This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
The aim of this study was to investigate the effects of advancement magnitude and changes in mandibular plane angle on the stability of mandibular advancement.
Materials and Methods
This retrospective cohort study evaluated the postoperative stability of mandibular advancement in class II skeletal subjects who underwent bilateral sagittal split osteotomy. Radiographs taken preoperatively, immediately postoperatively and 1 year postoperatively were traced and analyzed using linear and angular measurements. To determine horizontal and vertical relapse, an X-Y coordinate system was established in which the X-axis was constructed by rotating S-N downward by 7° (approximation of the Frankfort horizontal plane) and the Y-axis was defined as a line perpendicular to the X-axis and passing through the point Sella. For certain reference points including point A, point B, pogonion and menton, the perpendicular distance between each point and both axes was determined and cephalometric variables were recorded as X and Y coordinates.
Results
Twenty-five subjects were studied. A significant correlation between the amount of mandibular advancement and relapse in the B point (vertical and horizontal) and the pogonion point was observed (vertical and horizontal, P<0.001). Evaluation of data demonstrated a positive correlation between the mandibular plane angle (SN/ML) change and vertical relapse in the B point (P<0.05). A simple regression model demonstrated that 74% of horizontal relapse and 42.3% of vertical relapse in the B point was related to the amount of mandibular advancement. The receiver operating characteristic test showed that 8.5 mm mandibular advancement is related to a relapse rate of 1 mm or more in the pogonion, vertically or horizontally.
Conclusion
The magnitude of mandibular advancement is a stronger surgical predictor for horizontal rather than vertical relapse at the B point. Changes in mandibular plane angle (SN/ML) during surgery affect vertical, but not horizontal relapse at the B point.
Keywords: Mandible, Orthognathic surgery, Osteotomy, Mandibular advancement
I. Introduction
Bilateral sagittal split osteotomy (BSSO), introduced by Trauner and Obwegeser in 1957, is currently the most favored and widely used surgical method for correction of lower jaw deformities
1. This technique usually results in considerably improved function and appearance. However, undesirable side effects are possible
2, of which skeletal instability (relapse) is one of the most commonly reported
3. This happens in almost every case, and it can be fairly significant for some patients
4.
Considerable changes in the lower jaw position and significant alteration in the forces transmitted to it have made stability of new jaw position an important goal for every surgeon, and it is paramount to success
5.
Relapse is divided into early and long-term based on the timing of occurrence. The main causes of early relapse are usually movements at the osteotomy site and condylar sag. These problems are mainly due to unbalanced soft tissue tension after surgery
5. This type of relapse occurs during the first 6-24 weeks after orthognathic surgery
6, which is considered the period when the majority of relapse occurs
7. Long-term relapse usually occurs because of progressive condylar coorresorption, which leads to loss of height of the condyle and mandibular ramus
58.
Postoperative skeletal relapse is attributed to either biological factors, such as further mandibular growth, or factors related to the surgical procedure and postoperative patient care
2. These factors include the magnitude and direction of skeletal movement, method of fixation, use of bone graft, condylar positioning
910, and achievement of postoperative occlusion
9. However, other factors such as the magnitude of mandibular movement10 and the mandibular plane angle the effects of which on relapse have yet to be elucidated
811. Other variables such as age and sex may affect the new mandibular position after surgery.
In this study, we sought to assess if any correlation exists between the magnitude of mandibular movement and relapse in BSSO and if changes of the mandibular plane angle affect stability following surgery.
II. Materials and Methods
This retrospective cohort study aimed to evaluate the postoperative stability of mandibular advancement in class II skeletal subjects who underwent BSSO at Chamran Medical Center in Shiraz University of Medical Sciences, from 2008 to 2012. The study was approved by the medical ethics committee at Shiraz University. Subjects eligible for inclusion had class II skeletal deformities that required mandibular advancement without maxillary osteotomy. Each subject was checked for adequate records, including date and type of surgery. All patients had completed growth prior to surgery. Subjects were excluded if they had a history of trauma, orthognathic surgery, any augmentation with alloplastic or autogenous materials during or after surgery, temporomandibular joint (TMJ) surgery before or after orthognathic surgery, temporomandibular disorder before surgery or asymmetric mandible.
