Abstract
Objectives
Submental intubation has been advocated as an alternative to classical tracheostomy for certain indicated panfacial trauma surgeries. Surgeons should have various options for airway management in maxillofacial trauma patients. Most maxillofacial injuries involve occlusal derangements, which might require intraoperative occlusal corrections; hence, orotracheal intubation is not ideal. Maxillofacial surgeons generally prefer nasotracheal intubation; however, in cases with concomitant skull base fracture or nasal bone fracture, nasotracheal intubation might not be suitable; in these situations, tracheostomy is typically performed. However, the possible complications of tracheostomy are well known. Due to trauma situations and to avoid the complications of tracheostomy, submental intubation would be an ideal alternative procedure in selected maxillofacial trauma surgery patients. This study aimed to evaluate the safety and usefulness of a submental intubation technique for panfacial trauma surgery. Moreover, we intended to share our experience of submental intubation and to recommend this simple, safe procedure for certain panfacial trauma surgeries.
Materials and Methods
In five panfacial trauma patients, we performed submental intubation for airway management; the mean time required for the procedure was only eight minutes.
Orotracheal and nasotracheal intubations are the preferred procedures for airway maintenance in maxillofacial trauma patients. Nasotracheal intubation is an ideal approach to airway management in some maxillofacial trauma surgeries. Panfacial trauma, which involves occlusion or nasoethmoidal complex fracture with or without skull base fractures, needs to be attended to simultaneously. However, when there is a nasal bone fracture, nasotracheal intubation might not be ideal. Orotracheal intubation is also not suitable when surgeons must determine or correct the occlusion intraoperatively. In the above situations that might require intraoperative change from a nasotracheal tube to an orotracheal one, this act can invite anesthetic complications. Though classical tracheostomy could overcome these problems, it also has significant complications. In 1986, Hernández Altemir1 proposed submental intubation as a simple method of airway maintenance that facilitates the simultaneous treatment of all maxillofacial fractures without any interference to the tube during the operation. This procedure permits intraoperative occlusal corrections and also allows the surgery to address any associated nasoethmoid fractures. Submental intubation is one of the safest and simplest procedures, unlike tracheostomy, that requires technical expertise. Submental intubation can be performed by maxillofacial surgeons with a minimal basic armamentarium. It can also be executed within a short time with minimal complications and is the most cost-effective technique for complex maxillofacial injury patients2. Here, we present our experience of submental intubation in five cases of panfacial trauma with fractures of the mandible, maxilla, or zygomatic bone with occlusal derangement, requiring intraoperative occlusal adjustments and corrections, and also with nasal bone fracture that needed to be addressed simultaneously. Patients who were anticipated to be difficult intubations and those with problems opening their mouths were not included in our study.
Our aim is to evaluate the safety and usefulness of a submental intubation technique for panfacial trauma surgery, to present our experience, and to advocate this technique as an ideal alternate procedure to classic tracheostomy for certain indicated panfacial trauma patients.
All patients with a history of road traffic accident were referred to our Department of Dentistry at ESIC Medical College and Postgraduates Institute of Medical Sciences and Research (PGIMSR) (Chennai, India) from the regular outpatient department. After a thorough history was taken and clinical and radiographic examinations were performed, patients with more than one bone fracture were classified as having panfacial trauma. Patients with occlusal derangement and nasal bone fracture were scheduled for open reduction and internal fixation under general anesthesia using submental intubation. An anesthetist's opinion was obtained regarding the patients' fitness for surgery. The patients provided informed consent for submental intubation and also for surgery. Pre-anesthetic preparations were carried out. A flexometallic endotracheal tube with a detachable universal connector was used. The necessary airway with adjuncts, crash cart, intubation aids were readied prior to induction. The tube and connectors were disconnected and verified in order to help us easily remove them when changing the tube from intra-oral to extra-oral through the submental route. Initially, regular orotracheal intubation was achieved using a conventional laryngoscopy technique. Both extra-oral and intra-oral preparations were carried out. The landmarks for the skin incisions were placed below the commissure of the mouth and directly below the lower border of the mandible at the para-median region. Local anesthetic (2 mL of 2% lignocaine with adrenalin 1:200,000) infiltration was administered. A 2-cm para-median incision (Fig. 1) was made as described by Altemir1. Blunt dissection was carried out through the subcutaneous tissue, platysma with heavy artery forceps, and passed through the mylohyoid muscles.