Abstract
Objectives
We compared the transbuccal and transoral approaches in the management of mandibular angle fractures.
Materials and Methods
Sixty patients with mandibular angle fractures were randomly divided into two equal groups (A, transoral approach; group B, transbuccal approach) who received fracture reduction using a single 2.5 mm 4 holed miniplate with a bar using either of the two approaches. Intraoperatively, the surgical time and the ease of surgical assess for fixation were noted. Patients were followed at 1 week, 3 months, and 6 months postoperatively and evaluated clinically for post-surgical complications like scarring, infection, postoperative occlusal discrepancy, malunion, and non-union. Radiographically, the interpretation of fracture reduction was also performed by studying the fracture gap following reduction using orthopantomogram tracing. The data was tabulated and subjected to statistical analysis. A P-value less than 0.05 was considered significant.
Results
No significant difference was seen between the two groups for variables like surgical time and ease of fixation. Radiographic interpretation of fracture reduction revealed statistical significance for group B from points B to D as compared to group A. No cases of malunion/non-union were noted. A single case of hypertrophic scar formation was noted in group B at 6 months postsurgery. Infection was noted in 2 patients in group B compared to 6 patients in group A. There was significantly more occlusal discrepancy in group A compared to group B at 1 week postoperatively, but no long standing discrepancy was noted in either group at the 6 months follow-up.
Conclusion
The transbuccal approach was superior to the transoral approach with regard to radiographic reduction of the fracture gap, inconspicuous external scarring, and fewer postoperative complications. We preferred the transbuccal approach due to ease of use, minimal requirement for plate bending, and facilitation of plate placement in the neutral mid-point area of the mandible.
The mandible occupies a very prominent position on the face and is therefore a favored target of intentional and unintentional trauma1. The high incidence of fractures of the angle of the mandible is attributed to a thinner cross-sectional area relative to the neighboring segments of the mandible, the curvature of trajectories in the angle region, and the presence of third molars, particularly those that are impacted, which weakens the region2. It is therefore not uncommon for an oral and maxillofacial surgeon to encounter fractures of the angle of the mandible in their day-to-day practice.
The oral and maxillofacial surgeon's preference for the approach to a fracture site depends on accessibility, ease of procedure, aesthetic demands by the patient, and surgical expertise. Various approaches are used for the fixation of fractures of the angle region of the mandible. The traditional approach was an extra-oral approach. In this approach, an extra-oral skin incision was made and concealed in the submandibular shadow. This technique had certain disadvantages such as an unaesthetic scar and the risk of facial nerve injury, although exposure and direct application of the plate was better with this approach3.
To counteract these disadvantages, an alternative method called the "transoral or intraoral approach" was proposed. This approach involves operating entirely through an incision made in the oral mucosa/gingiva and is frequently used by surgeons. The disadvantages included placement of the plate in an anatomically unfavorable position, thin soft tissue coverage leading to an increase in dehiscence and exposure of the plate, and breakage of the plate due to a greater degree of intraoperative plate bending, which required to adapt to the complex contours of the superior border of the mandible. Other disadvantages include placement of plate closer to the dentition, allowing an easier and shorter path for bacterial pathogens to move from the periodontal sulcus to the fixation hardware and more prevalent loosening of the screw, as there is less bone density on the superior aspect of the mandible and the alveolus4.
