Abstract
Calcifying cystic odontogenic tumor (CCOT) is an uncommon benign cystic neoplasm of the jaw that develops from the odontogenic epithelium. Invasion into the maxillary sinus by a CCOT is not a typical, and the recurrence of the cystic variant of CCOT in the posterior maxilla is rare. This report describes a recurrent CCOT occupying most of the maxillary sinus of a 24-year-old male patient. As a treatment, marsupialization was carried out as a means of decompression, and the involved teeth were all endodontically treated. Afterward, surgical enucleation was performed. The size of the lesion continued to shrink after marsupialization, and the maxillary sinus restored its volume. This patient has been followed-up for 3 years after the surgery, and there have not been any signs of recurrence.
Calcifying odontogenic cyst, also known as Gorlin cyst, is an uncommon developmental lesion that originates from the odontogenic epithelium1. After Gorlin et al.'s first description of such a lesion in 1962, it has become clear that two basic entities may be present: a cystic tumor and a solid neoplasm2. This benign cystic neoplasm is microscopically characterized by a well-defined basal layer in the epithelial lining. An overlying layer consists of stellate reticulum-like cells, and masses of ghost cells are present within the epithelial lining or fibrous capsule. Moreover, dystrophic calcification forms a dentinoid tissue in the fibrous capsule34. In 2005, the World Health Organization Classification of Head and Neck Tumors considered this lesion an odontogenic tumor rather than a cystic lesion and thus named it calcifying cystic odontogenic tumor (CCOT)5.
CCOT is an uncommon lesion that represents only about 1% of jaw cysts, occurring mostly within the bone. Both intraosseous and extraosseous forms of the lesion are found in the maxilla and mandible with approximately the same probability6, and these lesions mostly affect the incisor and canine areas. This lesion can also involve the posterior maxilla, but only few such cases have been reported78.
CCOT is mostly asymptomatic; therefore, it is frequently discovered during a routine radiographic examination3. Radiographically, CCOT typically presents as an unilocular or multilocular distinct radiolucent area that may include various radiopaque irregular calcified bodies. The lesion may be related with an odontoma or an unerupted tooth—nearly onethird of the cases involve impacted teeth9. In addition, the adjacent teeth frequently appear with resorptive or divergently displaced roots7.
The treatment plan for CCOT depends on the location and histological type of the lesion. A conservative treatment modality such as simple enucleation and curettage is mostly chosen for the cystic variants with good prognosis. In contrast, complete excision is recommended for the neoplastic variant, and recurrence is frequent10.
CCOT in the maxilla involving the maxillary sinus is relatively rare, and very few cases have been published. Furthermore, only one case of recurrent CCOT invading into the maxillary sinus was reported in the English literature11. Therefore, the present case regarding a cystic variant of CCOT in the posterior maxilla that recurred twice is uncommon. This report aimed to represent this recurrent cystic tumor occupying most of the maxillary sinus and that was successfully managed by conservative treatment.
A 24-year-old male patient was referred to our department by an otolaryngologist due to an expansive lesion of the left maxillary region. The clinical exam revealed that an asymptomatic swelling had increased in size in the area of the upper left premolars and molars. The patient had undergone functional endoscopic sinus surgery (FESS) twice based on a presumptive diagnosis of a cystic lesion in the maxillary sinus at the Department of Otorhinolaryngology. The final diagnosis according to the microscopic examination was CCOT.
Two years after the first FESS procedure, the patient revisited the hospital with a complaint of nasal obstruction and cheek tenderness in the same region.(Fig. 1) An additional FESS procedure for cyst marsupialization and granulation tissue removal was performed at the same department. However, the patient revisited the hospital 3 years later with recurred symptoms, and an extended lesion was seen on computed tomography (CT).(Fig. 2. B)