(Fig. 2) While traversing these muscles, the forceps should always be in contact with the lingual surface of the mandible. One finger was kept inside the oral cavity to feel the tip of the artery forceps. When the forceps reached the mucosa, we could feel the tip of the artery forceps and noticed blanching of the mucosa in the floor of the mouth. The tip of the artery forceps was positioned away from the sublingual duct and its opening. An incision was made on the tip. While performing this incision over the mucosa, caution was taken not to injure the submandibular duct and its orifice or the lingual nerve. The tip of the forceps was opened widely to create a tunnel through which the tube would be passed from the intra-oral to the extraoral side. Here, we modified Altair's technique by passing an additional smaller artery forceps along with the main artery forceps. The patients were ventilated with 100% oxygen for two minutes before disconnecting the endotracheal tube from the connector. The endotracheal tube was immediately and carefully disconnected from the connector, and the pilot balloon was deflated by the anesthetist and then removed to the extra-oral side using a small artery forceps.(Fig. 3) Next, the proximal end of the tube was removed through the tunnel using a pair of stout artery forceps. With this technique, the duration of apnea was minimized to <20 seconds. Blood or secretions in the pilot balloon were cleaned, and the tube was reconnected with the connector and with the circuit and properly secured with skin sutures.(Fig. 4) The anesthetist verified the position of the tube and ventilation. Separate kits were used for submental intubation and for the main surgical procedure. At this time, the surgeons scrubbed in again and prepared for the main surgery, which was performed without disturbing the tube. All maxillofacial fracture sites were exposed, reduced, and fixed after achieving occlusion. Nasal bone fractures were also reduced using closed reduction. The maximum duration for the submental procedure was around 8 to 10 minutes. The armamentarium for submental intubation included two artery forceps, a No. 15 surgical blade and handle, retractors, and a suturing kit. The duration of the trauma surgeries was roughly 3 to 5 hours; the mean duration of surgery was 4 hours and 10 minutes. After the surgery, all patients were extubated by the anesthetist. During extubation, the proximal end of the tube was reintroduced into the oral cavity and extubated through the mouth in two patients. For the other three patients, the tube was extubated directly through the submental route. The skin wound was sutured with 3-0 Ethilon (Ethicon, Somerville, NJ, USA). All patients recovered uneventfully.
Patients were reviewed on the first, second, and third postoperative days and after one week. No postoperative complications like infection or scar were noticed. Skin wound healing was aesthetically acceptable.(Fig. 5)
Patients were reviewed on the first, second, and third postoperative days and after one week. No postoperative complications like infection or scar were noticed. Skin wound healing was aesthetically acceptable.
In maxillofacial trauma surgery, surgeons have to seek different methods of intubation when surgical access is needed in both the nasal and oral cavities. Nasotracheal and orotracheal intubations are the most frequently used techniques for many maxillofacial trauma surgeries. Maxillofacial trauma patients generally have occlusal derangements, associated nasal bone fractures, and base of the skull bone fractures. When occlusal derangement is present, it might require intraoperative occlusal adjustment. Nasotracheal intubation is the preferred technique by maxillofacial surgeons over orotracheal intubation. Patients with associated nasoethmoid complex fractures might require surgical intervention, such as reduction and fixation, when nasotracheal intubation is contraindicated or poses a significant problem3. An alternative technique to managing these types of situations is classical tracheostomy, which also has iatrogenic complications, such as internal emphysema, tracheal stenosis, damage to the laryngeal nerves, tracheoesophagal fistula, and scarring45. Hernández Altemir1 proposed submental intubation as an alternative method to classic tracheostomy because it facilitates simultaneous access for all maxillofacial fractures without intraoperative interference to the tube. MacInnis and Baig6 and Agrawal and Kang7 advocated for midline intubation as a modification of this technique. In contrast, Rungta8 suggested the technique of retromolar submental intubation for maxillofacial trauma patients. Franco et al.9 reported that submental intubation is an alternative to tracheostomy when nasoendotracheal intubation is unsuccessful. There are certain indications for submental intubation; 1) the presence of cerebrospinal fluid, rhinorrhea, epistaxis, or nasal bone fracture where nasal intubation is contraindicated, 2) panfacial trauma that requires intraoperative occlusal adjustment along with nasoethmoid fracture reduction and fixation, 3) basal bone fracture along with any of the above fractures, 4) craniomaxillary surgery/orthognathic surgery patient with nasal pathology, 5) orthognathic surgery+rhinoplasty/nasal bone corrective surgery, and 6) patient with neurological deficit. In addition, some contraindications are also present; 1) trauma patient who might require a long period of assisted ventilation, 2) poly trauma with severe neurological deficits, 3) major thoracic trauma, which might require multiple repeated surgeries, 4) patient with multiple fractures of the mandible or injury to the floor of the mouth, and 5) patient who might require ventilator support during the postoperative period.
