Abstract
Maxillofacial images must be examined to find pathologies not identified during clinical examination. Unicystic ameloblastoma (UA) extending to the mandibular body and ramus was neglected on initial panoramic radiographic examination. After orthodontic therapy, a huge lesion was observed clinically and through imaging exams. After the conservative surgery, no recurrence was observed during five years of follow-up. This case emphasized the need for careful evaluation of patient images focusing on the oral diagnosis before any dental treatment planning, including orthodontic therapy.
In spite of its benign nature, the ameloblastoma is a slowly growing, locally invasive, and epithelial odontogenic tumor1. Multicystic ameloblastoma is the most common variant and 5% to 15% of all ameloblastomas are of the unicystic type2. This lesion is a less clinically aggressive variant of ameloblastoma3. More than 90% of unicystic ameloblastoma (UA) involve the mandible, usually the posterior region; and up to 80% are associated with an unerupted mandibular third molar2. The mean age of UA occurrence is around 16 years, as opposed to 35 years, in the absence of an unerupted tooth without gender predilection12.
Radiographically, UA often has a unilocular radiolucency surrounding the crown of an unerupted tooth, although it may also appear as a well-defined intraosseous radiolucent area14. These findings resemble cysts in the jaws and, hence, the final diagnosis is only confirmed through histopathological analysis24. Therefore, UA tends to present as a well-defined unilocular lesion; nevertheless, a multilocular appearance is also reported45. In the early phase, UA may be routinely found in panoramic radiographs4. Nevertheless, computed tomography (CT) scans are highly recommended to determine details in relation to tumor extension and bone and teeth involvement6.
Here, we described a case of UA not found during orthodontic treatment planning. Although, some unilocular radiolucent lesions in the posterior mandible areas present sign and symptoms, others are completely asymptomatic and thorough imaging examination is necessary to avoid diagnosis negligence.
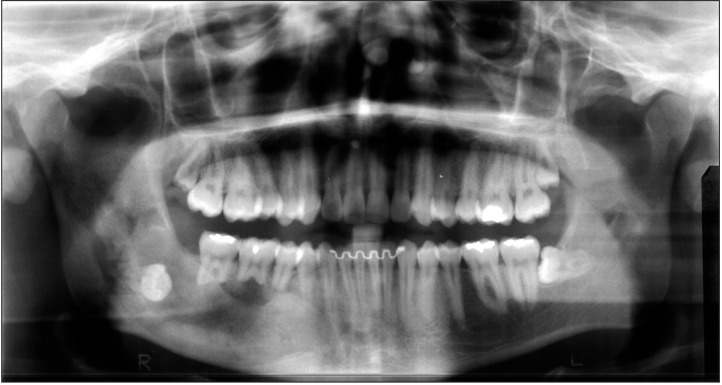
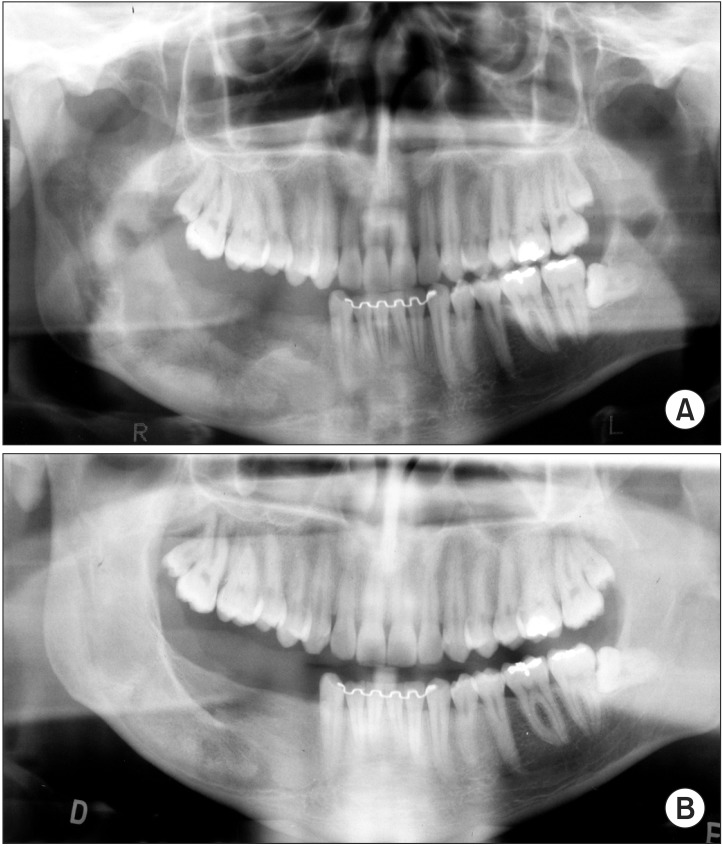
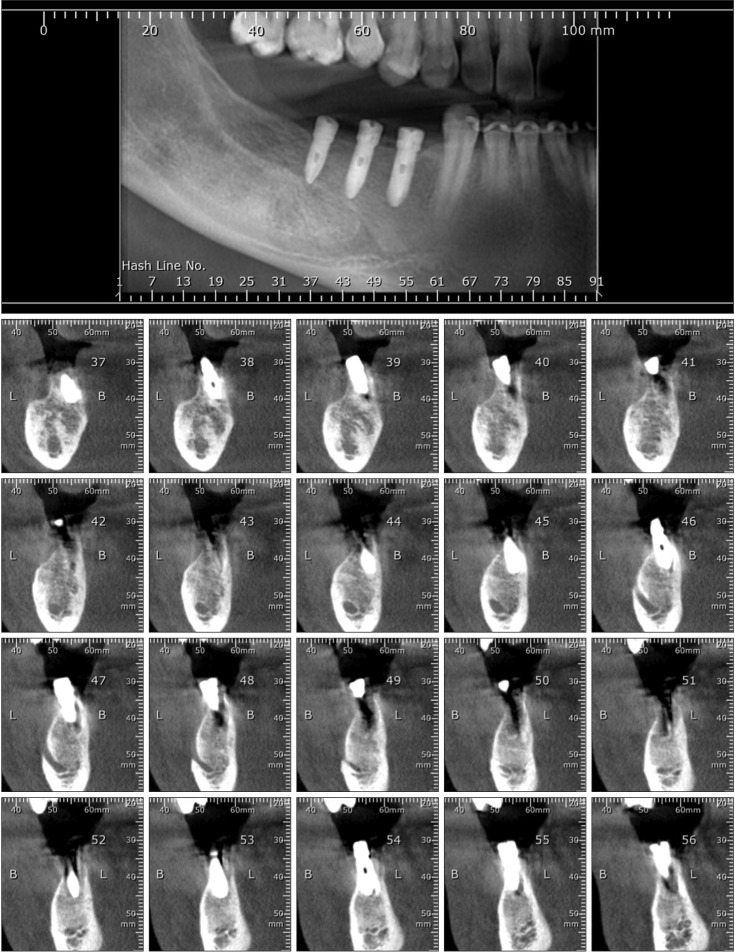
A 16-year-old Caucasian male patient was submitted to radiographic examination for orthodontic planning in 2004. (Fig. 1) On the panoramic radiograph, a circumscribed unilocular radiolucency lesion could be observed associated with an unerupted third molar. However, such alteration was neither pointed out in the radiological report, nor noted by the orthodontist and orthodontic braces were fixed. The medical history was non-contributory and extra and intraoral examination did not reveal any clinical findings. In 2008, the patient observed an edema in the right region of the mandible after he finished the orthodontic treatment and sought dental care. Firstly, periapical radiographs of the right lower premolars and molars were obtained. Radiographic examination showed a huge unilocular radiolucent image surrounding the roots of the erupted posterior teeth. A panoramic radiograph was obtained and a marked expansion of the right mandibular posterior region was seen. A remarkable tooth resorption and extension from the right mandible ramus to the anterior region limit were also observed.(Fig. 2) Additionally, axial and coronal multislice CT scans with a bone window were acquired to delimit the lesion tridimensionally, as well as to register its effects on the adjacent cortical bone plates such as spreading, erosion, and thinning. A hypodense area causing expansion and thinning of the buccal and lingual cortical plates, in the right mandibular body, angle, and ramus was seen in CT scans. The mandibular right third molar was displaced to the base of the mandible.(Fig. 3)
An incisional biopsy was performed and histopathological analysis revealed a cystic aspect with islands of odontogenic epithelium resembling stellate reticulum within a fibrous stroma. This cyst-like lesion was similar to ameloblastoma. Due to the large lesion dimensions, a drain was placed from the retromolar area to the mandibular body for decompression. On the panoramic radiograph, acquired after one year and four months of using drains, a radiopaque area was seen in the region corresponding to the lesion, indicating bone neoformation.(Fig. 4)
