This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
As the craniofacial and neck regions are prime areas of injury in bear attacks, the careful management of soft and hard tissue injuries and selection of reconstructive options is of the utmost importance. This study will review the incidence and patterns of bear mauling in eastern India reported to our department and the various modalities used for their treatment over a period of 7 years. It also documents the risks of infection in bear mauling cases and the complications that have occurred.
Materials and Methods
Twenty cases were treated over the study period. Cases were evaluated for soft and hard tissue injuries including tissue loss and corresponding management in the craniofacial region. Cases were also evaluated for other associated injuries, organ damage and related complications.
Results
Various modalities of treatment were used for the management of victims, ranging from simple primary repairs to free tissue transfers. Simple primary repairs were done in 75% of cases, while the management of the injured victims required reconstruction by local, regional or distant flaps in 25%. Free tissue transfers were performed in 15% of cases, and no cases of wound infection were detected in the course of treatment.
Conclusion
Knowledge of various reconstructive techniques is essential for managing maxillofacial injuries in bear mauling cases. Modern reconstructive procedures like free tissue transfer are reliable options for reconstruction with minimal co-morbidity and dramatic improvement in treatment outcomes.
Keywords: Maxillofacial injuries, Bear, Reconstructive surgical procedures, Free tissue flaps
I. Introduction
The head, neck and more importantly the face, is the center of attraction of the human body. Consequently, this area also bears the brunt of various forms of attacks. Animal attack is a less common cause of such types of injuries, with incidences ranging from 1.2% to 2.3% of cases
12. Of all wild animal attacks, bear attacks have the highest incidence, accounting for 51.2% of the total cases reported
3. Bears have attracted the attention of scientists due to their unique adaptation of remarkable healing with almost no scarring during their period of denning, the study of which may lead to the improvements in human wound healing capacity
4. However, they have also gained the attention of surgeons by causing injuries to humans that vary from minor wounds to devastating major trauma with their five-digit paws, on which each digit has a long non-retractable claw. Although the severity of the injuries varies in bear mauling cases, death is uncommon in such attacks with an incidence of only 2.39%
5.
The management of facial injury is always a challenge for surgeons due to the dynamic nature of this region. The reconstruction of this region should provide not only tissue coverage, but also functional rehabilitation and esthetic camouflage. This study was conducted at our institution, a tertiary referral center of Eastern India. The study is focused on the incidence, pattern of injury and different modalities of treatment, ranging from simple debridement and primary closure to free tissue transfer, used for the patients who have suffered from bear mauling.
II. Materials and Methods
The study was conducted both retrospectively and prospectively in the Department of Oral and Maxillofacial Surgery from 2007 to 2015. The data were collected from the cases reported with maxillofacial injuries associated with bear mauling that were treated at Sriram Chandra Bhanja Dental College and Hospital (Cuttack, India). Institutional review board approval has been taken for this study and written permission has been obtained from the study patients to report and publish the identifying photograph's.
Cases with maxillofacial injuries were evaluated for soft and hard tissue injuries including tissue losses and organ damage, if any. They were also evaluated for other associated injuries.
The protocol followed in our institute for the management of such cases is described below.
The patient's general condition is assessed in the Emergency Department, and necessary management is done to secure the airway, breathing and circulation.
Post-trauma anti-tetanus prophylaxis is given and adequate resuscitation with fluid or blood is performed.
Post-exposure prophylaxis for rabies is given by the local infiltration of equine immunoglobulin (40 IU/kg) and two-site intradermal administration of vaccine (0.1 mL at each site) given at 0, 3, 7, and 28 days as per the suggested protocol6.
Following the thorough cleaning and debridement of wounds, soft tissue or hard tissue management is performed under general anesthesia or local anesthesia depending on the extent of the injuries.
Plans for staged reconstructive surgery are made for the patients with soft tissue or hard tissue loss, to be performed later by a team of maxillofacial surgeons.
The overall treatment outcomes, the reconstructive options used and their reliability were also noted. Any complications encountered were studied and thus managed.