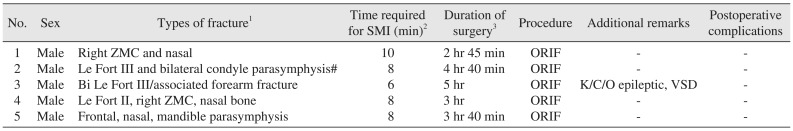
All our patients had panfacial trauma (Fig. 6; patients computed tomography) with the involvement and combination of at least any two of the mandible, maxilla, nasal bone, zygomatic maxillary complex, or frontal bone involving occlusion. For all cases of fractures that were reduced by open reduction, intraoperative occlusal correction was carried out, and internal fixation was performed by miniplate osteosynthesis. Nasal bone fracture was reduced, intranasal packing was placed, and external plaster of Paris splinting was applied. All patients were indicated for submental intubation. (Table 1) Oral intubation was initially established, and then patients were changed to submental intubation as described earlier. We required an average of 8 minutes (8-10 minutes) to perform the procedure; the duration of the surgery was 3 to 5 hours (mean, 4 hours and 10 minutes). Postoperatively, the patients were followed-up on the first, third, and seventh days, after two weeks, and after one month. Wound healing was satisfactory and resulted in minimal scarring. All patients were male. Skin incisions were made in a low-visibility area where a small scar might be more cosmetically acceptable than a regular tracheostomy scar. The intra-oral wound also healed well without any infection. Since this procedure allows for the simultaneous manipulation of nasal and facial fractures, we were able to avoid the complications of tracheostomy. No special equipment was required to execute this procedure, and it was technically very simple. Any oral surgeon could easily and safely perform this technique without expecting the same major complications that are currently associated with tracheostomy.
Reported complications of this approach include damage to adjacent structures, such as sublingual and submandibular ducts, sublingual gland, and lingual nerve8. Meyer et al.10 reported an 8% occurrence of oral floor abscesses and a 4% incidence of hypertrophic scar formation. However, the sample size in their study was rather small (n=25). Risk of postoperative salivary fistula has been reported in the literature in cases of prolonged ventilation. MacInnis and Baig6 detailed a patient who remained intubated in the intensive care unit for three days and experienced no complications. The risk of sepsis in the submental tunnel could be related to a contaminated endotracheal tube during extubation. We did not encounter any such complications in our patients. The endotracheal tube is routinely reintroduced intra-orally, which helps the surgeon with suturing the skin wound while the patient is still under anesthesia and the anesthetist with extubation. Two patients were extubated using the above method. The other three patients also had parasymphysis fractures, and open reduction and internal fixation was performed. There was a risk of infection through the submental tunnel due to the possibility of a contaminated endotracheal tube using the above method. To avoid such complications, the tube was extubated directly without reintroducing it intra-orally. The skin incision was sutured under local anesthesia while the patient was conscious. In the postoperative review, all patients were examined for submandibular and sublingual salivary gland function by measuring the salivary flow intra-orally or identifying salivary fistula, swelling, obstruction, or infection of the salivary glands. Lingual nerve function was also assessed using both an objective method (tongue pin prick test) and a subjective method by asking the patients whether they had any altered sensation of the tongue or loss of taste sensations on the side of the operation. All patients had normal salivary flow, and they all reported normal tongue sensation.
However, the sample size in our study was small (n=5). Our institution regularly treats maxillofacial trauma patients. Future longitudinal studies should include a larger number of samples.
Submental intubation is a simple, safe, and ideal procedure to maintain the airway during maxillofacial trauma surgery, particularly in patients with panfacial fracture who require occlusal correction and simultaneous management of all fractures. Maxillofacial surgeons who deal with panfacial trauma surgery should consider this procedure before opting for tracheostomy.
References
1. Hernández Altemir F. The submental route for endotracheal intubation: a new technique. J Maxillofac Surg. 1986; 14:64–65. PMID: 3456416.
2. Kar C, Mukherjee S. Submental intubation: an alternative and costeffective technique for complex maxillofacial surgeries. J Maxillofac Oral Surg. 2010; 9:266–269. PMID: 22190802.