The lesion was enucleated and five teeth were extracted (all the mandibular right premolars and molars) followed osteotomy of the margins. After the surgery, the histopathological examination revealed a cystic lesion partially lined by ameloblastomatous epithelium, evidencing peripheral palisading, hyperchromatic nuclei, and reversed nuclear polarization. Suprabasal cells were loosely arranged resembling stellate reticulum. The fibrous cystic wall was infiltrated by ameloblastomatous epithelium. Based on these features, a UA of the mural type was diagnosed. Serial sections were performed to rule out a diagnosis of conventional solid ameloblastoma.
The patient was continuously followed-up with clinical and radiographic examinations and no signs of lesion recurrence were seen five years after complete surgical excision. Conversely, a radiopaque area was observed on the corresponding region, i.e., mandibular right body, angle, and ramus. (Fig. 5) Rehabilitation with osseous integrated implants was planned to occur after five years of following-up. Cone-beam CT images showing the complete bone formation and the mandibular dental implants are presented in Fig. 6.
Ameloblastomas have a well-documented tendency to spread by infiltration through the medullary spaces in deep extension causing facial mutilation if early detection is not properly accomplished1. Although this behavior is more common in the multicystic pattern, some unicystic lesions can present a similar biological profile13. In this case report, lesion diagnosis was firstly neglected; however, imaging exams should have been a substantial tool in the assessment and treatment planning7. Panoramic radiographs, even displaying a two-dimensional aspect of such lesions, are useful to estimate invasion and other signs, such as root resorption, at the expense of a relatively lower radiation dose46. However, CT scans are mandatory for tridimensionally delimiting the lesion area and assessing the relationships with skull structures accurately67. In the present case, the UA was an asymptomatic and slowly growing tumor, corroborating the literature1234. Facial asymmetry was the clinical late sign and the main reason the patient sought dental care1234. In fact, the severe root resorption along with the marked occurrence of the lesion in the posterior region of the mandible was an important image feature for the establishing proper diagnosis13.
In this case, the choice of treatment modality mainly took into account the patient's age and lesion size89. A conservative decompression was followed by surgical excision to avoid radical mutilation891011. However, long-term follow-up with an average interval of seven years after the initial treatment is highly recommend, since late recurrences have been noted8910. Cone-beam CT scans acquired at five years of follow-up did not show signs of recurrence. This tridimensional modality yields high resolution images of the facial bones and teeth with lower radiation dose and cost, compared with multislice CT12.
It has been noted that neglecting a thorough assessment of an initial panoramic radiograph for orthodontic purposes was related to late diagnosis of important pathologies and bone damage. Furthermore, orthodontic therapy failures are more than an inconvenient consequence, since an evident destructive lesion was overlooked. Irrespective of their diagnostic goal, dentists must unequivocally analyze all the features from an area in a detailed and systematic manner, thus assuming the legal responsibility for a complete, accurate diagnosis.
References
1. Masthan KM, Anitha N, Krupaa J, Manikkam S. Ameloblastoma. J Pharm Bioallied Sci. 2015; 7(Suppl 1):S167–S170. PMID: 26015700.
2. Barnes L, Eveson JW, Reichart P, Sidransky D. Pathology and genetics of head and neck tumours. 3rd ed. Lyon: IARC Press;2005.
3. Philipsen HP, Reichart PA. Unicystic ameloblastoma. A review of 193 cases from the literature. Oral Oncol. 1998; 34:317–325. PMID: 9861335.

