Abstract
Amniotic constriction band is a rare clinical entity with varied manifestations that range from a combination of congenital malformations to isolated malformations that are unique to each patient. The etiology of this entity remains unknown. Herein, we highlight two cases of amniotic constriction band that presented to our unit with unique clinical characteristics. To the best of our knowledge, an isolated circumferential band of scarring on the face with ocular involvement, as demonstrated by the first case, and a combination of bilateral complete cleft lip and palate with bilateral microphthalmia, auto-amputation of the right thumb, and a constriction band on the left thumb, as demonstrated by the second case, are extremely rare presentations of amniotic constriction band that were not previously reported in the literature and therefore necessitate a special mention. We discuss potential etiologies for these cases and review the existing literature on this entity.
Amniotic constriction band (ACB) encompasses a constellation of congenital malformations characterized by extreme variability in clinical presentation that ranges from simple ring constrictions and minor digital defects to complex, bizarre, multiple congenital anomalies that are incompatible with life1. The incidence ranges from 1:1,200 to 1:15,000 live births and 178:10,000 spontaneous abortions2. The genders are equally affected, with nearly all cases being sporadic; evidence of familial transmission is extremely rare34. Even now, the exact etiology of ACB remains unknown.
The extremely variable clinical features between patients and the unusual nature of this constellation of findings, coupled with our current lack understanding about the etiology, are all reflected in the fact that the entity has been described in the literature using 34 different terms, including amnion rupture sequence, aberrant tissue band syndrome, ADAM (amniotic deformity, adhesions, mutilations) complex, constriction band syndrome, and Streeter's dysplasia5. The word “syndrome” has been used to describe this entity, but is controversial because there are no classic, consistently present, or defining features of ACB, as seen in other syndromes. Rayan6 evaluated the nomenclature related to this entity and concluded that ACB was the most appropriate terminology to reflect both its etiology and description; thus, we adopt the same terminology herein.
We hereby present two ACB cases that reported to our unit with unique clinical manifestations. To the best of our knowledge, the isolated circumferential band of facial scarring with ocular involvement that was present in the first case and the combination of bilateral complete cleft lip and palate with bilateral microphthalmia, auto-amputation of the right thumb, and a constriction band on the left thumb that was present in the second case are extremely rare and have not been previously reported in the literature. Herein, we discuss possible etiologies and review the existing literature on ACB. Through these cases, we add new examples of patients with a combination of malformations considered to be part of the ACB spectrum.
The written informed consents were obtained from all patients' guardian.
A 2-year-old boy presented to our unit with facial deformities from birth. He was the first child of non-consanguineous parents born after a regular pregnancy and delivered by caesarean section. The mother suffered no medical conditions and did not use any drugs or consume alcohol during her pregnancy. The family history was negative for craniofacial or other congenital malformations. An echocardiogram performed immediately following delivery showed a small defect in the peri-membranous portion of the patient's ventricular septum. A magnetic resonance imaging of the brain performed 26 days after birth showed normal findings. Abdominal ultrasound was also normal.
The patient's developmental milestones were normal. On clinical examination, a circumferential band of scarring was noted on the face. The band of scarring extended from the base of the right side of the nose toward the outer canthus of the right eye, extending in an oblique direction toward the scalp and then curving in a circular manner to involve the left supra-orbital ridge and extend to the base of the nose on the left side.(Fig. 1. A-C) The upper and the lower eyelids of the right eye together with the lower palpebral conjunctiva and globe were involved in the scarring, causing proptosis, corneal opacity, prolapse of the lower palpebral conjunctiva, and loss of vision in the right eye.(Fig. 1. D) The vision in the left eye was intact, although mild traction of the lower eyelid caused increased scleral exposure of the left eye. No other abnormalities were noted.