Extraoral examination showed facial asymmetry due to a non-tender left maxillary swelling. Intraoral examination revealed a firm swelling, covered by mucosa of normal appearance, which was localized on the buccal aspect of the premolar to the first molar region. There was no dental treatment history of left maxillary teeth. A panoramic radiograph revealed a large radiolucent lesion in the left maxillary sinus extending from #23 to #27, and the cystic lesion had resorbed the roots of teeth #23 to #27.(Fig. 2. A) CT scans showed a well-defined expansive lesion with thin cortical margins and irregular radiopaque masses. The size of the lesion was uncommonly large and occupied nearly the entire left maxillary sinus and extended to the orbital floor.(Fig. 2. B)
Cystic marsupialization and placement of an acrylic tube for maintaining a patency and drainage were carried out under local anesthesia.(Fig. 3. A) The patient was educated to irrigate the area with normal saline solution two times a week. Endodontic treatments were also performed in the involved teeth #23 to #27 that showed root resorption. Five months after the initial intervention, considerable regression of the lesion and new bone formation around the root areas of teeth #23 to #27 were noted. Radiographic examination showed that the bony border between the lesion and maxillary sinus became more apparent; the haziness in the area of the maxillary sinus not involved with the lesion appeared to be clearer, as new bone was deposited into the lesional border.(Fig. 3. B, 3. C)
At this time, surgical removal of the tumor was planned. Under general anesthesia, the lesion was simply enucleated through a transoral approach.(Fig. 4) As mentioned, since five months of marsupialization caused a thickened wall of the maxillary sinus, which was also the border between the lesion and the maxillary sinus, the sinus was intact during the surgery. Furthermore, no remarkable complication during or after the operation was noted.
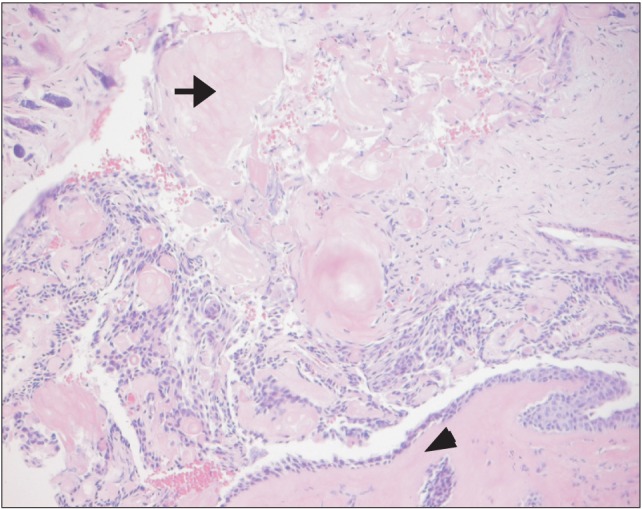
Histopathological examination concluded fibrous connective tissue with an epithelial lining; mineralization of ghost cells and dentinoid materials were identified. Cuboidal and cylindrical cells were found in the basal layer, and the epithelial cells were loosely arranged with groups of ghost cells. The definitive diagnosis was CCOT, the same as the previous biopsy result.(Fig. 5)
The patient was scheduled for regular follow-up. At recall, 36 months after the surgery, he did not show any signs of recurrence.(Fig. 6. B)
Odontogenic epithelial remnants are considered an origin of CCOT; because they are trapped within the bone or gingival tissue, CCOTs can be either intraosseous or extraosseous. In about 86% to 98% of cases, the lesions appear as a cyst-like structure, whereas 2% to 16% of cases show the solid or neoplastic form3. Since most CCOTs have no symptoms, they are usually found incidentally on radiographic results, and the lesions are often located in periapical or lateral periodontal areas of adjacent teeth12. Differential diagnosis of CCOT involves dentigerous cyst, adenomatoid odontogenic tumor, ameloblastic fibro-odontoma, and calcifying epithelial odontogenic tumor. The presence of radiopaque bodies is a meaningful finding. When calcified material is found on radiographic examination, the possibility of adenomatoid odontogenic tumor, calcifying epithelial odontogenic tumor, ossifying fibroma, and odontoma should be considered1314. In addition, it is important to recognize that, when CCOT is related with apices of the teeth, there is a high incidence of root resorption11. In cases of lesion associated with the apices of the teeth, root resorption has been found in 75% to 77% of the cases15. This rate of root resorption by CCOT is high compared with that by ameloblastoma in the cases reported by Struthers and Shear16. Therefore, root resorption, which was also found in the present case, can be considered one of the common features when the lesion is associated with adjacent teeth.
Treatment of CCOTs can be determined according to the site and the histological type of the lesion. Ledesma-Montes et al.17 studied 122 cases of CCOT and identified the following 4 histological variants: simple cystic CCOT (type 1), odontoma-associated CCOT (type 2), ameloblatomatous proliferating CCOT (type 3), and CCOT related with benign odontogenic tumors other than odontoma (type 4). In this case, the microscopic findings corresponded to those of CCOT type 1, the most commonly found histologic subtype. The treatment of the cystic (type 1) variant of CCOT is usually conservative. Such treatment includes enucleation with curettage for intraosseous lesions and local excision for the extraosseous lesions. Enucleation with curettage is the most approved treatment for intraosseous lesions rather than enucleation alone18. Enucleation with curettage means the removal of a 1- to 2-mm layer of bone around the periphery of the cystic cavity with a sharp curette or a bone bur. The purpose of this procedure is to eliminate the epithelial debris from which a recurrent lesion could originate1114. The solid variant of CCOT, which is often called a dentinogenic ghost cell tumor, is usually more aggressive. The most common treatment method for this solid variant of CCOT is excision19.