The disadvantages of the transoral approach prompted surgeons to find an alternative method, namely the transbuccal approach. This approach involves an intraoral incision plus a small incision on the facial skin, which permits the use of a transbuccal trocar to allow instruments such as a drill or screwdriver to pass through. Advantages include no external scarring, fixation of the plates on the thicker lateral cortical plate of the mandible in a sagittal plane, greater soft tissue coverage, less chance of plate fracture as weakening of plates by over-bending is avoided, lower infection rate due to less movement of pathogens from the third molar region, and direct visualization and confirmation of desired occlusion during fixation45.
Since the miniplate fixation differs for the transoral and transbuccal approaches, we decided to compare the two approaches in the management of angle fractures of the mandible.
A total of 60 patients reporting to Goa Dental College and Hospital from March 2013 to December 2014 were included in this prospective study and were randomly divided into 2 equal groups based on the type of approach employed for fracture fixation (group A, transoral approach; group B, transbuccal approach). The study was ethically approved by the Goa Dental College and Hospital's Review Committee and written informed consent was obtained from all patients participating in the study.
We included patients with an age between 15 to 60 years, unilateral/bilateral mandibular angle fractures or fractures associated with other facial bone fractures with radiographic preoperative displacement of the fracture segments ranging from 1 to 5 mm, patients with controlled systemic conditions, and those willing to follow-up. We excluded patients who refused to follow-up or had a medically compromised status and patients with infections or pathologic or comminuted fractures.
Preoperatively, we recorded a detailed case history for all patients. The degree of anatomical displacement was studied with digital orthopantomogram (OPG) and posteroanterior (PA) mandible radiographs. Complete hematological investigations were performed and all patients were started on intravenous antibiotics that were continued for 5 days postoperatively in all patients. Erich arch bars were applied to the maxillary and mandibular dentition a day prior to surgery.
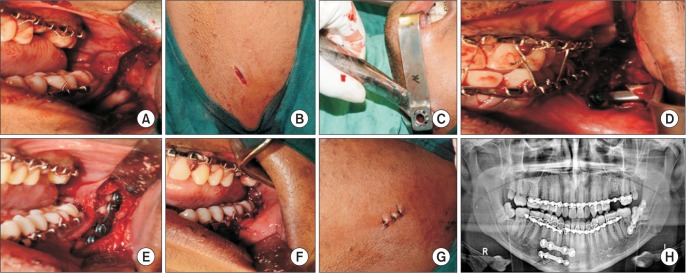
All patients were operated under general anesthesia with nasotracheal intubation following a standard surgical protocol by a single oral and maxillofacial surgeon. In group A, following local infiltration of the intraoral site with 2% lignocaine with 1:80,000 adrenaline, an incision was planned extending from the anterior border of the ascending ramus at the level of maxillary occlusal plane. The incision was then carried down just along the lateral portion of the anterior ramus and continued forward approximately 5 mm from the junction of the attached mucosa and vestibule to extend anteriorly to the level of the mandibular first molar. The mucoperiosteal flap was then raised and the fractured site was exposed.(Fig. 1. A) Fractured segments were reduced under direct vision. Satisfactory occlusion was achieved and held in place with intermaxillary fixation.(Fig. 1. B) Fractured segments were stabilized and fixed with a 2.5 mm 4-hole titanium miniplate with a gap, and were secured with monocortical screws that were 2.5-mm in diameter and 6 to 8 mm in length. These screws were threaded in position to the proper depth.(Fig. 1. C) The intermaxillary fixation was then released and occlusion was rechecked. Copious irrigation was performed with betadine and saline. The intraoral wound was closed with 3.0 vicryl sutures (Fig. 1. D) and the throat pack was removed. General anesthesia was reversed and the patient was extubated and shifted to the recovery room.