3. Navaneetham A, Vinod Thangaswamy S, Rao N. Submental intubation: our experience. J Maxillofac Oral Surg. 2010; 9:64–67. PMID: 23139571.

4. Taicher S, Givol N, Peleg M, Ardekian L. Changing indications for tracheostomy in maxillofacial trauma. J Oral Maxillofac Surg. 1996; 54:292–295. PMID: 8600235.

5. Amin M, Dill-Russel P, Manisali M, Lee R, Sinton I. Facial fractures and submental tracheal intubation. Anaesthesia. 2002; 57:1195–1199. PMID: 12479188.

6. MacInnis E, Baig M. A modified submental approach for oral endotracheal intubation. Int J Oral Maxillofac Surg. 1999; 28:344–346. PMID: 10535533.

7. Agrawal M, Kang LS. Midline submental orotracheal intubation in maxillofacial injuries: a substitute to tracheostomy where postoperative mechanical ventilation is not required. J Anaesthesiol Clin Pharmacol. 2010; 26:498–502. PMID: 21547178.
8. Rungta N. Technique of retromolar and submental intubation in facio-maxillary trauma patients. Indian J Trauma Anaesth Crit Care. 2007; 8:573–575.
9. Franco J, Coppage J, Fallucco M, Ferguson JS. Submental intubation: an alternative to tracheostomy when nasoendotracheal intubation is unsuccessful--a case report. Can J Plast Surg. 2009; 17:e37–e38. PMID: 21119832.

10. Meyer C, Valfrey J, Kjartansdottir T, Wilk A, Barrière P. Indication for and technical refinements of submental intubation in oral and maxillofacial surgery. J Craniomaxillofac Surg. 2003; 31:383–388. PMID: 14637068.

Fig. 6
A, B, D-F. Three-dimensional reconstructed computed tomography (CT) of all patients. C. CT image shows fracture of bilateral parasymphysis (mandible; arrows).
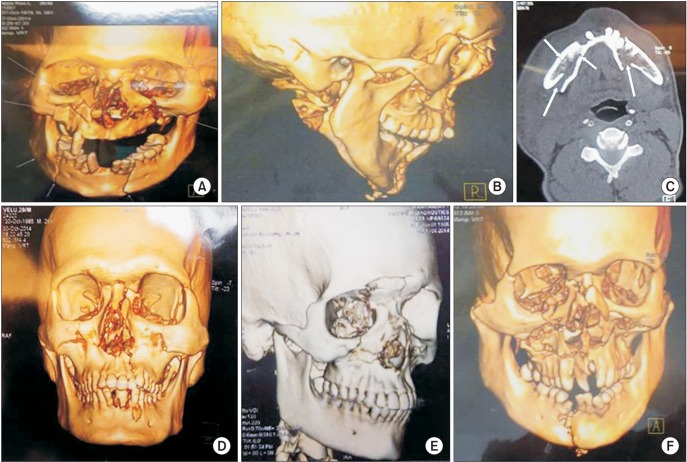
Table 1
Patient's details about the types of fracture




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download