Although the prognosis of the cystic type of CCOT is favorable, the presented patient had experienced two recurrences in five years before he was referred to our department. Although the lesion initially showed regression, the recurrent symptoms of nasal obstruction and cheek tenderness appeared two years after the first FESS procedure. The patient showed similar symptoms with apparent extension of the lesion on CT three years after the additional FESS procedure. (Fig. 1) The transnasal endoscopic approach to CCOT is considered more esthetic and less invasive than the conventional lateral approach20. However, this method involves risk of insufficient removal of the lesion. Since CCOT arises from odontogenic epithelial remnants that are often in a periapical or lateral periodontal relationship to adjacent teeth, treatment such as endodontic therapy or extraction of the involved teeth needs to be performed. When enucleation is considered the treatment of choice, the lesion should be thoroughly removed, including that in the area of the affected teeth area.
Although there were two recurrences in the presented case, the patient was again treated conservatively utilizing marsupialization as a decompression method not only to minimize the damage to anatomical structures, but also to reduce the size of the lesion. Marsupialization has been performed as a more conservative type of treatment for large cystic lesions in order to minimize cyst size and to reduce the extent of surgery. For the treatment of CCOT, marsupialization was first employed by Souza et al.14. The authors suggested that marsupialization could be used as a preliminary treatment option for CCOT to minimize damage to the anatomical structures. Sakai et al. emphasized the importance of marsupialization before total surgical removal in young patients with large CCOT lesions8.
After marsupialization, the patient was regularly followed and was subjected to saline irrigation through a tube inserted into the lesion at every follow-up visit.(Fig. 3. A) Remarkable regression of the lesion and bone apposition on the inner wall of the lesion were noted.(Fig. 3. C) After the enucleation, new bone was continuously deposited into the cavity where the lesion had existed, and the cavity size was reduced.(Fig. 6) Interestingly, gradual shrinkage of the lesion was accompanied by restoration of maxillary sinus volume. During this process, the bony wall of the cystic tumor became more apparent and thicker. Because of the thickened bony boundary, enucleation and aggressive bony curettage can be achieved without sinus wall destruction. This maxillary sinus pneumatization continues to progress even after removing the lesion surgically. Thus, some of the sinus volume was regained without intentionally removing the sinus wall. The patient was followed for three year after the surgical treatment, and there were no signs of relapse.
In conclusion, this case reports describes another case of recurrent CCOT in the posterior maxilla, which is not frequently reported. Even though a long-term follow-up study and additional cases are needed, marsupialization can be considered when planning the initial treatment of recurrent CCOT, especially in young patients with large maxillary lesions extending into the maxillary sinus.
References
1. Gorlin RJ, Pindborg JJ, Clausen FP, Vickers RA. The calcifying odontogenic cyst: a possible analogue of the cutaneous calcifying epithelioma of Malherbe. Oral Surg Oral Med Oral Pathol. 1962; 15:1235–1243. PMID: 13949298.
2. Praetorius F, Hjørting-Hansen E, Gorlin RJ, Vickers RA. Calcifying odontogenic cyst. Range, variations and neoplastic potential. Acta Odontol Scand. 1981; 39:227–240. PMID: 6948493.
3. Neville BW, Damm DD, Allen CM, Bouquot J. Oral and maxillofacial pathology. 3rd ed. St. Louis: Saunders;2008. p. 695–697.
4. Reyes D, Villanueva J, Espinosa S, Cornejo M. Odontogenic calcificant cystic tumor: a report of two clinical cases. Med Oral Patol Oral Cir Bucal. 2007; 12:E126–E129. PMID: 17322800.
5. Thinakaran M, Sivakumar P, Ramalingam S, Jeddy N, Balaguhan S. Calcifying ghost cell odontogenic cyst: a review on terminologies and classifications. J Oral Maxillofac Pathol. 2012; 16:450–453. PMID: 23248487.