A computed tomography scan of the brain and facial bones revealed that the right orbit was smaller in volume than the left.(Fig. 2. A) The anterior fontanelle was excessively large due to defects observed in the frontal bone on the left side. (Fig. 2. B) No other significant findings were observed.
The patient was operated on by a team consisting of a cleft surgeon, a plastic surgeon, and an oculoplastic surgeon, and the constriction band of scarring in relation to the base of the nose was excised and closed in a straight line. In the second surgical stage, the bilaterally exposed scleral was reduced by performing bilateral oculoplastic surgery using advancement flaps.(Fig. 3) These procedures were carried out solely to improve the patient's aesthetic appearance. Postoperative healing was uneventful although some degree of right palpebral conjunctival prolapse was still present. The child is scheduled for future reconstructive procedures to further improve his overall facial appearance.
A 4-year-old boy was referred to our unit with a bilateral cleft lip and palate and limb malformations. He was the first child of non-consanguineous parents born after a regular pregnancy and delivered by caesarean section. The mother had no history of drug or alcohol consumption during her pregnancy. Her maternal obstetric history did not suggest any antenatal damage to the fetus. The family history was negative for craniofacial or other congenital malformations. An echocardiogram revealed a congenital heart disease, tetralogy of Fallot, for which the child underwent surgery at 3 years of age. Abdominal ultrasound was normal.
A gross developmental delay was observed in the patient. On clinical examination, the following malformations were asymnoted: bilateral microphthalmia, bilateral complete cleft lip and palate with pre-maxillary excess, auto-amputation of the thumb of the right hand, and constriction band at the most-proximal aspect of the left thumb.(Fig. 4)
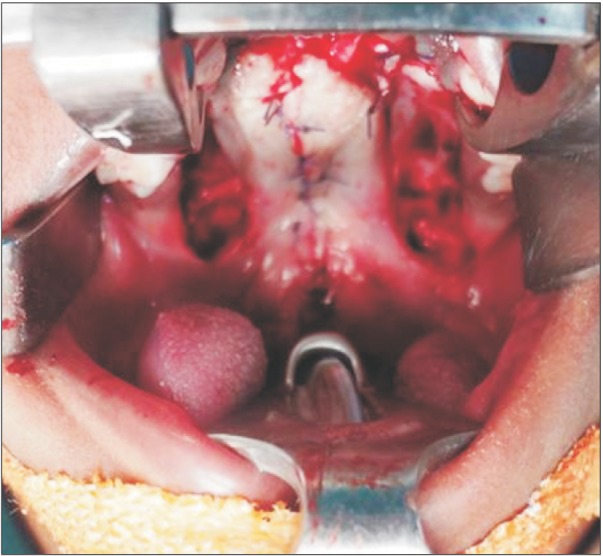
Following cardiologic clearance, the patient underwent an operation to close the bilateral cleft lip using the Mulliken technique.(Fig. 5) Three months later, a second surgery was performed to repair the bilateral cleft palate. Finally, 6 months later, vomerine osteotomy was performed to correct the premaxillary excess.(Fig. 6, 7) Postoperative healing was uneventful.
Among 3% of the total body malformations, ACB accounts for 1% to 2%2. The classic feature of ACB is involvement of multiple extremities to varying degrees, the most common being limb or digit amputations, constriction rings, and acrosyndactyly 5. Additional findings can include talipes equinovarus and, less commonly, scoliosis. Even rarer are craniofacial abnormalities, such as cleft lip or cleft palate, body wall defects, and internal organ abnormalities57. Varying craniofacial disturbances, like asymmetric facial clefts; orbital defects including anophthalmos, microphthalmos, enophthalmos, and corneal abnormalities; central nervous system malformations, such as anencephaly, encephalocele, or asymmetric meningocele; and calvaria defects can result in compression of the fetal head or face by the bands2. Sometimes, an isolated constriction band involving the digits, extremities, neck, thorax, abdomen, or any other body part can be the sole presentation of ACB18910. Because of such a wide spectrum of possible anomalies and many combinations of their simultaneous appearance, there are no two identical ACB cases. We also observed significant variations in the clinical ACB cases reported here. After reviewing the existing literature, we did not come across a single case of isolated circumferential band with facial scarring, indicating this is an extremely rare presentation. Similarly, the constellation of malformations noted in the second case has also not previously been reported in the literature.
The etiology of ACB has been debated in the literature for nearly eight decades, with no clear consensus. A number of theories have been proposed by various authors to explain the pathogenetic mechanism of ACB. The most widely accepted theory is amniotic disruption or extrinsic theory, proposed by Torpin11 in 1965. According to this theory, amniotic rupture is followed by amniotic fluid loss and extrusion of all or parts of the fetus into the chorionic cavity. In this limited space, the fetus is subjected to compression with the fetal limbs or other body parts becoming entangled in the shriveled, rolled remnants of the amnion. The exact nature of the anomalies depends on the timing of amniotic rupture during pregnancy as well as the location and degree of compression of the underlying structures. Higginbottom et al.12 found that early damage (i.e., before 45 days of gestation) produced severe facial clefts and severe defects of the brain and calvarium, while late damage (i.e., after 45 days of gestation) resulted in limb involvement with no facial clefting or central nervous involvement.
