Abstract
Objectives
If teeth are missing, super-eruption of teeth in the opposing arch can occur in the area and can change the occlusal plane. When missing teeth are replaced with implants, the oral surgeon must determine whether or not the super-erupted teeth need to be treated in order to normalize the occlusal plane. In this study, we evaluated the clinical prognosis of dentition after implant placement and prosthetic treatment were completed in an occlusal plane altered by super-erupted teeth in the opposing arch without additional treatment of the super-erupted teeth.
Materials and Methods
Twenty-two patients (9 males, 13 females) were treated with implants and prosthetics without addressing the super-erupted opposing dentition from April 2004 to August 2012 at Seoul National University Bundang Hospital. A total of 33 implants were placed. Values of crestal bone loss, survival rates, and surgical and prosthetic complications for an average of 29.6 months after prosthetic loading were recorded.
When a tooth is lost for any reason, an unopposed tooth can super-erupt, and the movements of teeth such as tilting toward the vacant area or tooth rotation can occur. Such changes can cause a change in the occlusal plane. Craddock et al.1 reported that 92% of unopposed teeth in a group of teeth that had at least one unopposed tooth exhibited super-eruption, with an average of 1.68 mm and maximum of 3.99 mm of super-eruption. Also, they reported an average super-eruption of 1.91 mm and 1.03 mm when the unopposed tooth was in the maxilla and the mandible, respectively. This is because super-eruption of opposing teeth is more frequent in the maxilla, while tilting of teeth is more frequent in the mandible. Kiliaridis et al.2 reported that 24% of unopposed teeth had greater than 2 mm of super-eruption, while 18% of unopposed teeth had no super-eruption. In other words, 82% of unopposed teeth exhibited super-eruption. Findings from another study concluded that the occlusal change of unopposed teeth was mostly within 2 mm; thus, observation with no treatment was one viable option3. Many reports have shown a similar pattern of super-eruption of unopposed teeth to that found in this study, although their pattern or frequency was slightly different. However, if the severe super-eruption of an unopposed tooth results in the loss of intermaxillary space, which limits the possibility of ideal restoration through prosthodontics, treatment might be necessary. With regard to immediatetreatment methods, occlusal reduction of the super-erupted tooth, placement of a prosthodontic restoration, and orthodontic intrusion or a surgical method accompanied by segmental osteotomy, none of which damage the tooth, are widely used. Since screws of a variety of materials have been designed as anchors in orthodontic treatment, orthodontic intrusion with such screws is widely used456. Segmental osteotomy, which was devised by Cohn-Stock7 and has been improved into many forms by Wassmund8, Axhausen9, Schuchardt10, and Wunderer11, is also used. The aim of this study is to evaluate the clinical prognosis of restoration of a missing tooth using an implant without any additional treatment for a super-erupted opposing tooth that has altered the occlusal plane.
This study was conducted with the approval of the Seoul National University Bundang Hospital Institutional Review Board (B-1405-252-109).
The study was conducted on patients who visited Seoul National University Bundang Hospital from April 2004 to August 2012 and had implants placed and prosthodontic treatment completed without treating super-erupted opposing teeth.
1) A super-erupted tooth opposing an implant placed in the premolar or molar area.
2) Regular periapical radiographs performed during the follow-up period.
1) Treatment of the opposing tooth with endodontic therapy, prosthodontic restoration, occlusal reduction through tooth grinding, segmental osteotomy, or orthodontic intrusion, etc., due to severe super-eruption.
2) Patients who lacked medical records or did not return for follow-up appointments.
Referring to medical records and radiographs, we examined the implant placement area, additional surgery other than implant placement, the prognosis of the opposite tooth after the implant became functional, complications, crestal bone loss, and implant survival rate. For implant survival rate, if the implant and upper prosthesis remained at the final follow-up appointment regardless of peri-implant bone loss, we classified this case as successful. With regard to prosthetic complications, we examined the presence of screw loosening, prosthetic dislodgement, or prosthetic fracture after the prosthesis became functional.
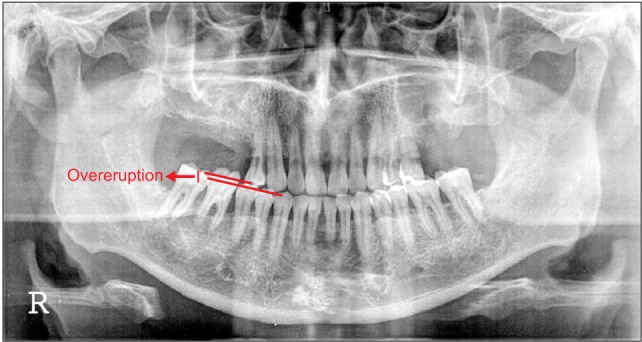
Through panoramic radiographs at 30% magnification (Fig. 1), the difference in distance between the straight line drawn between the buccal cusps of the super-erupted teeth and the straight line drawn between the buccal cusps of adjacent teeth was determined to be the amount of super-eruption.
To examine the amount of crestal bone loss, we compared a periapical radiograph collected immediately after the prosthesis became functional with a periapical radiograph performed at the final observation using the paralleling technique. We measured the amount of bone loss in the mesiodistal aspect of the implants on each radiograph to investigate the average amount of bone loss during implant function and adjusted the value after correcting for the 30% magnification of the radiograph using the length of the placed implant.
We studied a total of 22 patients, 9 males and 13 females, with an average age of 56.5 years (range, 32-72 years). A total of 33 implants were placed, 10 of which were immediately loaded after placement. For the remaining 23 implants, the final prosthetic restoration was fabricated an average healing time of 2.8 months after implant placement. The average follow-up period was 29.6 months, and the amount of super-eruption of all opposing teeth was less than 2 mm.
The implants were placed as follows: One implant in the maxillary premolar area, six implants in the maxillary molar region, one implant in the mandibular premolar space, and 27 implants in the mandibular molar area.
There were 12 cases in which additional bone grafting was performed due to the lack of alveolar bone in the implant site. In 10 cases, bone grafting was performed in the adjacent bony defect area during the placement of the implant. In two cases, implant placement was delayed after the bone graft was placed. Delayed placement of the implant was decided for one case requiring sinus graft and vertical ridge augmentation and for another case in which a socket graft was performed.