III. Results
A total of 20 cases were managed in our center during the study period. Patient age ranged from 4 to 60 years (mean age, 41.1 years) and there was a strong male predominance (95%). When only the head and neck region was concerned, soft tissue injuries occurred in all cases. Bony injury was found in 95% of cases. Associated major bony injuries to other body parts were found in only 10% of cases. Upon evaluation, the patients included in the study had no significantly associated medical morbid conditions, and their routine hematological and biochemical test results were within normal limits.
Soft tissue injuries were managed by simple debridement and primary closure in 75% of cases. The majority of bony injuries were managed with open reduction and internal fixation by either miniplate fixation or trans-osseous wire fixation (78.9% of the cases). Maxillo-mandibular fixation was used in the rest of the cases as a treatment modality for bony injury. Soft tissue loss was found in five cases (25%), whereas loss of bony tissue was found in two cases (10%). Two cases required local or regional flaps for tissue coverage, while three cases required free tissue transfers for reconstruction of the defects. Bone loss was managed by providing a palatal plate for maxillary bone loss in one case and a fibula-free tissue transfer for mandibular segment loss in another case. One case also required cartilage replacement for the ala of the nose.
The overall treatment outcomes were satisfactory from the surgeons' and patients' perspectives. The reconstructive options used were successful in achieving the preset goals of treatment. Upon culturing swabs taken from the wounds, mixed microbial flora were found. Fortunately, we have not encountered complications such as infections. Complications like parotid fistulas, hypertrophic scars and enopthalmus have occurred in a few cases, and were treated successfully at a later stage.
IV. Discussion
Bear attacks mostly take place in rural areas in the early morning. Deforestation brings the bears close to human habitation in the quest for food. Observations from this study suggest
that the majority of victims are farmers or daily wagers by occupation, and that immediate medical attention is given to them by the nearest health centers at a distance of 5 to 20 km. The remote locations of attacks with the added effects of poor transportation cause delays in seeking medical care from tertiary centers, with the delays ranging from 6 to 30 hours in the current study. Although instances have been reported, the incidence of rabies after a bear attack is extremely rare. After adhering to post-exposure prophylaxis as a protocol in all cases, we did not encounter any victims suffering from rabies after a bear attack, which is in agreement with previous studies
7.
Bear mauling comprises facial injury in the majority of victims, with an incidence of 80.57%. Among the facial fractures, mandible fractures were found in nine cases (45%), zygoma fractures were found in seven cases (35%), maxilla fractures were found in four cases (20%), nasal bone fractures were found in two cases (10%), and a cranial bone fracture was found in one case in this study. Rasool et al.
5 reported incidences of soft tissue injuries in all cases that concur with this study, but our current study records much higher percentages of bony injuries (95%) than his study reported (27.09%). Zygoma fracture had the highest incidence in their study, but in the present study, the number of mandible fractures exceeded that of zygoma fractures. Significant damage to the eyeball was found in 15% of the cases and was always associated with vision loss. This study has a higher incidence of omnious damage to eyeball (15%) than that found by Rasool et al.