In group B, in addition to the transoral incision, a small extraoral stab incision was given to permit the insertion of the transbuccal cannula.(Fig. 2. A, 2. B) The location of the extraoral stab incision was guided by the location of the fracture line and the position of the facial vessels. The trocar was advanced into the operative site with blunt dissection through the stab incision, perforating the periosteum in the area planned for plate fixation.(Fig. 2. C) The cheek retractor was applied to stabilize the trocar assembly during movement towards and away from the fracture site. A drill bit that was 11.5 cm in length and 2.3 mm in diameter was inserted through the drill guide to drill the holes. The procedure followed for fracture reduction was similar to that of the transoral approach, except that after fracture reduction, the trocar assembly was removed and the extraoral skin incision was sutured with 5.0 ethilon (Johnson & Johnson, New Brunswick, NJ, USA) suture.(Fig. 2. D-H) All patients were hospitalized for 5 days and were placed on a liquid diet for 2 weeks, followed by a soft diet for another 4 weeks. Patients were followed at 1 week, 3 months, and 6 months.
Intraoperatively, patients were evaluated for the ease of surgical access for fixation and the surgical time (time from incision to closure). The ease of surgical access for fixation in either approach was evaluated by the operating surgeon and graded as 1, good; 2, fair; and 3, poor, based on the visual analogue scale6.
Radiographic evaluation of fracture reduction between the two groups was done by measuring the gap between the fractured segments of the mandible in postoperative OPG radiographs. These radiographs were taken within 1 day after surgery. All radiographs were performed using the Orthophos XG Machine (Sirona Dental Systems, Bensheim, Germany) with similar exposure parameters. On the radiographs, a line was drawn along the fracture and divided into three equal parts. Perpendicular lines were projected onto the fracture line to create reproducible measuring points. Measurements of the fracture gap were conducted on these 4 defined points with a digital caliper6.(Fig. 3, 4)
Postoperative complications such as scarring (in group B), occlusal discrepancy, infection, nonunion, and malunion were evaluated at each regular follow-up period.
Evaluation of scarring in group B was done with photographs at the 6th month postoperatively. The scoring for the scar was as follows: 1, hypertrophic scar; 2, invisible scar; and 3, barely visible scar7.
Postoperative occlusion was evaluated using the following scoring system: 1, pre trauma; 2, minor discrepancy; and 3, major discrepancy8.
The data was tabulated and subjected to statistical analysis (SPSS version 13; SPSS Inc., Chicago, IL, USA). A P-value less than 0.05 was considered significant.
The mean age in this study was 26.73 years (range, 17-53 years), with a peak incidence in the second and third decades of life (n=46, 76.7%) which showed male predominance (n=58, 96.7%). Road traffic accidents accounted for the majority of the cases (n=52, 86.7%). Isolated mandibular angle fracture was seen in 20 patients (33.3%), with a higher incidence of right sided fracture (n=36, 60.0%) when compared to the left (n=24, 40.0%).
The ease of surgical access for fixation revealed no statistical significance when compared between the two groups. (Table 1) The mean surgical time for each group was 37 minutes and did not vary between groups.(Table 2)
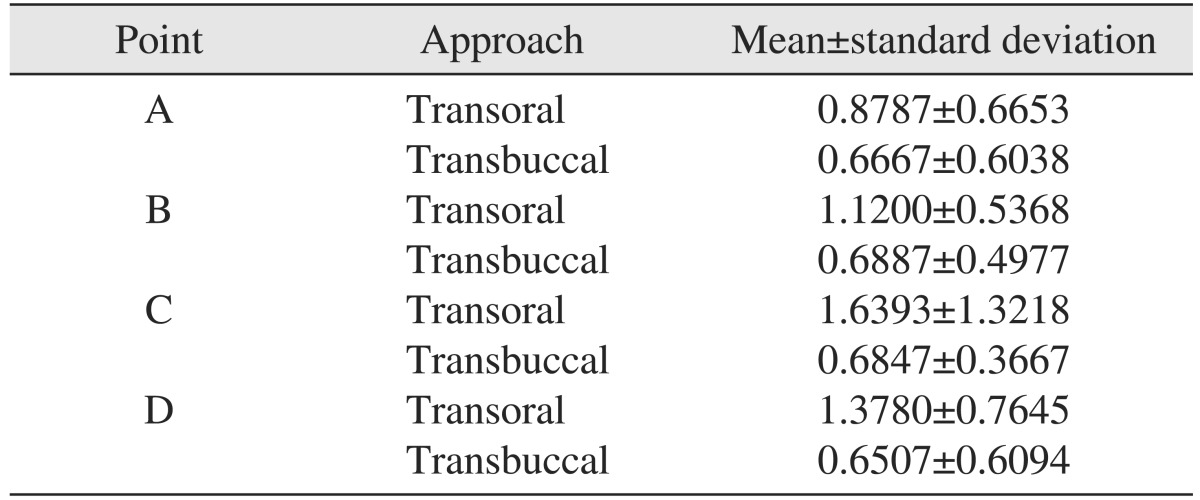
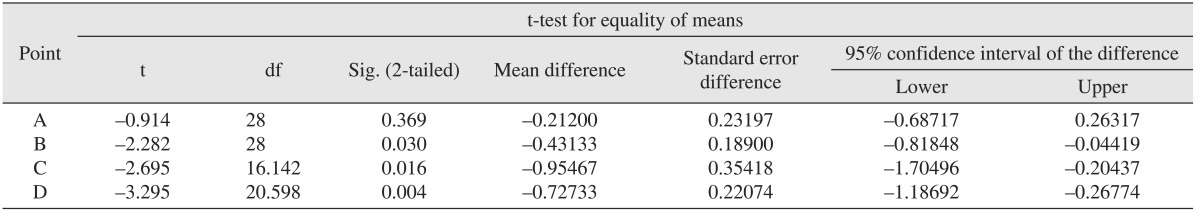
Postoperative radiographic tracing for both groups was done on the OPG. It was noted that the reduction in the gap in group B was uniform from points A to D, whereas in group A, there was gradual increase in the distance between the fractured segments.(Table 3) There was no statistical difference at point A for both groups. However, points B (P=0.030), C (P=0.016), and D (P=0.004) were statistically different between groups.(Table 4)
