Abstract
The purpose of this study is to report a rare case of mandibular adenocarcinoma that was diagnosed due to metastasis from the prostate. Numb chin syndrome (NCS), which was associated with this case, is also discussed. Computed tomography (CT) and an intraoral incisional biopsy of the left mandibular area were performed. Urology consultation, hormone therapy, chemotherapy and follow-up radiographic images were administered. Histological examination of the incised specimen revealed moderately differentiated adenocarcinoma. The Gleason score was 8 (primary 4/secondary 4). Immunohistochemical features and radiographic results confirmed the diagnosis of metastasis from prostate adenocarcinoma, moderately differentiated. The patient's prostate-specific antigen (PSA) level was very high. After hormone treatment, the patient's PSA levels dropped gradually. Seventeen months later, in May 2015, the PSA level was elevated. The 18-month follow-up CT image indicated that the patient's condition was aggravated. Docetaxel chemotherapy was started in June 2015 (18 months later), and the sixth cycle of the therapy is in progress. Oral metastases that originate from prostate adenocarcinoma are rare and can induce various periosteal reactions. Hormone therapy, chemotherapy and close follow-up could be additional, appropriate treatment, and were applied in this case. Finally, NCS is a valuable indicator of metastatic disease in the mandible.
Prostate carcinoma is caused by development of cancer in the prostate, a gland in the male reproductive system. Metastatic tumors from the primary region to the oral cavity are rare, and account for only 1% of all malignant oral neoplasms. The proportional frequency of cases with oral and maxillofacial metastases that originate in the prostate to the total number of cases with oral and maxillofacial metastases that originate in all primary sites is about 6.2%1. Because of this low case frequency, it is important to determine the right diagnosis and treatment of oral cavity metastases from the prostate gland. Hirshberg et al.2 stated that symptoms associated with metastases include rapid swelling, pain and paresthesia, which can be cardinal symptoms of jaw metastases.
The purpose of this study is to report a rare case of a metastasis from the prostate adenocarcinoma that was diagnosed with a biopsy. The Gleason system has been introduced to aid tumor evolution prediction and pathological staging. In addition, this case also discusses numb chin syndrome (NCS), which is an uncommon neurological manifestation caused by metastatic malignancy.
An 80-year-old man was referred to our outpatient clinic by a dentist in December 2013, with complaints of numbness and swelling on the left site of the mandible. The patient stated that he had been suffering from this numbness for 7 months and swelling for 3 to 4 months.
A diffuse radiolucent lesion was observed in the left mandibular angle region with a panoramic radiograph. Oropharynx computed tomography (CT) showed a 6×.7×7.2 cm3-sized enhancing mass with a sunburst periosteal reaction in the ramus, angle and posterior body of the left mandible. It also showed invasion to the left medial pterygoid muscle and lateral pterygoid process, bulging into the left lateral mouth floor and shifting inferiorly to the left submandibular gland, without pathologic cervical lymph nodes.(Fig. 1)
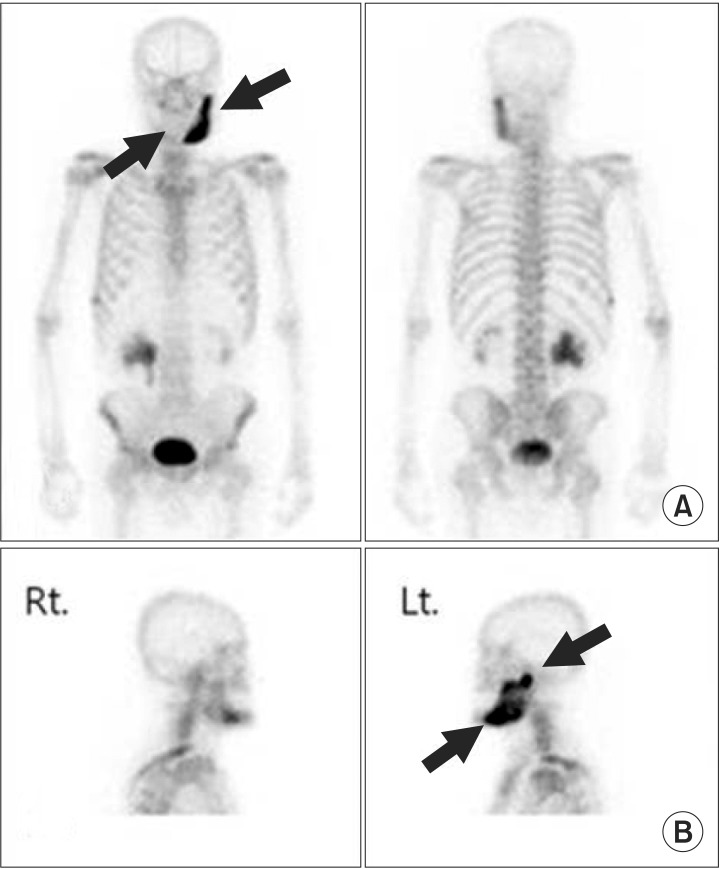
Biopsy was performed under local anesthesia. Histological examination (H&E staining) of the incised specimen revealed moderately differentiated adenocarcinoma. The Gleason score was 8 (primary 4/secondary 4) and it was predicted to be moderately aggressive. Immunohistochemical stain results maxshowed prostate-specific antigen (PSA–positive; cytokeratin 7, cytokeratin 20, TTF-1, and S100–negative).(Fig. 2) The patient was sent for medical consultation and an abdomenpelvis CT, prostate magnetic resonance imaging, and bone scan were performed. The bone scan showed abnormal, increased bony uptake in the left mandible, right lateral 8th and 9th ribs, and right posterior 9th to11th ribs.(Fig. 3) These immunohistochemical features and radiographic results confirmed the diagnosis of metastasis from the prostate adenocarcinoma, moderately differentiated.