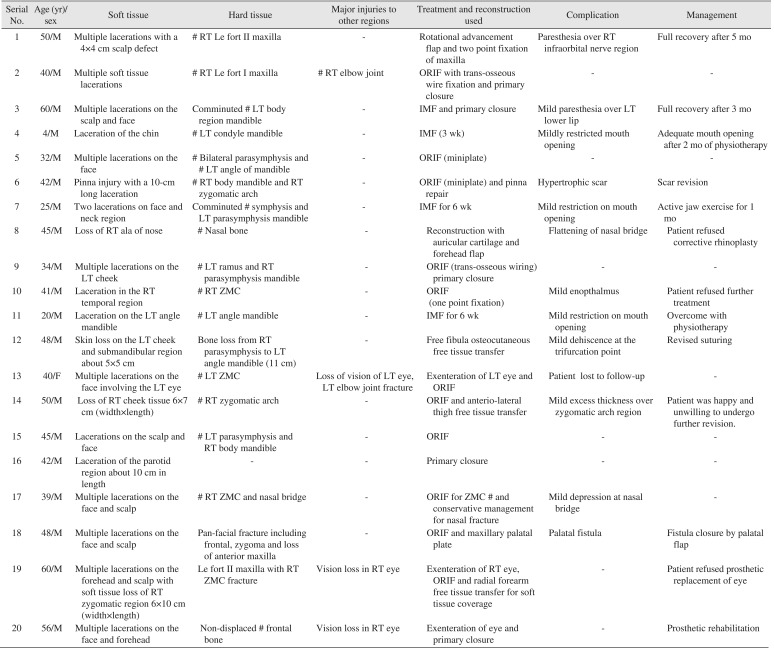
5 (8.87% of cases). Exenteration was performed as the treatment for injured viscera in all three cases. One case underwent the prosthetic rehabilitation of the enucleated eye, one was not willing to undergo any further intervention and one case was lost to follow-up. Treatment data for individual patients have been summarized in
Table 1.
Attacks by wild animals like bears are frequently associated with a significant percentage of tissue loss. Soft tissue injuries were managed by primary closure in 15 cases (75%), while 25% of cases required some sort of reconstructive procedure. A variety of flaps was utilized for the management of tissue losses in this study. Local and regional flaps can be used to cover small defects, but the fixed tissue yield and associated co-morbidity make these options suitable in certain limited cases, like scalp defect coverage by rotational flap in one of the cases from this study. Second, the presence of multiple lacerations in a local flap region also restricts the use of by virtue of compromised vascularity. In the case of regional flaps, a forehead flap with first stage cartilage grafting from the auricular cartilage for ala repair was successfully used and found to be reliable. Huang and Wong
8 used extraanatomic conchal cartilage, while Fell et al.
9 utilized rib cartilage for a similar purpose in their respective studies.
The use of free tissue transfers in bear attack cases has been reported for the first time in the authors' knowledge in this study. An anterio-lateral thigh (ALT) free flap, a radial forearm free flap (RFFF) and a fibula free tissue transfer were used for management of tissue loss in this study. ALT and RFFF provide good amounts of tissue for soft tissue reconstruction, and the selection of either depends on the size and thickness of the tissue required for the area of interest. Hazani et al.
10 reconstructed a scalp by a partial lateral thigh flap in a lion attack case, while an ALT flap was used for a cheek defect in this study.(
Fig. 1,
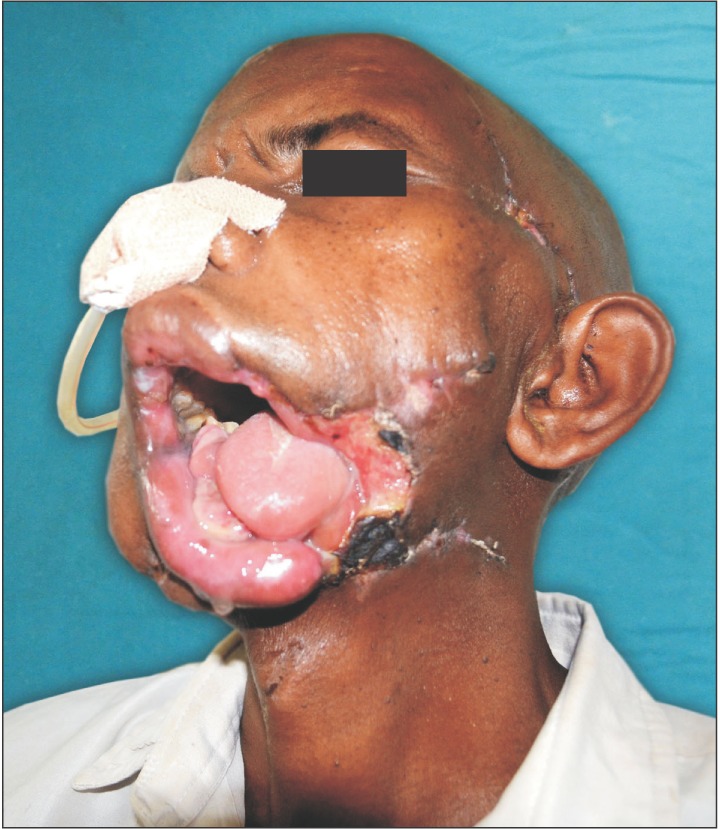
2) Except for the initial excess bulk that is reduced after several days, the ALT flap provides ample tissue for the coverage of wide areas requiring bulk such as the cheek. RFFF has been utilized for the mid-face area and defects in the peri-orbital region with satisfactory outcomes.(
Fig. 3,
4) RFFF, with its thin and pliable nature, provides an excellent option for mid-face, scalp and forehead reconstruction. When considering the reconstruction of composite defects, Govila et al.
