I. Introduction
Song et al.
1 first reported the anterolateral thigh (ALT) flap as a septocutaneous flap based on the descending branch of the lateral circumflex femoral artery (LCFA) in 1984. Recently, the ALT flap has become a popular option for soft tissue reconstruction of the oral cavity
23. The ALT flap offers several advantages. It is easily raised and has long and good caliber vascular pedicles with suitable vessel diameter, different tissues with large amounts of skin are available, and there is minimum morbidity at the donor site
2. Flap thickness is adjustable as required
3.
However, the ALT flap has been criticized due to variations in vascular pedicles and perforator anatomy, making flap elevation challenging
4. Therefore, this flap has not been widely used in oral and maxillofacial reconstruction. Kimata et al.
5 and Kawai et al.
6 reported anatomical variations in the ALT flap in the Japanese population and surgical concerns regarding dissection of the flap. Valdatta et al.
7 and Yu
8 reported flap characteristics in the Western population.
The ALT flap is mostly supplied by one to three perforators of the descending branch of the LCFA. It can be located clinically by measuring the midpoint of a line drawn from the anterior superior iliac spine (ASIS) to the superolateral border of the patella. However, there is some variation in the location of these perforators. In addition, the oblique branch of the LCFA often runs between the descending and the squatransverse branches of the LCFA
9. The ALT flap has other variations in cutaneous branches. Song et al.
1 reported that the ALT flap has some septocutaneous vessels. However, many reports have shown that harvested ALT flap has more musculocutaneous perforators (up to 87%)
13.
In the present study, we investigated the surgical anatomy of the ALT flap in a series of eight cases, focusing on the pattern of perforators and variation in pedicle course compared with previous studies.
Go to :

II. Materials and Methods
Cases of reconstructive surgery using ALT free flaps were enrolled from the database of all patients who underwent ablative surgery for oral and maxillofacial cancers from 2014 to 2015 in the Department of Oral and Maxillofacial Surgery in Asan Medical Center (Seoul, Korea). Eight patients were included in the study, and their medical records were carefully reviewed.
Demographic data included gender, age, pathological data, tumor stage, primary site, and whether adjuvant raidotherapy was performed. Operative records were reviewed regarding flap size, thickness, pedicle length, and anastomosis of vessels.
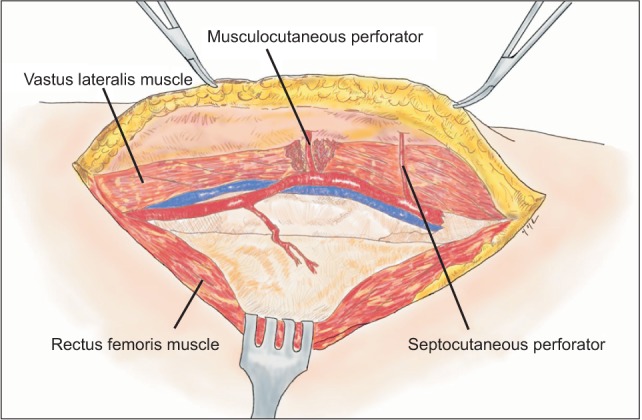
Anatomical variation was recorded during flap harvesting. The number of perforators included in the skin peddle was counted, and the perforators feeding skin were investigated as to whether they ran through the septum in the vastuslateralis muscle (septocutaneous) or through the intramuscular portion (musculocutaneous).(
Fig. 1) Yu
8 and Urken et al.
10 noted that the course of the main pedicle in ALT free flaps derived from three origins of the LCFA. Variation in the pedicle course was recorded according to classification as types I, II, and III. In type I, the vascular pedicle derives from the descending branch of the LCFA, and that in type II from the transverse branch of the LCFA. The vascular pedicle derives directly from the profunda femoris artery in type III.(
Fig. 2) We considered the pedicles of type III unusable, as did Yu
8 and Urken et al.
10, due to the small caliber and short length. Therefore, patients with type III variation were excluded because it was not possible to use the ALT flap. The study protocol was reveiwed and approved by the Institutional Review Board of Asan Medical Center (S2016-1056-0001).