4. Volpi L, Ferreli F, Karligkiotis A, Pistochini A, Meloni F, Castelnuovo P. Radiology quiz case 1. Diagnosis: unicystic ameloblastoma (UA). Arch Otolaryngol Head Neck Surg. 2012; 138:973–974. PMID: 23069829.
5. Bajpai M, Agarwal D, Bhalla A, Kumar M, Garg R, Kumar M. Multilocular unicystic ameloblastoma of mandible. Case Rep Dent. 2013; DOI: 10.1155/2013/835892.

6. Crusoé-Rebello I, Oliveira C, Campos PS, Azevedo RA, dos Santos JN. Assessment of computerized tomography density patterns of ameloblastomas and keratocystic odontogenic tumors. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:604–608. PMID: 19464213.

7. De Melo WM, Pereira-Santos D, Sonoda CK, Pereira-Freitas SA, de Moura WL, de Paulo Cravinhos JC. Large unicystic ameloblastoma of the mandible: management guided by biological behavior. J Craniofac Surg. 2012; 23:e499–e502. PMID: 22976721.
8. Dolanmaz D, Etoz OA, Pampu A, Kalayci A, Gunhan O. Marsupialization of unicystic ameloblastoma: a conservative approach for aggressive odontogenic tumors. Indian J Dent Res. 2011; 22:709–712. PMID: 22406718.

9. de Paulo LF, Oliveira MT, Rodrigues ÁR, Zanetta-Barbosa D. Treatment of an extensive unicystic ameloblastoma in a 7-year-old child: the best approach? Br J Oral Maxillofac Surg. 2015; 53:292–294. PMID: 25542283.

10. Ramesh RS, Manjunath S, Ustad TH, Pais S, Shivakumar K. Unicystic ameloblastoma of the mandible--an unusual case report and review of literature. Head Neck Oncol. 2010; 2:1. PMID: 20157425.

11. Park HS, Song IS, Seo BM, Lee JH, Kim MJ. The effectiveness of decompression for patients with dentigerous cysts, keratocystic odontogenic tumors, and unicystic ameloblastoma. J Korean Assoc Oral Maxillofac Surg. 2014; 40:260–265. PMID: 25551089.

12. Luo J, You M, Wen C, Xu L, Zheng G. Cone-beam CT features of ameloblastomas. Hua Xi Kou Qiang Yi Xue Za Zhi. 2014; 32:373–377. PMID: 25241540.
Fig. 1
First panoramic radiograph acquired for orthodontic planning showed a unilocular radiolucent image associated with the mandibular right third molar.

Fig. 2
Panoramic radiograph after the orthodontic treatment showing a well-defined extensive unilocular lesion with the involvement of the mandibular third molar.

Fig. 3
Axial and coronal computed tomography scans highlighting lesion expansion. Note the lingual and buccal cortical plate expansion and thinning.

Fig. 4
Panoramic radiograph showing the decompressed lesion area with a radiopaque filling, suggesting bone neoformation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download