Twenty-five subjects were assessed. All subjects were surgically treated by BSSO for mandibular advancement according to the Obwegeser/Dal Pont method. Rigid internal fixation was obtained with miniplates and four monocortical screws bilaterally.
By using lateral cephalograms taken on three occasions (preoperatively, immediately after surgery, and 1 year postoperatively) as a raw data base, skeletal points were determined and digitized to evaluate two-dimensional skeletal changes during and after surgery and to determine the amount of relapse. The same x-ray machine and settings were used for all cephalograms. Patients were stabilized in the ProMax cephalometric unit (Planmeca, Helsinki, Finland) using a cephalostat. This positions the patient with the head oriented at a 90° angle relative to the x-ray beam at a distance of 5 ft from the tube. The jaws were in maximum intercuspation, with the tip of the tongue behind the upper incisor teeth and the lips in repose. The receptor (CR; Konica Minolta Medical Imaging, Maitland, FL, USA) was placed 38.1 cm from the head (this is the standard under which all cephalometric radiographs are taken and ensures that radiographs taken at different time points are directly comparable).
Radiographic exposure was at 60-80 kVp and 10-15 mA (23-61 seconds) and was repeated for each case. The radiographs were processed in the laser readout processor of the mentioned CR system. A DICOM PACS system was used to save and transfer images.
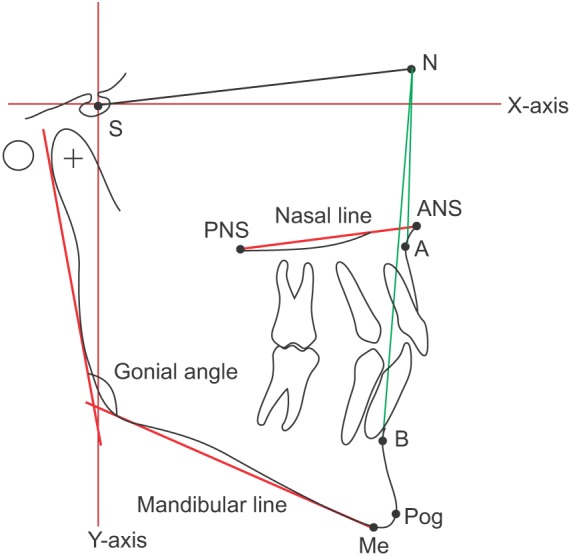
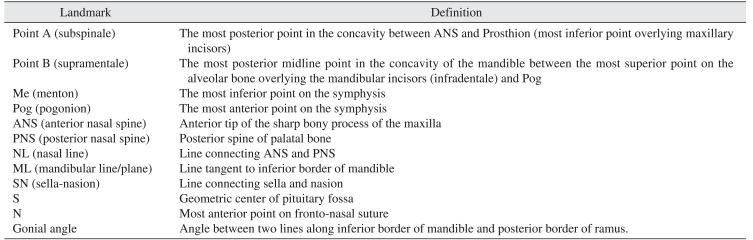
All lateral cephalograms were traced by hand, digitized, superimposed and evaluated by the same examiner. Tracings were then retraced and reanalyzed by another examiner. Cephalometric points included: Go (gonion), Pog (pogonion), Me (menton), point B, S (sella), and Na (nasion).(
Fig. 1,
Table 1)
Two angular parameters were determined using the points previously mentioned cephalometric reference. These angular parameters consisted of the gonial angle and SN/ML (mandibular line to sella turcica-nasion).