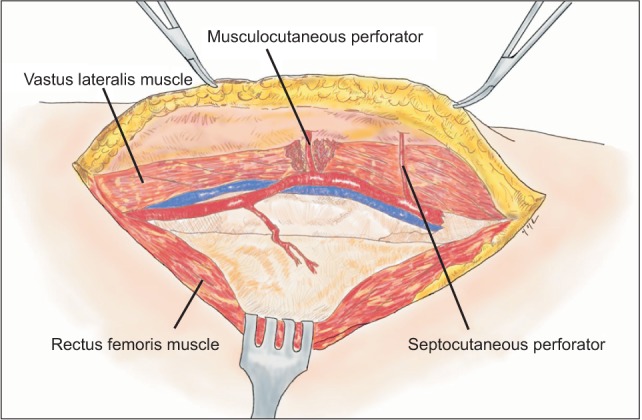 | Fig. 1Septocutaneous perforator and musculocutaneous perforator.
|
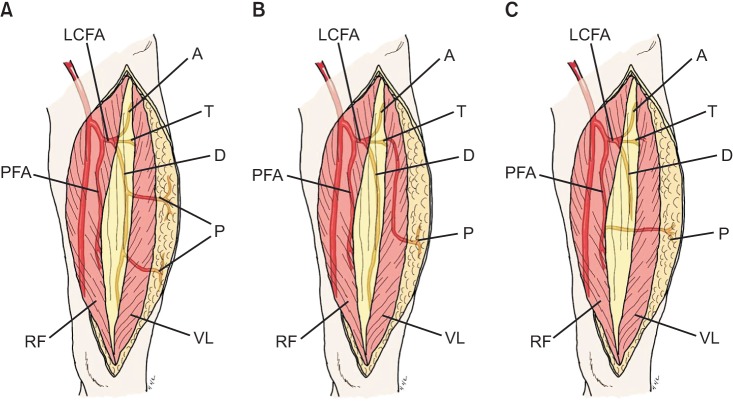
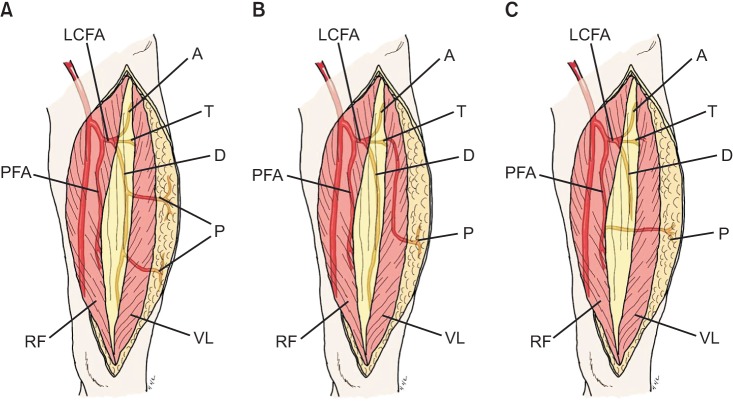 | Fig. 2The course of vascular pedicles was categorized into three types. In type I (A), the main pedicle derives from the descending branch of the lateral circumflex femoral artery (LCFA). In type II (B), the vascular pedicle is derived from the transverse branch of the LCFA instead of the descending branch. The vascular pedicle in type III (C) directly arises from the profunda femoris artery. (A: ascending branch, T: transverse branch, D: descending branch, PFA: profunda femoris artery, P: perforator, RF: rectus femoris muscle, VL: vastus lateralis muscle)
|
Go to :

III. Results
The mean age of patients was 61 years, and the male to female ratio was 4:4. The eight cases comprised six squamous cell carcinomas, one adenoid cystic carcinoma, and one osteosarcoma. Tumor stages ranged from T2N0M0 to T4N0M0, and five patients underwent postoperative radiotherapy.(
Table 1)
Table 1
Demographic data of patients
|
Variable |
Recovered |
Non-recovered |
P-value |
|
Sample |
|
46 (76.7) |
14 (23.3) |
|
|
Age (yr) |
|
26.8±6.9 |
28.9±7.5 |
|
|
Gender |
Male (n=46) |
35/46 (76.1) |
11/46 (23.9) |
0.847 |
|
Female (n=14) |
11/14 (78.6) |
3/14 (21.4) |
|
Fracture location |
Body of the mandible (n=27) |
24/27 (88.9) |
3/27 (11.1) |
0.043 |
|
Angle of the mandible (n=33) |
22/33 (66.7) |
11/33 (33.3) |
|
Fracture displacement |
More than 5 mm (n=28) |
17/28 (60.7) |
11/28 (39.3) |
0.006 |
|
Less than 5 mm (n=32) |
29/32 (90.6) |
3/32 (9.4) |
|
Post-traumatic neurosensory score |
Abnormal (n=52) |
38/52 (73.1) |
14/52 (26.9) |
0.179 |
|
Normal (n=8) |
8/8 (100) |
0/8 (0) |

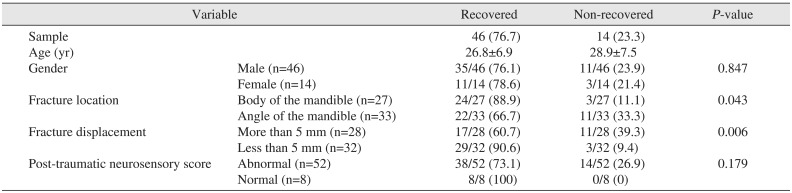