The PSA level was very high (>5,000 ng/mL; normal range, <4.4 ng/mL). The patient was started on leuprorelin acetate and given a 3.75 mg injection every 4 weeks, and a bicalutamide 50 mg tablet every day. After hormone treatment, the patient's PSA level dropped to 505 ng/mL (after 1 month), 55 ng/mL (after 5 months), 28 ng/mL (after 9 months), and 47 ng/mL (after 14 months).
A mandible CT showed decreased extent of soft tissue mass, increased sclerotic changes, and a residual tumor that involved the left mandible and adjacent masticator space (5 months follow-up). A follow-up positron emission tomography-CT after 10 months showed sclerotic change with mild fluorodeoxyglucose (FDG) uptake in the left mandible (maximum standard uptake value, maxSUV=2.40; SUV=tissue radioactivity concentration [MBq/mL]/injected dose [MBq]× BW [g]).(Fig. 4)
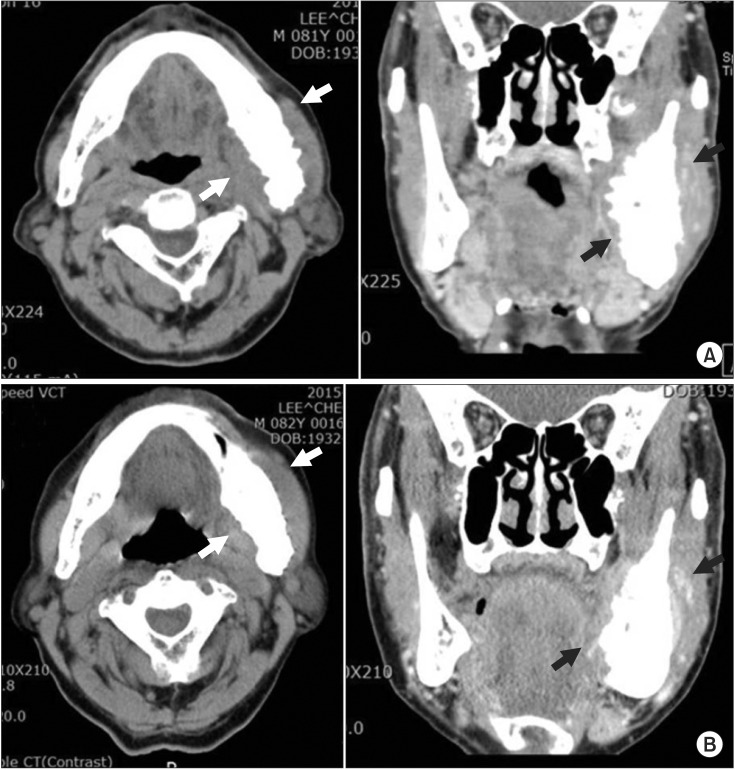
However, in May 2015 (17 months later), the PSA level was elevated to 315 ng/mL. The 18 month follow-up visit mandible CT showed an increased soft tissue mass that involved the left mandible and adjacent masticator space, decreased extent of sclerotic changes and periosteal reaction. (Fig. 5) The patient was evaluated as aggravated. Docetaxel chemotherapy (125 mg injection/1 cycle) was started in June 2015 (18 months later) and is currently in the sixth cycle. Until now, the patient was moderately tolerant to hormonal and chemical treatment for several months and he has been in follow-up for 28 months.
Prostate carcinoma is caused by cancer in the prostate, a gland in the male reproductive system. Jaw metastasis occurs less frequently, compared to the involvement of other bones of the body3 and represents 1% of all malignant mouth neoplasms. Shen et al.1 showed that the proportional frequency of cases with oral and maxillofacial metastases that originate in the prostate to the total number of cases with oral and maxillofacial metastases that originate in all primary sites is about 6.2%. Aksoy et al.3 determined that the most common sites of primary tumors in men were lungs (22.3%), prostate (12%), kidney (10.3%), bone (9.2%), and adrenals (9.2%). Because of this low frequency but common primary sites, it is important to accurately diagnosis and treat oral cavity metastases from the prostate gland4.
The Gleason system has been introduced for tumor evolution prediction and to determine pathological staging. The Gleason score is the sum of the pattern-number of the primary and secondary grades based upon microscopic appearances. A score of 2 to 4 (well differentiated) is mild, while a score of 7 to 10 is more aggressive and has a bad prognosis5. In this case, the primary tumor grade was 4 and the secondary tumor grade was 4, so the Gleason score was 4+4=8. Histological features were moderately differentiated, and predicted to be moderately aggressive.
Prostate cancer usually metastasizes to bones, such as lumbar vertebrae, thoracic vertebrae, and the pelvis6. Prevertebral venous plexus drainage is the predominant method for bony spread7. In the maxillofacial region, prostate carcinomas target the jawbone. In men, 11% of the jawbone metastases originated from the prostate gland compared with 1.5% in the soft tissues2. The mandible was found to be the most affected site for oral metastasis (35.6%). The molar and premolar region was the most frequently involved (53.0%), followed by the ascending ramus (31.6%), mandibular angle (17.8%), condyle (15.8%), and the mental region (6.1%)1. The posterior mandible is the most susceptible metastasis site because of its rich blood supply and hematosis7.