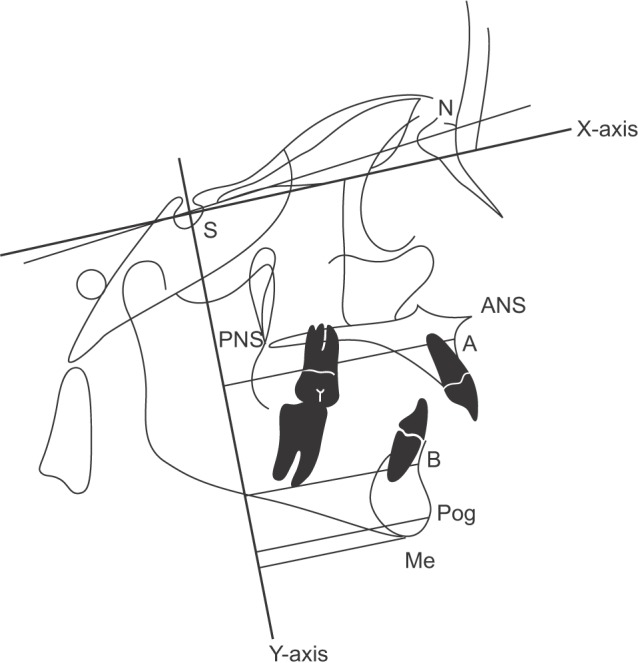
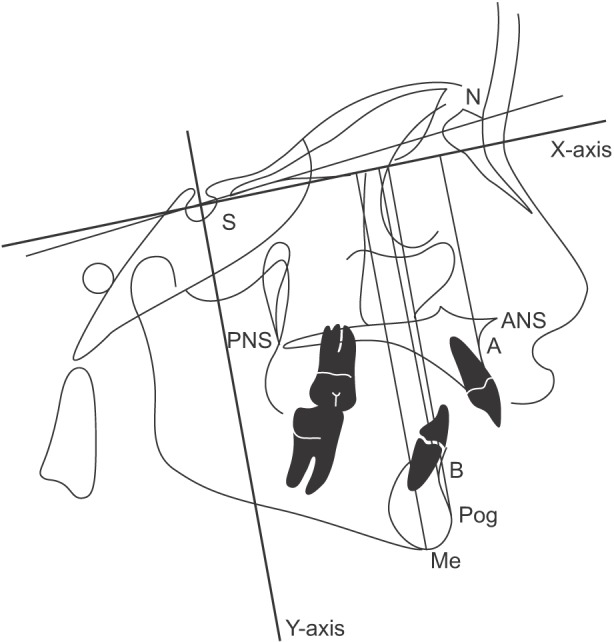
To determine horizontal and vertical relapse, an X-Y coordinate system was established. The X-axis was constructed by rotating S-N downward by 7° (an approximation of the Frankfort horizontal plane), and the Y-axis was defined as the line perpendicular to the X-axis and passing through the point sella. For certain reference points including point A, point B, pogonion, and menton, the perpendicular distance between each point and both axes was determined and the cephalometric variables were recorded as X- and Y-coordinates.(
Fig. 2,
3) All measurements were performed 1 year after the operation and conclusion of orthodontic treatments.
1. Tracing technique
All cephalograms were traced by a single operator on Garware matte acetate tracing paper of 0.003-inch thickness with a 3-H microlead pencil. Cephalometric landmarks were located, identified, and marked. The tracings were rechecked by another examiner.