Microvascular reconstructions with ALT free flaps were performed for all surgical defects in the maxilla (five cases), buccal mucosa (two cases), and floor of the mouth (one case). (
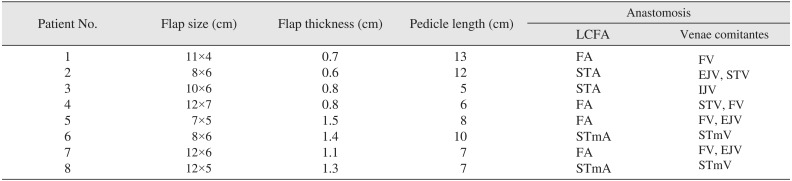
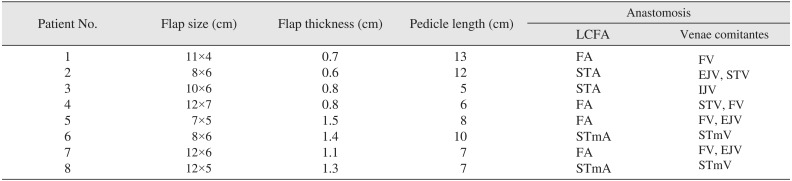
Table 1) The mean flap size was 10.0×5.6 cm, and the mean thickness was 1.0 cm. The mean pedicle length was 8.5 cm. LCFAs were anastomosed with the facial artery in four cases, superior thyroid artery in two cases, and superficial temporal artery in two cases. In vein anastomosis, one or two venae comitantes were used, and recipient veins included the facial, superior thyroid, superficial temporal, external jugular, and branches of internal or external jugular veins.(
Table 2) All flaps successfully survived. Although one case showed partial necrosis at the edge of flap, it did not affect the result of reconstruction. Flap elevations were performed through the subfascial dissection.
Table 2
Intraoperative aspects of anterolateral thigh free flaps
|
Patient No. |
Flap size (cm) |
Flap thickness (cm) |
Pedicle length (cm) |
Anastomosis |
|
LCFA |
Venae comitantes |
|
1 |
11×4 |
0.7 |
13 |
FA |
FV |
|
2 |
8×6 |
0.6 |
12 |
STA |
EJV, STV |
|
3 |
10×6 |
0.8 |
5 |
STA |
IJV |
|
4 |
12×7 |
0.8 |
6 |
FA |
STV, FV |
|
5 |
7×5 |
1.5 |
8 |
FA |
FV, EJV |
|
6 |
8×6 |
1.4 |
10 |
STmA |
STmV |
|
7 |
12×6 |
1.1 |
7 |
FA |
FV, EJV |
|
8 |
12×5 |
1.3 |
7 |
STmA |
STmV |

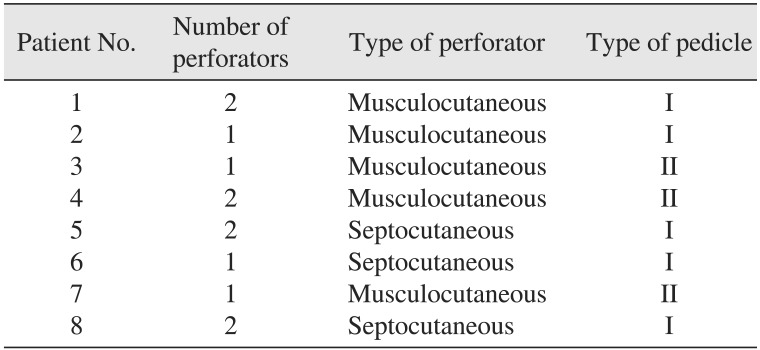
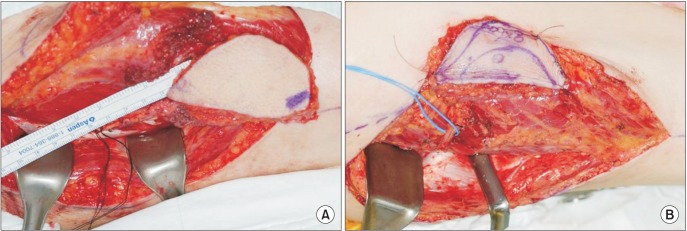
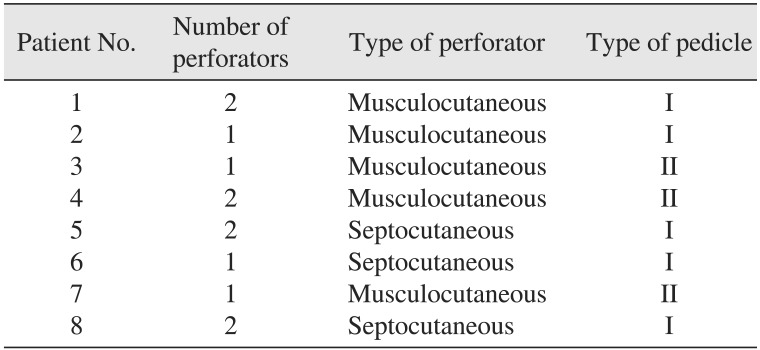
There was one perforator in four cases and two in four cases. Five patients had musculocutaneous perforators and three had septocutaneous perforators.(
Fig. 3) Type I pedicles were present in five patients, and type II pedicles in three patients who needed intramuscular dissection for flap elevation. However, type III pedicles, which are reported to occur in 1% to 5% of patients
810, were not observed in the eight cases.(