11 in 1989 reported the use of a "rib sandwich" pectoralis major island flap in a bear attack case. They have recommended its use as a primary reconstructive option in cases of massive defects associated with a high risk of infection. Bony or composite defects have been reconstructed by fibula osteocutaneous free tissue transfer with good functional restoration.(
Fig. 5,
6) Now, with modern advances like micro-vascular techniques, the free tissue transfer can deliver better results with fewer complications and minimal donor site morbidity. Hence, this study favored free flaps as the treatment modality for tissue restoration.
As a general rule, the oral flora of the biting animal not only contains the usual "normal flora" but is also influenced by the micro-biome of their ingested prey and other foods
12. As the Asian black bear is mainly herbivorous, the chances of infection from bite wounds would be lower. Although some studies have reported a high incidence of infection in bear attack victims (34.4%)
13, none of the victims from the current study group developed infections or delayed wound healing. This can be explained by the rich blood supply to the face and the prophylactic use of broad-spectrum antibiotics in the study group, as suggested by previous studies
13. Minor complications like parotid fistulas may occur when the pre-auricular region is injured. We recommend intervention through duct ligation, which results in a successful outcome.
Due to the high intensity injuries and the involvement of complex areas like the head and neck in bear attacks, stepwise reconstructive surgery is required for better results. The financial burden and the number of operations required precipitate a lack of interest from victims in subsequent rehabilitation procedures. Motivational counseling towards treatment is of the utmost importance for the victims' well-being.
V. Conclusion
Maxillofacial injuries due to bear mauling may require staged reconstructive surgeries with symbiotic efforts of doctors and patients. Prophylactic use of broad-spectrum antibiotics minimizes the risk of infections drastically and should be followed as a routine protocol in the injury management. Although a large proportion of cases can be treated with simple procedures, a considerable number of cases (25%) require reconstructive surgery. The tissues to be replaced, the area to be reconstructed and the function to be restored are the three factors of prime importance in such maxillofacial injuries. The selection of different reconstructive options, including free tissue transfer and motivational counselling for rehabilitation, will provide better quality of life for bear mauling victims.
Fig. 1
Preoperative residual cheek defect.

Fig. 2
Anterolateral thigh flap used for cheek reconstruction.

Fig. 3
Soft tissue loss of mid-face and peri-orbital region.

Fig. 4
Radial forearm free flap for tissue coverage.

Fig. 5
Segmental defect of mandible with skin loss.