The opposing teeth did not exhibit any complications such as pain, deterioration of periodontal disease, or necessity of endodontic therapy after the implant became functional.
In one case, exposure of the cover screw occurred after the initial surgery. The screw was immediately replaced with a healing abutment. The patient recovered well without any additional complications.
There was no screw loosening or prosthetic fracture. Unfortunately, there was repetitive prosthetic dislodgement in one case.
During the 29.6 months average follow-up period after prosthetic loading, an average of 0.09±0.30 mm of bone loss was observed. In most cases, crestal bone loss was rarely observed. In one case, bone loss greater than 1 mm was observed.
A total of 31 of 33 implants survived until the final follow-up, a survival rate of 93.94%. Of the two failed implants, one was placed in the maxillary molar area and another in the mandibular molar area. One failed implant was caused by peri-implantitis, which occurred from severe nocturnal bruxism. In another case in which immediate loading was performed, the implant was removed due to its failure to osseointegrate. All failed implants were replaced, successfully restored with the final prosthesis, and functioned normally without any complications.
Super-eruption of an unopposed tooth is well-known and has been the focus of many studies. Compagnon and Woda12 classified super-eruptions into active eruptions and periodontal growth. An active eruption was defined as tooth eruption out of the socket without a change in the periodontal tissue. Periodontal growth was defined as the growth of periodontal tissue, including alveolar bone, toward the occlusal plane. In addition, the study classified an eruption caused by gingival retraction as a passive eruption that could not lead to super-eruption when it occurred alone. Super-eruption that occurred through the loss of an opposing tooth was mainly caused by periodontal growth in the early stage and by active eruption later, when the tooth was no longer functional. The study also concluded that super-eruption easily occurred, and that the eruption was usually classified as an active eruption when the periodontal condition was poor. Craddock et al.1 reported relative wear that could be regarded as a "pseudo-eruptive" condition that was related to age and usually occurred in unopposed mandibular teeth.
In this study, 26 implants were placed in the mandible and seven in the maxilla, meaning that most of the super-erupted teeth were in the maxillary arch. Many other studies on super-erupted teeth also showed a high correlation with maxillary teeth. Researchers say that most super-eruptions occur in the maxilla. One of the reasons for the high frequency of super-eruptions in the maxilla is that periodontal disease is more common in the maxilla than in the mandible due to the larger amount of trabecular bone, thinner cortical plate, and greater blood supply in the maxilla. In addition, this correlation is also due to the muscular effect of the tongue on mandibular teeth. The tongue is usually placed on the occlusal plane of mandibular teeth in a resting position, increasing the likelihood of super-eruption of mandibular dentition131415.
To date, the only reported cases involve implant treatment without treatment of the super-erupted tooth. There were 12 cases in which a bone graft was performed due to the lack of alveolar bone in the implant site.
There was no screw loosening or prosthetic fractures in this study, but we observed one case of repetitive dislodgement where a tooth was restored with a short abutment and crown. The continued dislodgement was due to the short length of the crown due to the lack of intermaxillary space. After replacing the prosthesis, no additional dislodgement occurred. During the average 29.6 months of follow-up, there was an average of 0.09±0.30 mm of crestal bone loss. In one case, greater than 1 mm of bone loss was observed. In that case, a bone graft was performed around the implant during placement, and immediate loading was applied. The loss of crestal bone was considered to be due to resorption of the bone graft materials during function.
With two of 33 implants being classified as failed, an average implant survival rate of 93.94% was observed in this study. One of the two failed implants was caused by severe nocturnal bruxism, while the other case failed as a result of immediate implant loading.
Change in the occlusal plane caused by the super-eruption of an opposing tooth has negative effects due to occlusal overload and increase in parafunction. Craddock and colleagues1617 reported in studies performed in 2004 and 2008 that occlusal interference occurred in 51.6% and 53% of cases in each unopposed posterior molar area, respectively, and that the interference increased in teeth that were unopposed for more than five years. Those studies concluded there was no significant association between the degree of super-eruption and the occurrence of occlusal interference. Although there has yet to be a study that suggests a specific treatment standard, the results of this study suggest that occlusal interference that can damage a prosthesis will not occur in the absence of treatment for super-eruption as long as the super-eruption is not excessive. The limitations of this study are mainly due to the small number of sample cases. In addition, the marginal bone loss was measured by one examiner, thus leading to possible intra-examiner error. This limits the ability to reach a reliable conclusion. More studies involving larger sample sizes would lead to more meaningful results.
During implant treatment for an occlusal scheme with a super-erupted opposing tooth, various treatments can be considered. This includes conservative, prosthodontic, orthodontic, and surgical treatments of the super-erupted tooth. Some procedures can be performed to regain the ideal intermaxillary space and occlusal plane. However, when the super-eruption distance is less than 2 mm, typical implant treatment can be performed without addressing the super-erupted opposing tooth. This study determined that lack of treatment of the super-erupted tooth will have no negative effects on the implant or the opposing tooth.
References
1. Craddock HL, Youngson CC, Manogue M, Blance A. Occlusal changes following posterior tooth loss in adults. Part 1: a study of clinical parameters associated with the extent and type of supra-eruption in unopposed posterior teeth. J Prosthodont. 2007; 16:485–494. PMID: 17559530.