Table 3)
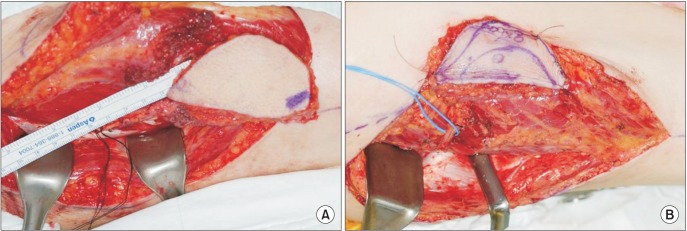 | Fig. 3Dissection of the musculocutaneous perforator and septocutaneous perforator. In the case of a musculocutaneous perforator (A), meticulous intramuscular dissection around the perforator should be performed to elevate a cutaneous soft tissue flap. The perforator and pedicle were easily elevated in the case of a septocutaneous perforator (B).
|
Table 3
Anatomical variation of anterolateral thigh free flaps
|
Patient No. |
Number of perforators |
Type of perforator |
Type of pedicle |
|
1 |
2 |
Musculocutaneous |
I |
|
2 |
1 |
Musculocutaneous |
I |
|
3 |
1 |
Musculocutaneous |
II |
|
4 |
2 |
Musculocutaneous |
II |
|
5 |
2 |
Septocutaneous |
I |
|
6 |
1 |
Septocutaneous |
I |
|
7 |
1 |
Musculocutaneous |
II |
|
8 |
2 |
Septocutaneous |
I |

Go to :

IV. Discussion
The ALT flap has many advantages for oral and maxillofacial reconstruction. It has moderate thickness, low morbidity at the flap donor site, long pedicle length, and appropriate vessel diameter. In addition, a simultaneous two-team approach can be used, with the feasibility of two skin islands based on two separate cutaneous perforators
28. With these advantages, the ALT flap has become the workhorse for oral and maxillofacial reconstruction. In our serial cases, flaps of various sizes were elevated according to defect size in the oral and maxillofacial area, which ranged from 4 to 7 cm in width and 7 to 12 cm in length. Harvested soft tissue of these sizes was considered adequate to cover most defects caused by resection of oral and maxillofacial cancers except in rare cases of a huge tumor mass that might be inoperable or should only be covered by a latissimus dorsi flap. In a study of ALT flap characteristics in the Western population by Yu
8, the mean flap thickness was 19.9 mm in women and 12.9 mm in men. Nakayama et al.