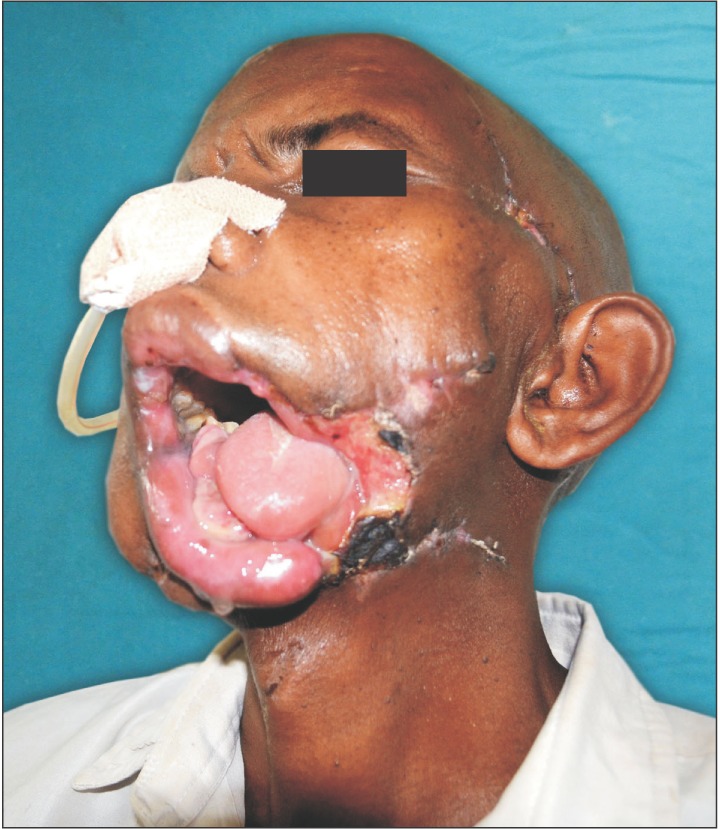
Fig. 6
Fibula osteocutaneous free flap of restoration of oral seal and function.

Table 1
Patient treatment data of the bear mauling cases
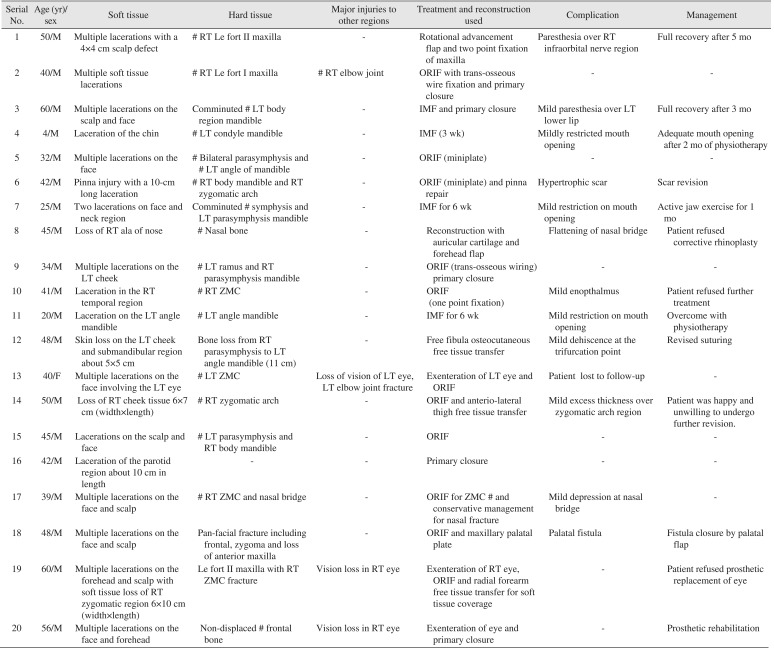
|
Serial No. |
Age (yr)/sex |
Soft tissue |
Hard tissue |
Major injuries to other regions |
Treatment and reconstruction used |
Complication |
Management |
|
1 |
50/M |
Multiple lacerations with a 4×4 cm scalp defect |
# RT Le fort II maxilla |
- |
Rotational advancement flap and two point fixation of maxilla |
Paresthesia over RT infraorbital nerve region |
Full recovery after 5 mo |
|
2 |
40/M |
Multiple soft tissue lacerations |
# RT Le fort I maxilla |
# RT elbow joint |
ORIF with trans-osseous wire fixation and primary closure |
- |
- |
|
3 |
60/M |
Multiple lacerations on the scalp and face |
Comminuted # LT body region mandible |
- |
IMF and primary closure |
Mild paresthesia over LT lower lip |
Full recovery after 3 mo |
|
4 |
4/M |
Laceration of the chin |
# LT condyle mandible |
- |
IMF (3 wk) |
Mildly restricted mouth opening |
Adequate mouth opening after 2 mo of physiotherapy |
|
5 |
32/M |
Multiple lacerations on the face |
# Bilateral parasymphysis and # LT angle of mandible |
- |
ORIF (miniplate) |
- |
- |
|
6 |
42/M |
Pinna injury with a 10-cm long laceration |
# RT body mandible and RT zygomatic arch |
- |
ORIF (miniplate) and pinna repair |
Hypertrophic scar |
Scar revision |
|
7 |
25/M |
Two lacerations on face and neck region |
Comminuted # symphysis and LT parasymphysis mandible |
- |
IMF for 6 wk |
Mild restriction on mouth opening |
Active jaw exercise for 1 mo |
|
8 |
45/M |
Loss of RT ala of nose |
# Nasal bone |
- |
Reconstruction with auricular cartilage and forehead flap |
Flattening of nasal bridge |
Patient refused corrective rhinoplasty |
|
9 |
34/M |
Multiple lacerations on the LT cheek |
# LT ramus and RT parasymphysis mandible |
- |
ORIF (trans-osseous wiring) primary closure |
- |
- |
|
10 |
41/M |
Laceration in the RT temporal region |
# RT ZMC |
- |
ORIF (one point fixation) |
Mild enopthalmus |