2. Kiliaridis S, Lyka I, Friede H, Carlsson GE, Ahlqwist M. Vertical position, rotation, and tipping of molars without antagonists. Int J Prosthodont. 2000; 13:480–486. PMID: 11203673.
3. Faggion CM Jr, Giannakopoulos NN, Listl S. How strong is the evidence for the need to restore posterior bounded edentulous spaces in adults? Grading the quality of evidence and the strength of recommendations. J Dent. 2011; 39:108–116. PMID: 21093527.

4. Creekmore TD, Eklund MK. The possibility of skeletal anchorage. J Clin Orthod. 1983; 17:266–269. PMID: 6574142.
5. Kanomi R. Mini-implant for orthodontic anchorage. J Clin Orthod. 1997; 31:763–767. PMID: 9511584.
6. Costa A, Raffainl M, Melsen B. Miniscrews as orthodontic anchorage: a preliminary report. Int J Adult Orthodon Orthognath Surg. 1998; 13:201–209. PMID: 9835819.
7. Cohn-Stock G. Die chirurgische Immediatregulierung der Kiefer, speziell die chirurgische Behandlung der Prognathie. Vjschr Zahnheilk Berlin. 1921; 37:320.
8. Wassmund M. Lehrbuch der praktischen chirurgie des Mundes und der kiefer: Band 1. Berlin: Leipzig Meusser;1935.
10. Schuchardt K. In bier, braun, and kummel: chirurgische operationslehre. Berlin: Leipzig Meusser;1935.
11. Wunderer S. Swiss Society of Plastic and Reconstructive Surgeons. Surgical correction of the profile by operation on the maxilla. 1965. In : Proceedings: annual meeting Swiss Society of Plastic and Reconstructive Surgeons; Amsterdam: Excerpta Medica Foundation.
12. Compagnon D, Woda A. Supraeruption of the unopposed maxillary first molar. J Prosthet Dent. 1991; 66:29–34. PMID: 1941670.

13. Proffit WR. Equilibrium theory revisited: factors influencing position of the teeth. Angle Orthod. 1978; 48:175–186. PMID: 280125.
14. Gierie WV, Paterson RL, Proffit WR. Response of erupting human premolars to force application. Arch Oral Biol. 1999; 44:423–428. PMID: 10391500.

15. McArthur DR, Turvey TA. Maxillary segmental osteotomies for mandibular removable partial denture patients. J Prosthet Dent. 1979; 41:381–387. PMID: 370371.

16. Craddock HL, Youngson CC. A study of the incidence of overeruption and occlusal interferences in unopposed posterior teeth. Br Dent J. 2004; 196:341–348. PMID: 15044991.

17. Craddock HL. Occlusal changes following posterior tooth loss in adults Part 3 A study of clinical parameters associated with the presence of occlusal interferences following posterior tooth loss. J Prosthodont. 2008; 17:25–30. PMID: 17927736.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download