2. Surgical technique
After induction of general anesthesia and nasotracheal intubation, lidocaine plus epinephrine 1:80,000 (persocaine-E; Darupakhsh, Tehran, Iran) was submucosally injected into the surgical site to control bleeding during the procedure. Bilateral mucosal incisions were made at the retromolar area to provide access to the bone. BSSOs were performed according to the abovementioned method using splitting forceps and elevators (curved Smith Sagittal Split Separators; Walter Lorentz Surgical, Biomet, FL, USA). After subperiosteal dissection, bone cuts were performed using a saw. The bone was cut laterally at the mesial area of the second molar, and a medial cut was created horizontally above the lingula approximately 1 cm above the occlusal plane. Two cuts were connected through the alveolar ridge. Splitting was performed with the elevator positioned in the vertical bone cut and the forceps in the sagittal bone cut. Once the superior part of the mandible began to split, the elevator was repositioned at the inferior end of the vertical cut, and the splitting was completed. After complete mobilization of the mandible and detachment of the medial pterygoid attachments on the proximal and distal segments, it was advanced into the desired position using a thin wafer. Intermaxillary wire fixation and elastics were not used postoperatively. In all subjects, condyles were positioned in the superior and posterior part of the glenoid fossa by manually guiding the proximal segment. Titanium miniplates (four holes) were used for fixation of the fragments.
3. Statistical analysis
Statistical analyses were performed using the IBM SPSS Statistics, version 19.0 (IBM Co., Armonk, NY, USA). Pearson correlation test was used to find correlations between age, amount of advancement, and study outcomes. A linear general model was applied to predict possible relapse. Independent t-test was used to determine the possible difference between genders. The receiver operating characteristic (ROC) test was used to identify a cut-off point in anatomical size. Inter-examiner reliability analysis was performed using the Kappa statistic to determine consistency between examiners.
III. Results
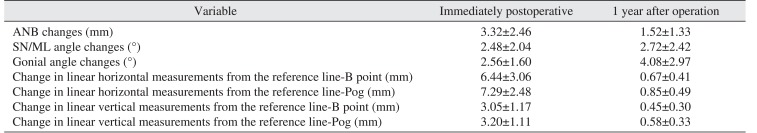
Twenty-five subjects (10 males, 15 females) were studied. The mean age was 23.64±4.41 years. Mean mandibular advancement was 6.44±3.06 mm at the B point. Mean relapse was 0.67±0.41 mm in the horizontal vector at the B point and 0.45±0.30 mm in the vertical vector. Mean relapse in the pogonion point was 0.85±0.49 mm in the horizontal and 0.58± 0.33 mm in the vertical vector.(
Table 2)
Data analysis by Pearson correlation test showed significant correlation between the amount of mandibular advancement and relapse in the B point (vertical and horizontal) and pogonion point (vertical and horizontal) (P<0.001). The results did not show any correlation between relapse in SN/ML and amount of mandibular advancement (P>0.05).
Mean SN/ML change after the surgeries was 4.40°±3.48°. Data evaluation demonstrated a positive correlation between the SN/ML change and vertical relapse in the B point and the mandibular plane (P<0.05). There was no correlation among SN/ML change, horizontal relapse in the B point, and relapse in the pogonion (vertical and horizontal) (P>0.05).