Patient refused further treatment |
|
11 |
20/M |
Laceration on the LT angle mandible |
# LT angle mandible |
- |
IMF for 6 wk |
Mild restriction on mouth opening |
Overcome with physiotherapy |
|
12 |
48/M |
Skin loss on the LT cheek and submandibular region about 5×5 cm |
Bone loss from RT parasymphysis to LT angle mandible (11 cm) |
- |
Free fibula osteocutaneous free tissue transfer |
Mild dehiscence at the trifurcation point |
Revised suturing |
|
13 |
40/F |
Multiple lacerations on the |
# LT ZMC |
Loss of vision of LT eye, LT elbow joint fracture |
Exenteration of LT eye and ORIF |
Patient lost to follow-up |
- |
|
14 |
50/M |
Loss of RT cheek tissue 6×7 cm (width×length) |
# RT zygomatic arch |
- |
ORIF and anterio-lateral thigh free tissue transfer |
Mild excess thickness over zygomatic arch region |
Patient was happy and unwilling to undergo further revision. |
|
15 |
45/M |
Lacerations on the scalp and face |
# LT parasymphysis and RT body mandible |
- |
ORIF |
- |
- |
|
16 |
42/M |
Laceration of the parotid region about 10 cm in length |
- |
- |
Primary closure |
- |
- |
|
17 |
39/M |
Multiple lacerations on the face and scalp |
# RT ZMC and nasal bridge |
- |
ORIF for ZMC # and conservative management for nasal fracture |
Mild depression at nasal bridge |
- |
|
18 |
48/M |
Multiple lacerations on the face and scalp |
Pan-facial fracture including frontal, zygoma and loss of anterior maxilla |
- |
ORIF and maxillary palatal plate |
Palatal fistula |
Fistula closure by palatal flap |
|
19 |
60/M |
Multiple lacerations on the forehead and scalp with soft tissue loss of RT zygomatic region 6×10 cm (width×length) |
Le fort II maxilla with RT ZMC fracture |
Vision loss in RT eye |
Exenteration of RT eye, ORIF and radial forearm free tissue transfer for soft tissue coverage |
- |
Patient refused prosthetic replacement of eye |
|
20 |
56/M |
Multiple lacerations on the face and forehead |
Non-displaced # frontal bone |
Vision loss in RT eye |
Exenteration of eye and primary closure |
- |
Prosthetic rehabilitation |




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download