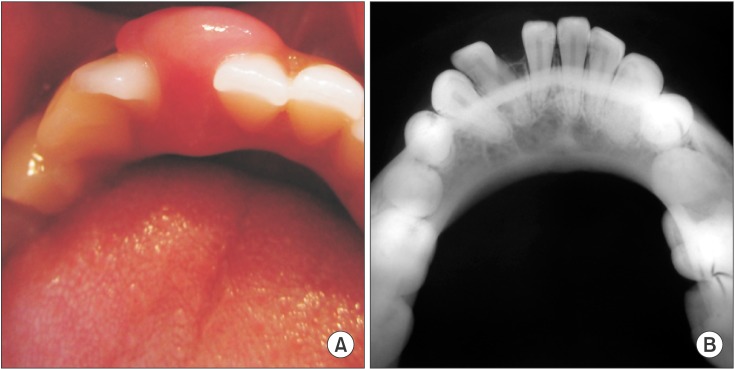
Fig. 2
2. A. H&E stained section (×10) showing loose myxomatous lesional tissue separated from the overlying stratified epithelium by a fibrous capsule. B. Toluidine blue-stained section (×40) showing mast cells in myxoid stroma. C. Reticulin-stained section (×10) showing strong positivity. D. Lesional tissue showing reactivity to Alcian blue staining (×10).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download