NCS is an uncommon neurological manifestation of an oral cavity metastatic tumor. Sensory discomfort could be the first sign of infiltration when the prostate cancer metastasizes to the mandible8910. The first case of NCS was reported by Charles Bell in 1830 in his monograph 'The nervous system of the human body'11. Clinical features of mandibular metastases present as toothache, rapid swelling, pain and paresthesia. These symptoms sometimes lead to extraction of the affected tooth2. This patient had been suffering from this numbness for 7 months and swelling for 3 to 4 months without any detectable symptoms too. Accordingly, it is important to recognize NCS as an uncommon neurological manifestation because of the possibility of metastatic malignancy.
Periosteal reactions can be classified as single layer, multilayered, solid, speculated, perpendicular, sloping, complex, Codman triangle and sunburst12. The appearance of a 'sunburst' periosteal reaction is suggestive of rapid onset pathology7. Most tumors produce osteolytic-like lesions. However, metastatic prostate carcinomas can secrete high amounts of the receptor activator of nuclear factor kappa-B ligand (RANKL) inhibitor osteoprotegerin, thereby weakening osteoclastic reactions during metastasis. Based on these characteristics metastic prostate neoplasms were proposed to be osteoblastic or sclerotic2. The sunburst image is most commonly associated with osteoblastic metastasis and approximately 30% are secondary to prostatic carcinoma12. Sunburst periosteal reaction in the ramus, angle and posterior body of the left mandible with clinical features, in this case, strongly suggests a malignant bone forming tumor, such as an osteosarcoma.
There are several treatment approaches for prostate cancer: radical prostatectomy, radiation therapy, chemotherapy, and endocrine therapy13. The first PSA level was very high (>5,000 ng/mL; normal range, <4.4 ng/mL). The patient was started on a leuprorelin acetate 3.75 mg injection every 4 weeks, and a daily bicalutamide 50 mg tablet. In response to these hormone treatments, the PSA level dropped to 505 ng/mL (after 1 month), 55 ng/mL (after 5 months), 28 ng/mL (after 9 months), and 47 ng/mL (after 14 months). However, in May 2015 (17 months later) the PSA level was elevated to 315 ng/mL. Because of this PSA elevation, docetaxel chemotherapy was administered.
The presence of oral metastases indicates a poor prognosis, with a mean interval of approximately 7 months between the occurrence of metastases and death2. Sometimes an aggressive case with high levels of PSA can rapidly progress to death within only 3 weeks after the detection of jawbone metastases8.
In this case, at the 18 month follow-up visit, a mandible CT image showed increased soft tissue mass that involved the left mandible and adjacent masticator space, decreased sclerotic changes and a periosteal reaction.(Fig. 5) Evaluation of the patient indicated good disease control and good tolerance to treatment over several months; however, the PSA level elevation and CT image showed that the patient's condition was aggravated, and a sixth docetaxel chemotherapy session is in progress.
In summary, periosteal reactions identified in a panorama CT scan are helpful for diagnosing malignant tumors. Hormone therapy, such as chemotherapy in this case, can extend the patient's lifespan in metastatic prostate cancer. NCS is also a useful indicator of metastatic prostate adenocarcinoma.
References
1. Shen ML, Kang J, Wen YL, Ying WM, Yi J, Hua CG, et al. Metastatic tumors to the oral and maxillofacial region: a retrospective study of 19 cases in West China and review of the Chinese and English literature. J Oral Maxillofac Surg. 2009; 67:718–737. PMID: 19304027.

2. Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, Berger R. Metastatic tumours to the oral cavity: pathogenesis and analysis of 673 cases. Oral Oncol. 2008; 44:743–752. PMID: 18061527.
3. Aksoy S, Orhan K, Kursun S, Kolsuz ME, Celikten B. Metastasis of prostate carcinoma in the mandible manifesting as numb chin syndrome. World J Surg Oncol. 2014; 12:401. PMID: 25547947.

4. Daley T, Darling MR. Metastases to the mouth and jaws: a contemporary Canadian experience. J Can Dent Assoc. 2011; 77:b67. PMID: 21683026.
5. Menezes JD, Cappellari PF, Capelari MM, Gonçalves PZ, Toledo GL, Toledo Filho JL, et al. Mandibular metastasis of adenocarcinoma from prostate cancer: case report according to epidemiology and current therapeutical trends of the advanced prostate cancer. J Appl Oral Sci. 2013; 21:490–495. PMID: 24212997.

6. Saijo H, Chikazu D, Mori Y, Hikiji H, Yonehara Y, Takato T. Metastasis of prostate cancer to the mandibular condyle. Asian J Oral Maxillofac Surg. 2008; 20:86–88.

7. Tchan MC, George M, Thomas M. Metastatic prostate cancer mimicking primary osteosarcoma of the jaw: an infrequent clinical case. South Med J. 2008; 101:657–659. PMID: 18475226.

8. Soares EC, Costa FW, Rocha-Filho FD, Ferreira FV, Alves AP. Metastatic prostate adenocarcinoma associated with numb chin syndrome. J Craniofac Surg. 2011; 22:2366–2368. PMID: 22134281.