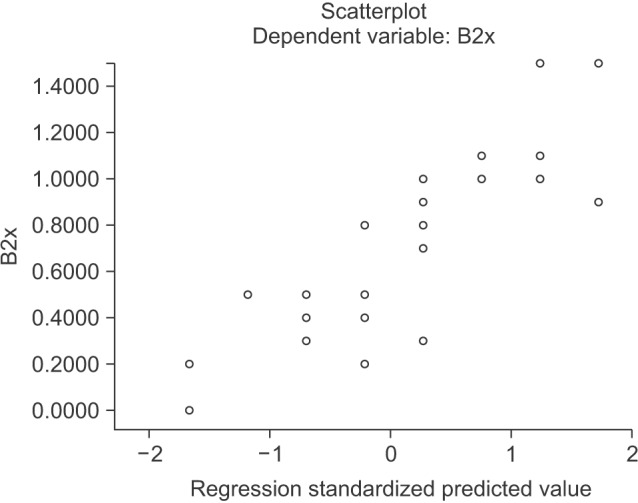
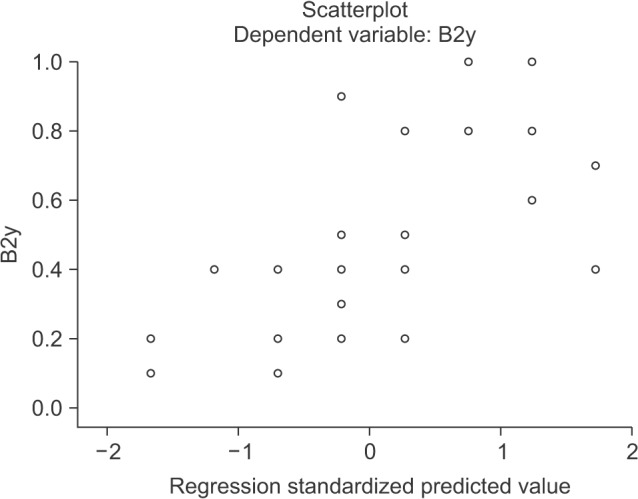
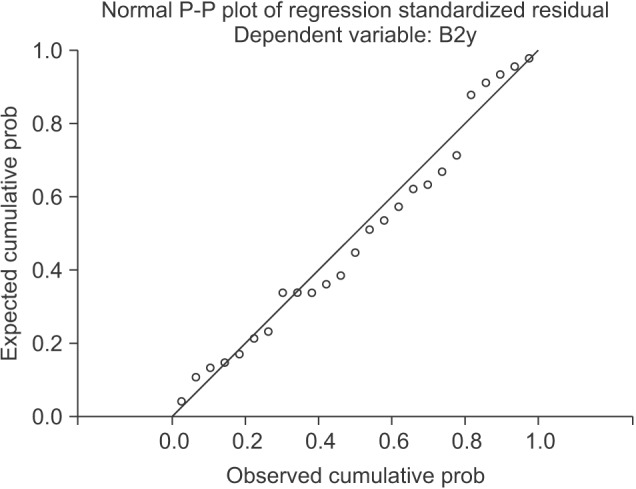
A simple regression model demonstrated that 74% of the horizontal relapse in B point was accounted for by the amount of mandibular advancement. The results showed that when the mandible was advanced 1 mm, horizontal relapse increased by 0.17 mm.(
Fig. 4) For one unit standard deviation (SD) increase in mandibular advancement, the horizontal relapse is expected to increase by 0.86 of a SD unit (R
2=0.74, β=0.86,
P=0.001). Data analysis showed that 42.3% of the vertical relapse in B point could be predicted by the amount of mandibular advancement. When the mandible was advanced 1 mm, vertical relapse increased by 0.09 mm.(
Fig. 5) For one unit SD increase in mandibular advancement, vertical relapse increased by 0.65 of a SD unit (R
2=0.42, β=0.65,
P=0.001).
The general linear model revealed that 24.2% of vertical relapse in the B point was accounted for by the amount of mandibular plane angle change. When mandibular plane angle increased by one degree, vertical relapse increased by 0.04 mm.(
Fig. 6) For one unit SD increase in mandibular plane angle, the vertical relapse is expected to increase by 0.49 of a SD unit (R
2=0.24, β=0.49,
P=0.001).