Streeter's intrinsic or embryonic dysplasia theory suggests that fetal disruptions result from imperfect histiogenesis13. Normal programmed cell death, which occurs during embryogenesis, is perturbed in ACB cases, resulting in abnormal functioning of ectodermal placodes, which are involved in the formation of many organs. Vascular disruption theory proposed by Van Allen14 suggests that the defect genesis is due to interruption of the blood supply during embryogenesis. Even with the multitude of existing theories, it is difficult to explain the different malformations of ACB across all patients using a single theory.
The first patient presented with circumferential band on his face with ocular involvement and defects to the frontal bone. Amniotic disruption theory appears to be the most plausible explanation for this particular banding. The corneal opacity observed in the right eye might have been caused by the amniotic band adhering to the cornea, with possible perforation.
The second patient presented with bilateral complete cleft lip and palate with premaxillary excess and bilateral microphthalmia, auto-amputation of the right thumb, constriction band on the left thumb, and syndactyly of the first and second toes of both feet. Congenital heart disease in the form of tetralogy of Fallot was also noted. The clefting observed in the second patient was a primary clefting that formed when fusion between the nasal and maxillary processes or maxillary and mandibular processes was disturbed before the transformation phase was complete15. This is in contrast to asymmetrical and bizarre craniofacial clefting that corresponds to no recognized appositional lines of embryonic development, which is usually seen in ACB and therefore is not typical of similar ACB-associated defects516. It is likely that, in this instance, the presence of cleft lip and cleft palate in association with digit malformations, regardless of whether they are auto-amputations or constriction rings, is a coincidence. If this is so, then the digit malformations can best be explained by extrinsic theory.
Obstetric ultrasound, performed as early as 12 weeks gestation, can detect amniotic bands that appear as linear echoes floating in the amniotic fluid217. This early detection helps in counseling parents who might have to consider fetal surgery in utero or, in cases of gross malformations, pregnancy termination. Three-dimensional or four-dimensional ultrasound, as well as magnetic resonance imaging, offer more sensitive prenatal ACB diagnosis17.
ACB should be part of differential diagnoses for all complex asymmetrical malformations of the extremities, face, and body wall (e.g., amniotic folds, short umbilical cord syndrome, and extra-amniotic pregnancy)318.
ACB management is mostly surgical and requires a unique approach for each case. A multidisciplinary approach to resolve the multitude of problems associated with this entity is usually required. Management should focus on improving function and development while providing a more acceptable aesthetic appearance. The first case had a circumferential band of scarring on the face, as opposed to the primary clefting observed in the second case. Although an improved cosmetic outcome was achieved in the second case with respect to the facial clefting, it was difficult to achieve the same outcome for the first case due to the presence of scar tissue. Reconstruction is extremely challenging in such cases, and such children require multiple surgical procedures to achieve a desired cosmetic outcome.
In conclusion, ACB represents a rare congenital abnormality with varied clinical presentations that are unique to each patient. Our cases have different clinical presentations, neither of which has been previously described in the literature and therefore require a detailed report. Although their etiologies are unknown, both cases point toward the extrinsic theory of pathogenesis. Cleft surgeons should be aware of the range of clinical presentations that are possible for ACB and should consider this entity in the differential diagnoses for complex and asymmetrical malformations of the face, limbs, or body wall. Management can be extremely challenging in cases presenting with extensive scarring. Nevertheless, a multidisciplinary approach for management with a treatment plan specific to the case is often required to ensure a desired cosmetic outcome.
References
1. Ciloglu NS, Gumus N. A rare form of congenital amniotic band syndrome: total circular abdominal constriction band. Arch Plast Surg. 2014; 41:290–291. PMID: 24883282.