6. Buchner A. The central (intraosseous) calcifying odontogenic cyst: an analysis of 215 cases. J Oral Maxillofac Surg. 1991; 49:330–339. PMID: 2005490.

7. Iida S, Fukuda Y, Ueda T, Aikawa T, Arizpe JE, Okura M. Calcifying odontogenic cyst: radiologic findings in 11 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:356–362. PMID: 16504870.

8. Chindasombatjaroen J, Poomsawat S, Boonsiriseth K. Two unique cases of calcifying cystic odontogenic tumor in the maxillary posterior region. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014; 118:497–504. PMID: 25201118.

9. Hirshberg A, Kaplan I, Buchner A. Calcifying odontogenic cyst associated with odontoma: a possible separate entity (odontocalcifying odontogenic cyst). J Oral Maxillofac Surg. 1994; 52:555–558. PMID: 8189290.

10. Chindasombatjaroen J, Poomsawat S, Klongnoi B. Calcifying cystic odontogenic tumor associated with other lesions: case report with cone-beam computed tomography findings. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 113:414–420. PMID: 22669147.

11. Daniels JS. Recurrent calcifying odontogenic cyst involving the maxillary sinus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 98:660–664. PMID: 15583537.

12. Sciubba JJ, Fantasia JE, Kahn LB. Tumors and cysts of the jaws. Washington: Armed Forces Institute of Pathology;2001. p. 43–45.
13. Cheng YS, Wright JM, Walstad WR, Finn MD. Calcifying epithelial odontogenic tumor showing microscopic features of potential malignant behavior. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 93:287–295. PMID: 11925538.

14. Souza LN, Souza AC, Gomes CC, Loyola AM, Durighetto AF Jr, Gomez RS, et al. Conservative treatment of calcifying odontogenic cyst: report of 3 cases. J Oral Maxillofac Surg. 2007; 65:2353–2356. PMID: 17954339.

15. Tanimoto K, Tomita S, Aoyama M, Furuki Y, Fujita M, Wada T. Radiographic characteristics of the calcifying odontogenic cyst. Int J Oral Maxillofac Surg. 1988; 17:29–32. PMID: 3127486.

16. Struthers P, Shear M. Root resorption by ameloblastomas and cysts of the jaws. Int J Oral Surg. 1976; 5:128–132. PMID: 820661.

17. Ledesma-Montes C, Gorlin RJ, Shear M, Prae Torius F, Mosqueda-Taylor A, Altini M, et al. International collaborative study on ghost cell odontogenic tumours: calcifying cystic odontogenic tumour, dentinogenic ghost cell tumour and ghost cell odontogenic carcinoma. J Oral Pathol Med. 2008; 37:302–308. PMID: 18221328.