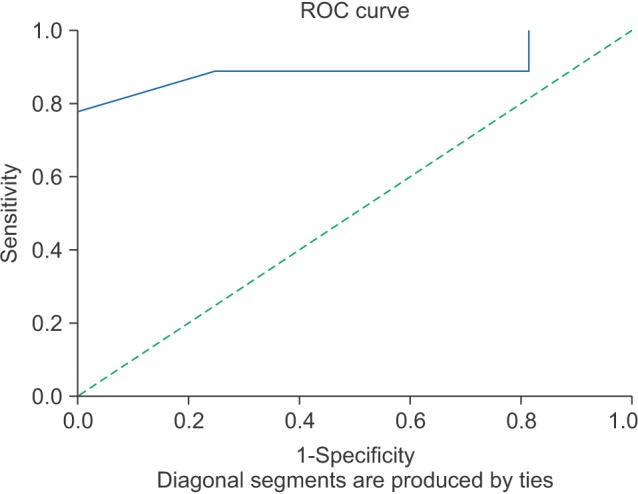
The ROC test showed that mandibular advancement by 8.5 mm had a relapse rate of 1 mm or more in the pogonion vertically and horizontally.(
Fig. 7)
The inter-examiner reliability for examiners was found to be Kappa=0.69 (P<0.001) with 95% confidence interval, demonstrating substantial agreement between examiners.
IV. Discussion
Relapse is a known short- and long-term complication of BSSO, and it has been studied extensively for more than three decades. It is a multifactorial phenomenon affected by many variables
4; the extent to which each factor contributes to total relapse is not yet known
12. The amount of mandibular movement along with other factors has been shown to play a role in the magnitude of relapse
51314.
We assessed the effect of the magnitude of mandibular advancement, change of mandibular plane angle during surgery, age and sex on postoperative stability.
Since a number of factors, including TMJ pathologies related to greater advancements, are involved in postoperative relapse, certain considerations should be taken into account for interpretation of results. To establish a reliable study, measurement error should be considered. Many variables and analytical errors were eliminated. All patients underwent only one orthognathic surgical procedure by the same surgical team at the same institution, and all cephalometric measurements were made by one operator. Because they all had the same type of osteotomy and were operated on under similar conditions allows general conclusions to be drawn. The B point and pogonion were selected as identifiable anterior references. These two points are the most widely used parameters to assess mandibular movements because of their stability and reliability
7.
Our results confirmed that significant correlation existed between the amount of advancement and vertical and horizontal relapse in both the B point and pogonion. The current study indicates that although the magnitude of mandibular advancement significantly affects degree of relapse in the B point and pogonion, it does not correlate with the degree of postoperative change in mandibular plane angle (SN/ML). The results showed that there was a positive correlation between the change in SN/ML during surgery and postoperative relapse of SN/ML. Changes in SN/ML affect vertical but not horizontal relapse at the B point. According to the results, the magnitude of mandibular advancement was a stronger surgical predictor for horizontal rather than vertical relapse at the B point. In addition, mandibular plane angle (SN/ML) changes during surgery affected the vertical relapse at the B point.
Previous studies have mostly found similar results in terms of short-term stability. Their findings indicated that magnitude of advancement was a major contributor to relapse
12151617. In addition to placing increasing amounts of stretch on the surrounding soft tissue, larger advancements have a smaller interface of bone at the osteotomy site. This may make them more susceptible to short-term relapse
13.
Eggensperger et al.
11 concluded that magnitude of relapse correlates to magnitude of surgical movements in 2004. In a later study
8 analyzing short- and long-term skeletal relapse, they found no significant relationship between the amount of initial surgical advancement and skeletal relapse. This result is probably because the amount of surgical movement in their study was lower than that in other investigations (4.1 at the B point and 4.9 at the pogonion)
8.
According to many studies, when advancement exceeds 6 or 7 mm measured at the B point and pogonion, the risk of horizontal relapse increased
1418.
In a study by Arpornmaeklong et al.
19, mandibular advancement greater than 10 mm was associated with a significant increase in the relapse rate.
Our results are consistent with the findings of other authors. Our study had an average mandibular advancement of 6.44±3.06 mm, and significant increase in relapse was observed when the magnitude of advancement exceeded 8.5 mm. However, some previous studies did not report the same results. Perrott et al.
6 reported an average of 6.34 mm mandibular advancement and found no correlation between the amount of mandibular advancement and relapse.
In another study with B point advancement of 4.4 mm (range 1-10 mm), no patient showed a clinically significant relapse
20.