2. Matic A, Komazec J. Amniotic band syndrome. Acta Medica Medianae. 2009; 48:44–48.
3. Das D, Das G, Gayen S, Konar A. Median facial cleft in amniotic band syndrome. Middle East Afr J Ophthalmol. 2011; 18:192–194. PMID: 21731335.

4. Braude LS, Miller M, Cuttone J. Ocular abnormalities in the amniogenic band syndrome. Br J Ophthalmol. 1981; 65:299–303. PMID: 6786324.

5. Goldfarb CA, Sathienkijkanchai A, Robin NH. Amniotic constriction band: a multidisciplinary assessment of etiology and clinical presentation. J Bone Joint Surg Am. 2009; 91(Suppl 4):68–75.

7. Doi Y, Kawamata H, Asano K, Imai Y. A case of amniotic band syndrome with cleft lip and palate. J Maxillofac Oral Surg. 2011; 10:354–356. PMID: 23204754.

8. Martínez-Frías ML. Epidemiological characteristics of amniotic band sequence (ABS) and body wall complex (BWC): are they two different entities? Am J Med Genet. 1997; 73:176–179. PMID: 9409868.

9. Kim JB, Berry MG, Watson JS. Abdominal constriction band: a rare location for amniotic band syndrome. J Plast Reconstr Aesthet Surg. 2007; 60:1241–1243. PMID: 17950186.

10. Kashyap S, Shanker V, Sharma N. Amniotic band: a rare presentation. Indian J Dermatol. 2015; 60:200–202.

11. Torpin R. Amniochorionic mesoblastic fibrous strings and amnionic bands: associated constricting fetal death. Am J Obstet Gynecol. 1965; 91:65–75. PMID: 14245093.
12. Higginbottom MC, Jones KL, Hall BD, Smith DW. The amniotic band disruption complex: timing of amniotic rupture and variable spectra of consequent defects. J Pediatr. 1979; 95:544–549. PMID: 480028.

13. Streeter GL. Focal deficiencies in fetal tissues and their relation to intra-uterine amputation. Contrib Embryol Carnegie Inst. 1930; 22:1–44.
14. Van Allen MI. Fetal vascular disruptions: mechanisms and some resulting birth defects. Pediatr Ann. 1981; 10:219–233. PMID: 7254912.
15. van der Meulen JC, Mazzola R, Vermey-Keers C, Stricker M, Raphael B. A morphogenetic classification of craniofacial malformations. Plast Reconstr Surg. 1983; 71:560–572. PMID: 6828591.

16. Jones KL, Smith DW, Hall BD, Hall JG, Ebbin AJ, Massoud H, et al. A pattern of craniofacial and limb defects secondary to aberrant tissue bands. J Pediatr. 1974; 84:90–95. PMID: 12119963.

17. Merrimen JL, McNeely PD, Bendor-Samuel RL, Schmidt MH, Fraser RB. Congenital placental-cerebral adhesion: an unusual case of amniotic band sequence. Case report. J Neurosurg. 2006; 104(5 Suppl):352–355. PMID: 16848094.
18. Burk CJ, Aber C, Connelly EA. Ehlers-Danlos syndrome type IV: keloidal plaques of the lower extremities, amniotic band limb deformity, and a new mutation. J Am Acad Dermatol. 2007; 56(2 Suppl):S53–S54. PMID: 17224388.

Fig. 1
Clinical presentation of the circumferential constriction band on the face in Case 1. A. Frontal view showing the constriction band on the face. B. Right lateral view showing the extent of the constriction band on the scalp. C. Left lateral view showing the extent of the constriction band. D. Close-up view to appreciate the ocular involvement.

Fig. 2
Three-dimensional computed tomographic view of the facial skeleton in Case 1. A. View demonstrating the smaller dimensions of the right orbit as compared to the left. The right orbit measured 2.9×2.1 cm in greatest dimensions whereas the left orbit measured 3.0×2.6 mm in greatest dimensions. B. View demonstrating a defect in the frontal bone on the left side.
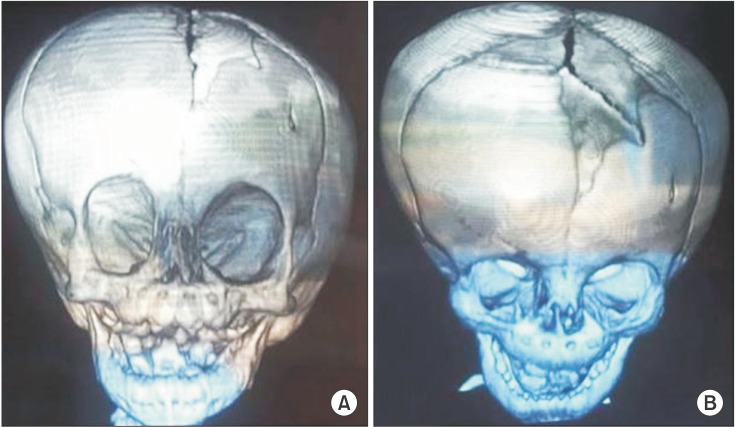
Fig. 3
Intraoperative and postoperative photographs of Case 1. A. Intraoperative photographs of bilateral oculoplastic surgery. B. Postoperative photographs at 6 months from surgery.

Fig. 4
Clinical presentation of Case 2. A. Frontal view showing bilateral complete cleft lip, premaxillary excess and bilateral microphthalmia. B. Photograph of the right hand showing auto-amputation of the thumb. C. Photograph of the left hand showing constriction band on the left thumb.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download