With regard to postoperative complications, scar evaluation in group B at 6 months revealed 1 patient (3.3%) with a hypertrophic scar, 6 patients (20.0%) with barely visible scars, and 23 patients (76.7%) with invisible scars. Infection was noted in 2 patients (6.7%) in group B, compared to 6 patients (20.0%) in group A at 3 months postoperatively. The cause of the infection could be traced to the infected plates that were removed under local anesthesia, and patients were prescribed a course of oral antibiotics for 5 days. Healing was uneventful in all cases. No cases of malunion or non-union were noted in the two groups. With regard to postoperative occlusion, 28 patients in group B had a score of 1 (pre-trauma occlusion), compared to 16 patients in group A (P=0.027, significant). Twelve patients in group A had a score of 2 (mild discrepancy), compared to 2 patients in group B (P=0.016, significant). Two patients in group A had a score of 3 (major discrepancy), compared to no patients in group B.(Table 5) The occlusal discrepancy was noted only in the first week postsurgery in either group and was corrected using elastic traction in all patients. No patients underwent re-operation for correction of an occlusal discrepancy.
The mandibular angle is subjected to forces between the muscles of mastication and the supra-hyoid group of muscles, resulting in unstable rotation of distal and proximal fragments. The presence of an impacted third molar tooth in the line of fracture may result in the fracture being compounded intraorally, which may distract away from bone or interfere in ideal fracture reduction9.
Although the management of mandibular angle fractures is still a topic of debate, the treatment is dictated by the principles of fixation and aesthetic demand by the patient. As treatments and equipment have evolved, miniplate fixation can now be carried out in an anatomically favorable position using a transbuccal approach. However, some surgeons do not prefer the transbuccal technique due to the theoretical risk of damage to the facial nerve and an unfavorable facial scar1011.
In this study of 60 patients, the incidence of mandibular angle fractures was seen in ages ranging from 17 to 53 years, with a mean age of 26.73 years. The peak incidence of fractures was seen in the second and third decades of life (n=46, 76.7%) with a definite predilection in males (n=58). Road traffic accidents was the most common etiological factor, (n=52, 86.7%) followed by assault (n=8, 13.3%). The findings were in unison with a study conducted by Kumar et al.12, which reported the pattern of maxillofacial fractures in 2,731 patients. The highest incidence of fractures in this study was found in the second and third decades of life (n=1,535, 56%). The male to female ratio was 6:1. Road traffic accidents were the most frequent cause (n=2,086, 76%), followed by assault (n=260, 12%). Another similar study13 looked at 214 patients and stated that the incidence of angle fractures was higher in the male population and was most common in the third decade of life.
Although we report that surgical access is facilitated with the transbuccal approach, we did not observe any statistically significant differences between the two approaches for this parameter.
Surgical time is defined as the time taken from incision and exposure of the fractured site to closure. It was 37 minutes for both the transoral and transbuccal approaches. This finding contradicted studies in the literature that have shown increased surgical time with the transbuccal approach when compared to the transoral approach1011.
Radiographic evaluation of fracture reduction was performed by studying the gap using tracings done on the OPG. There was no statistical difference at point A in both groups. However, points B (P=0.030), C (P=0.016), and D (P=0.004) were statistically different between groups. The reduction obtained in group B was uniform from points A to D, whereas in group A, there was a gradual increase in the distance between the fractured segments. We believe that the favorable position of the miniplate in the transbuccal approach brings about better control of the tensile and compressive forces, resulting in more uniform reduction in the fracture gap from points B to D. This observation was in accordance with a study on three-dimensional models by Kroon et al.14 and Choi et al.15, who observed bony gaps along the inferior fracture border and found that this fracture movement was a contributory factor for subsequent complications, including infection.