A number of other investigations evaluated long-term relapse
1521. Van Sickels
15 noted considerable long-term relapse for advancements beyond 13 mm.
The effect of preoperative mandibular plane angle was not investigated in our survey. However, several studies have investigated the correlation between mandibular plane angle and horizontal and vertical relapse
14.
Different patterns of relapse were observed among high-angle and low-angle subjects. High-angle cases were associated with more horizontal relapse, whereas patients with a low mandibular plane angle had increased vertical relapse. Moreover, low-angle mandibular plane angle was associated with short-term relapse. In high-angle cases, the majority of relapses occurred late in the follow-up period
1422.
Eggensperger et al.
11 reported that cases with high mandibulo-nasal plane angle (hyper divergence) had 30% higher relapse rates. In another investigation of short- and long-term relapse, Eggensperger
8 concluded that preoperative high mandibulo-nasal plane (ML-NL) angle was correlated with long-term skeletal relapse. These findings were in accordance with other studies reporting more frequent relapse in BSSO patients with high mandibular plane angle
1923.
Mobarak et al.
22 reported that low-angle patients are at higher risk of short-term relapse due to early postoperative movement at the osteotomy site.
Alteration of mandibular plane angle during surgery is considered another surgical factor that affects postoperative relapse. Together with large mandibular advancement, it increases the relapse rate
24. However, few studies have evaluated the effects of differing mandibular plane angles on relapse rate.
Frey et al.
12 concluded that alteration of mandibular plane angle with counterclockwise rotation of mandibular plane angulation was associated with late vertical and horizontal relapse. The results of our study suggest a positive correlation between change in mandibular plane angle during surgery and postoperative relapse. Changes in mandibular plane angle during surgery affected vertical but not horizontal relapse at the B point.
The mandibular plane angle changes according to position of the proximal segment relative to the distal segment. If the proximal segment is rotated upwards and forwards, this alone decreases the mandibular plane angle regardless of it is a high-angle case or a low-angle case.
Age has been described as another significant factor in postoperative stability, with younger subjects showing a higher probability of late relapse
11. The reason we did not find a correlation between age and relapse in this study is likely because a longer follow-up period is necessary.
There are some limitations about this study. The aim of this investigation was to evaluate relapse for one year. A longer period of observation is necessary to assess the results of orthognathic surgery. Our study did not evaluate other possible contributing factors such as condylar change, and we did not have a comparison group. Stronger statements could have been made by considering contributing factors with a comparison group. Because the majority of relapses occur early during the first 6 months after surgery, movement at the osteotomy site or failure to properly seat the condyle are strongly implicated. However, condylar position was not studied here. Open bite and deep bite subjects were not designated or compared in terms of changes in mandibular plane angle during surgery and postoperative stability. Surgery stability depends on occlusion, but analysis of occlusion was not conducted in this study.
Other factors such as postoperative patient management, which may influence the outcome of surgery, were also not taken into account. The relatively small sample size in this study does not permit discussion of predictable patterns of mandibular movement. A larger sample size is required to draw general conclusions. The results of different studies are not fully comparable because there are differences in patient populations, cephalometric analyses, magnitudes of advancement, use of occlusal splints, fixation techniques and follow-up periods.
V. Conclusion
The following conclusions can be made on the basis of findings from a sample of 25 class II subjects characterized by mandibular retrognathism who received BSSO to correct the class II relationship:
1. Magnitude of mandibular advancement is a major contributor to relapse; it is a stronger surgical predictor for horizontal than vertical relapse at the B point.
2. With average mandibular advancement of 6.44±3.06 mm at the B point, significantly increased relapse was observed when the magnitude of advancement exceeded 8.5 mm.
3. Changes in mandibular plane angle during surgery affect early vertical but not horizontal relapse at the B point.
4. No significant relationship was found between sex and relapse.
5. There was no significant correlation between age and postoperative stability.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download