18. Ellis E. Surgical management of oral pathologic lesions. In : Patterson LJ, Ellis E, Hupp JR, Tucker MR, editors. Contemporary oral and maxillofacial surgery. 2nd ed. St. Louis: Mosby-Year Book;1993. p. 526–553.
19. Brøndum N, Jensen VJ. Recurrence of keratocysts and decompression treatment. A long-term follow-up of forty-four cases. Oral Surg Oral Med Oral Pathol. 1991; 72:265–269. PMID: 1717918.
Fig. 1
Computed tomography shows recurrence of the lesion after the first functional endoscopic sinus surgery (FESS) procedure. A. Expansile cyst-like lesion at the first visit. B. A recurrent lesion two years after the first FESS.
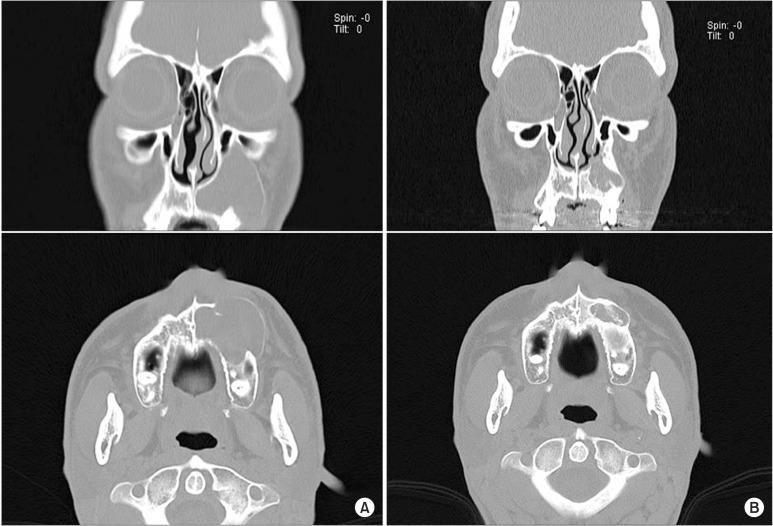
Fig. 2
When the patient was referred to our department, three years after the second functional endoscopic sinus surgery procedure, he showed recurrence in the same region. A. A panoramic radiograph revealing the large extension of unilocular radiolucency in the left maxilla. B. Computed tomography scan showing a large lesion in the left maxillary sinus expanding up to the inferior orbital floor and projecting into the nasal cavity.
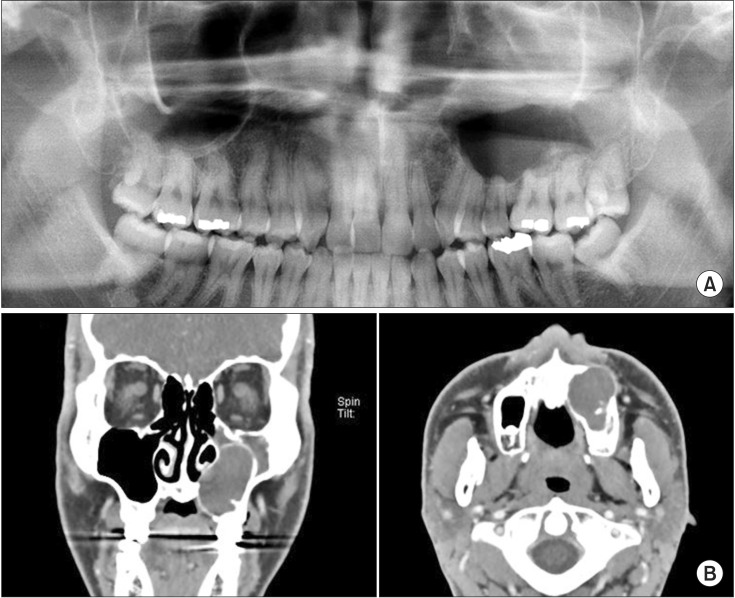
Fig. 3
A. Cyst marsupialization and placement of an acrylic tube for drainage. B. Five months computed tomography (CT) image after the endodontic treatment and marsupialization. C. Cone-beam CT scan showing the regressed lesion and new bone deposition around the lesion.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download