A study by Wan et al.4 states that in transbuccal approach, no patients developed facial nerve palsy, whereas 1 patient out of 227 (45%) developed a hypertrophic scar from the 6-mm facial skin incision. Another study by Sugar et al.10 reported similar findings in a population of 84 patients. No incidence of unsatisfactory facial scarring and facial nerve palsy from the transbuccal approach was noted. This is in accordance with our study, which reported 1 case (3.3%) of hypertrophic scarring and no incidence of facial nerve palsy in group B.
Three months after surgery, only two patients in group B had an infection, as compared to six patients in group A. This was due to the infected plate, which was retrieved under local anesthesia. A course of oral antibiotics for 5 days was subsequently prescribed and the healing was uneventful. A study by Barry and Kearns9 reported infection in 4 out of 50 patients in which the plate was retrieved at an out-patient department. Another study by Ellis and Walker16 reported infection occurring within two weeks of surgery in 2 out of 81 patients; this infection was treated initially with oral antibiotics, which resulted in normal fracture healing. These complications were related to the presence of hardware and intraoral incisions.
The gold standard in management of mandibular fracture is to establish the pre-trauma occlusion with minimal postoperative complications. When postoperative occlusion was assessed, the transoral group had significantly more occlusal discrepancy than the transbuccal group. The discrepancy in occlusion was observed only in the first week postsurgery and was managed using light guiding elastics in all patients, with no re-surgical intervention required in any patient. No patient presented with occlusal discrepancy at 6 months postsurgery. Malocclusion may be due to the presence of concomitant fractures which may contribute to instability at the mandibular angle fracture site10. This is in concordance with our study, which showed concomitant fractures in 11 patients (73.3%) in group A and 9 patients (60%) in group B. The rate of postoperative malocclusion reported in the literature ranges from 0% to as high as 7.5%.
Sugar et al.10 presented a study showing a strong preference of surgeons for fixation using a transbuccal approach. The principal reasons given were ease of use, minimal requirement for plate bending, and facilitation of plate placement in the neutral mid-point area of the mandible. Our experience with the transbuccal approach was somewhat similar.
A meta-analysis by Al-Moraissi and Ellis17 states that the use of one miniplate is superior to the use of two miniplates in the management of mandibular angle fractures, as the incidence of postoperative complications was considerably lower. This is concordant with the present study, which showed better results when a single miniplate was used either transorally or transbuccally.
In conclusion, although both approaches have inherent advantages and disadvantages, the transbuccal approach was superior to the transoral approach with regard to radiographic reduction in the fracture gap, inconspicuous external scarring, and fewer postoperative complications. We did not find increased operating time or damage to the facial nerve, which was observed by other authors when the transbuccal approach was employed. We preferred the transbuccal approach over the transoral approach due to ease of use, minimal requirement for plate bending, and facilitation of plate placement in the neutral mid-point area of the mandible. A study employing a larger sample size and without any confounding variables is ongoing to define our results even more precisely.
References
1. Khan A, Khitab U, Khan MT, Salam A. A comparative analysis of rigid and non-rigid fixation in mandibular fractures: a prospective study. Pak Oral Dental J. 2010; 30:62–67.
2. Fox AJ, Kellman RM. Mandibular angle fractures: two-miniplate fixation and complications. Arch Facial Plast Surg. 2003; 5:464–469. PMID: 14623682.
3. Toma VS, Mathog RH, Toma RS, Meleca RJ. Transoral versus extraoral reduction of mandible fractures: a comparison of complication rates and other factors. Otolaryngol Head Neck Surg. 2003; 128:215–219. PMID: 12601317.