9. Zaheer F, Hussain K, Rao J. Unusual presentation of 'numb chin syndrome' as the manifestation of metastatic adenocarcinoma of the lung. Int J Surg Case Rep. 2013; 4:1097–1099. PMID: 24240077.

10. Narendra H, Ray S. Numb chin syndrome as a manifestation of metastatic squamous cell carcinoma of esophagus. J Cancer Res Ther. 2009; 5:49–51. PMID: 19293491.

12. Wenaden AE, Szyszko TA, Saifuddin A. Imaging of periosteal reactions associated with focal lesions of bone. Clin Radiol. 2005; 60:439–456. PMID: 15767101.

13. Reyes Court D, Encina S, Levy I. Prostatic adenocarcinoma with mandibular metastatic lesion: case report. Med Oral Patol Oral Cir Bucal. 2007; 12:E424–E427. PMID: 17909506.
Fig. 1
A 6×7.7×7.2 cm3 sized enhancing mass with sunburst periosteal reaction in ramus, angle and posterior body of left mandible. A. Panorama (1st medical examination). B. Oropharynx computed tomography (CT) axial view (1st medical examination). C. Oropharynx CT coronal view (1st medical examination). Arrows indicate enhancing mass with sunburst periosteal reaction.
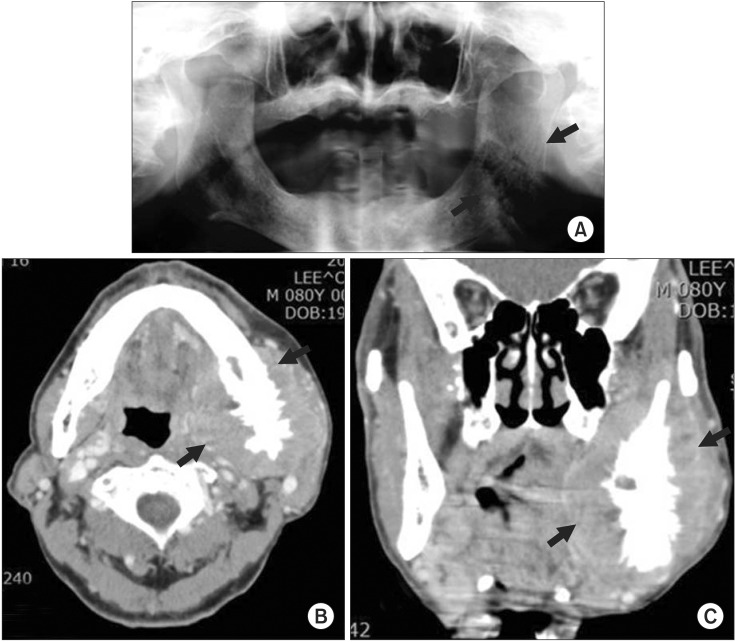
Fig. 2
Immunohistochemical stain for prostate-specific antigen (PSA–positive; cytokeratin 7, cytokeratin 20, TTF-1, and S100–negative) reveals diffuse strong positive result. A. Submucosal tissue (H&E staining, ×100). B. Submucosal tissue (PSA immunohistochemical staining, ×200).
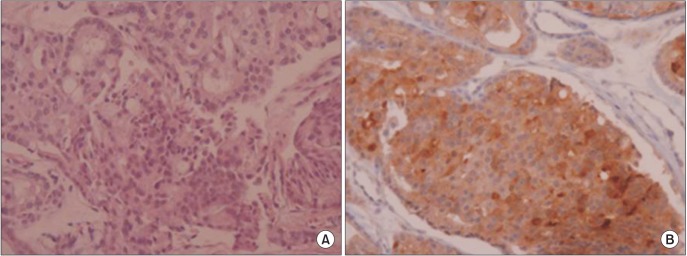
Fig. 3
Active bone lesion in left (Lt.) mandible and right (Rt.) lateral 8th and 9th ribs, right posterior 9th to 11th ribs. A. Whole body bone scan: abnormal increased bony uptake in right lateral 8th and 9th ribs, right posterior 9th to 11th ribs. B. Mandible bone scan: abnormal increased bony uptake in left mandible. Arrows indicate active bone lesion.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download