11 reported the average thickness of ALT flap in Asian population to be 7.1 mm, with intermediate thickness of subcutaneous fat compared to other free flaps used in oral and maxillofacial reconstruction such as the radial forearm free flap and rectus abdominis flap. The thickness of the harvested flap in our cases ranged from 0.6 to 1.5 cm (mean, 1.0 cm), which was comparable to the previous results. A flap thickness of about 20 mm might be the limit for use in soft tissue reconstruction of the oral and maxillofacial area, especially for the buccal mucosa and tongue except in total glossectomy. In our study, the maximum thickness of an ALT flap was 1.5 cm. The thickness of the ALT flap was considered appropriate for oral and maxillofacial defects regardless of gender. The mean pedicle length was 8.5 cm, ranging from 5 to 13 cm. Urken et al.
10 reported that the vascular pedicle of ALT flaps varied from 8 to 16 cm, although this could vary depending on patient stature, extent of proximal dissection of the LCFA, and location of skin perforators. The length of pedicles in ALT free flaps might be not a limitation for reconstruction of oral and maxillofacial area. In our series, there were no problems related to pedicle length, even when used for large defects in the maxilla with microvascular anastomosis of the flap to neck vessels such as the facial, superior thyroid, and superficial temporal vessels.
Despite these many advantages, the complicated distribution of feeding perforators and the anatomical variation of pedicle courses in the muscular structures of the ALT area have limited the widespread use of this flap
8. The first important consideration is anatomical variation in the cutaneous perforators. Yu
8 reported that perforators are most consistently located around the midpoint of the reference line from the ASIS to the superolateral border of the patella. Kimata et al.
5 also reported that cutaneous perforators were concentrated near the midpoint of this reference line. Chana and Wei
12 reported that the majority of skin perforators were located within a circle of 3 cm radius centered at this midpoint. Xu et al.
13 reported that at least one perforator was located in the inferolateral quadrant of this circle in 80% of cases. However, Choi et al.
2 reported that the cutaneous perforators were broadly distributed from 4/10 to 8/10 area between the ASIS and the superolateral border of the patella. In this study, the flaps in four cases included one perforator, and the flaps in the other four cases included two perforators. However, the number of perforators did not affect the survival or viability of the harvested flaps. We could find at least one main perforator in a circle of 3 cm radius centered at the midpoint of the reference line. Feeding perforators can be classified into two categories: septocutaneous perforators, which were first reported by Song et al.
1, run in the intermuscular space, and musculocutaneous perforators penetrate the vastus lateralis muscle
14. Valdatta et al.
7 reported that only five of 34 perforators identified were septocutaneous (14.7%). Kimata et al.
5 reported that 31 of 171 perforators (18.1%) were septocutaneous perforators. In 38 elevations of ALT flaps from a total of 160 perforators in a cadaver study by Choi et al.
2, 28 perforators (17.5%) were septocutaneous and 132 perforators (82.5%) were musculocutaneous. Similarly, Xu et al.
13 and Zhou et al.
15 reported that septocutaneous perforators were found in 40.8% of 42 cadavers and in 37.5% of 32 patients. These studies suggest that the blood supply of the ALT flap is mostly derived from musculocutaneous perforators. Therefore, a more refined surgical technique is required to dissect these perforators through the vastus lateralis muscle
2. Five of our cases had musculocutaneous and three had septocutaneous perforators. Meticulous intramuscular dissection was required for the fragile musculocutaneous perforators. This additional procedure was time-consuming and cumbersome, but did not affect the design or size of flap that could be harvested.
The second important consideration is the course of the main pedicle of the ALT free flap. Yu
8 classified the courses of these pedicles as deviation from the LCFA. Three types of variations affect surgical dissection and the fate of the flap. They are classified as types I, II, and III
816.(
Fig. 2) In type I, the most common (90%), the descending branch sends off one to three cutaneous perforators to the flap. Surgical dissection should be relatively straightforward. Type II accounts for 4% of the cases and requires tedious dissection to free the pedicle from the vastus lateralis along its entire length
16. This scenario was encountered in three of our type II cases. In type III, the ALT flap cannot be used for free tissue transfer, and the cutaneous perforator is a direct branch of the profundus femoris vessels. It pierces the rectus femoris muscle to reach the skin and is therefore more anteriorly located. Because of the small caliber and short pedicle length, the flap was abandoned in all three cases (4%). However, it has been reported that the flap could be converted to an anteromedial thigh flap
1017.
In our cases, the ALT free flap could be used for reconstruction of various soft tissue defects, including those of relatively large size. Moreover, sufficient pedicle length was available for microvascular surgery. Some anatomical variations, such as the distribution of perforator and courses of pedicles, might be a barrier for the application of ALT free flap to various reconstruction cases. However, these problems can be overcome with an understanding of anatomical variation and meticulous surgical dissection.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download