4. Wan K, Williamson RA, Gebauer D, Hird K. Open reduction and internal fixation of mandibular angle fractures: does the transbuccal technique produce fewer complications after treatment than the transoral technique? J Oral Maxillofac Surg. 2012; 70:2620–2628. PMID: 22959879.

5. Dierks EJ. Transoral approach to fractures of the mandible. Laryngoscope. 1987; 97:4–6. PMID: 3796174.

6. Devireddy SK, Kishore Kumar RV, Gali R, Kanubaddy SR, Dasari MR, Akheel M. Transoral versus extraoral approach for mandibular angle fractures: a comparative study. Indian J Plast Surg. 2014; 47:354–361. PMID: 25593420.

7. Subramanian B, Krishnamurthy S, Suresh Kumar P, Saravanan B, Padhmanabhan M. Comparison of various approaches for exposure of infraorbital rim fractures of zygoma. J Maxillofac Oral Surg. 2009; 8:99–102. PMID: 23139484.

8. Laverick S, Siddappa P, Wong H, Patel P, Jones DC. Intraoral external oblique ridge compared with transbuccal lateral cortical plate fixation for the treatment of fractures of the mandibular angle: prospective randomised trial. Br J Oral Maxillofac Surg. 2012; 50:344–349. PMID: 22421389.

9. Barry CP, Kearns GJ. Superior border plating technique in the management of isolated mandibular angle fractures: a retrospective study of 50 consecutive patients. J Oral Maxillofac Surg. 2007; 65:1544–1549. PMID: 17656281.

10. Sugar AW, Gibbons AJ, Patton DW, Silvester KC, Hodder SC, Gray M, et al. A randomised controlled trial comparing fixation of mandibular angle fractures with a single miniplate placed either transbuccally and intra-orally, or intra-orally alone. Int J Oral Maxillofac Surg. 2009; 38:241–245. PMID: 19167189.

11. Gear AJ, Apasova E, Schmitz JP, Schubert W. Treatment modalities for mandibular angle fractures. J Oral Maxillofac Surg. 2005; 63:655–663. PMID: 15883941.

12. Kumar GB, Dhupar V, Akkara F, Kumar SP. Patterns of maxillofacial fractures in Goa. J Maxillofac Oral Surg. 2015; 14:138–141. PMID: 26028827.

13. Meisami T, Sojat A, Sàndor GK, Lawrence HP, Clokie CM. Impacted third molars and risk of angle fracture. Int J Oral Maxillofac Surg. 2002; 31:140–144. PMID: 12102410.

14. Kroon FH, Mathisson M, Cordey JR, Rahn BA. The use of miniplates in mandibular fractures. An in vitro study. J Craniomaxillofac Surg. 1991; 19:199–204. PMID: 1894737.
15. Choi BH, Kim KN, Kang HS. Clinical and in vitro evaluation of mandibular angle fracture fixation with the two-miniplate system. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995; 79:692–695. PMID: 7621024.

16. Ellis E 3rd, Walker LR. Treatment of mandibular angle fractures using one noncompression miniplate. J Oral Maxillofac Surg. 1996; 54:864–871. PMID: 8676232.

17. Al-Moraissi EA, Ellis E 3rd. What method for management of unilateral mandibular angle fractures has the lowest rate of postoperative complications? A systematic review and meta-analysis. J Oral Maxillofac Surg. 2014; 72:2197–2211. PMID: 25236822.
Fig. 1
Transoral approach. A. Fracture exposure. B. Fracture reduction and placement of intermaxillary fixation. C. Placement of miniplate. D. Closure. E. Postoperative radiograph.

Fig. 2
Transbuccal approach. A. Fracture exposure. B. Transfacial stab incision. C. Placement of the transbuccal trocar and placement of intermaxillary fixation. D. Plate fixation. E. Plate on the lateral aspect of the ramus. F. Intraoral closure. G. Stab incision closure. H. Postoperative radiograph.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download