Abstract
The detection of foreign bodies in the upper-aerodigestive tract is a fairly frequent event and can occur in various areas and for various reasons. In rare cases, foreign bodies can simulate a neoplasia. We evaluated similar cases during emergency regimen with an oral cavity mucosal lesion, causing lockjaw, sore throat, dysphagia, and swelling of the submandibular and laterocervical region. Physical examination revealed an extensive mucosal ulceration in the floor of the mouth and the lateral surface of the tongue, comparable to oral cancer. During a second, more accurate assessment, a partially deteriorated iron supplement tablet was found embedded in a mucosal pocket. After removing the tablet, gradual normalization of the tissue was observed without any sequelae. This is one of the many reasons why it is advisable and useful in cases of oral lesions to collect a detailed medical history and to perform an accurate clinical evaluation, including inspection and palpation of the lesion, before proceeding to further diagnostic assessments, especially in elderly patients taking many medications. However unlikely, it is possible that difficulty in swallowing pills or tablets could generate tumorlike lesions.
Go to : 
Ulcerative lesions are common oral mucosal disorders. The most frequent causes are mechanical and reactive factors, infectious diseases, and neoplasms, as well as autoimmune and hematological disorders. In all of these conditions, the main clinical feature is an ulcer, involving all epithelial layers with no tendency to heal.
Mucosal injuries of the gastrointestinal tract owing to therapeutic oral iron supplementation is commonly reported, yet underestimated1.
Injuries in the airways related to iron supplementation tablets have been documented in isolated case reports234 and small case series5.
A single case of iron supplementation tablet-induced mucosal injury of the hypopharynx has been described6, while similar cases involving the oral cavity have not been reported yet.
Foreign bodies embedded in the oral cavity are uncommon, due to the anatomical conformation of the mouth, even if some cases have been reported in dental literature. Most frequently, foreign bodies include dental materials, metallic projectiles, and pieces of glass7. The patient's presenting symptoms could include: oral pain, signs of local inflammation, painful swallowing, or a purulent discharge8. This paper describes a patient, treated for an iron deficiency anemia, with an ulcerative lesion similar to a squamous cell carcinoma of the oral cavity, but that was later identified as an inflammatory reaction to a tablet trapped in the floor of the mouth for multiple days.
Go to : 
An 83-year-old Caucasian woman was referred to the ENT (ear, nose, and throat) department from the emergency room, complaining of lockjaw, sore throat, dysphagia for three days, and a burning pain in the mouth.
The patient did not report any previous trauma, had no fever, and was not able to swallow anything, either solid or liquid. The symptoms decreased with painkillers but continued to worsen. Initially, her pharmacological history was believed to include only angiotensin-converting-enzyme inhibitors and oral antidiabetic drugs, as the patient forgot to mention the oral iron supplementation.
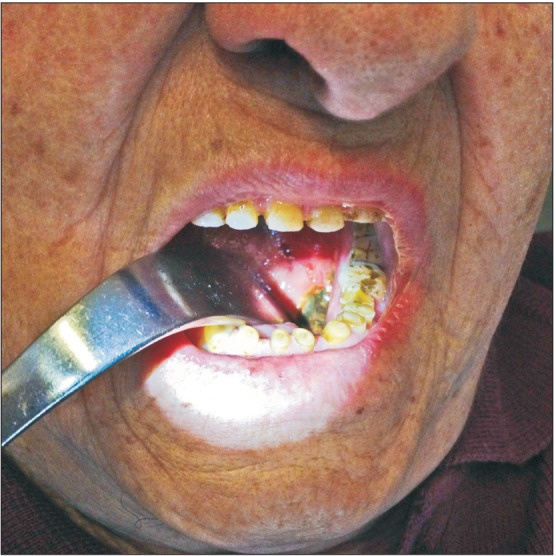
During the first evaluation, there was a painful swelling of the left side of the submandibular region, which extended to the ipsilateral upper laterocervical region. An ulceration with irregular margins, 1×2 cm in diameter, involving the floor of the mouth, the inferior gingiva, and the lateral surface of the tongue, was observed.(Fig. 1) The surrounding mucosa was healthy. An endoscopic examination of the upper airways did not show any other lesions.
Owing to a strong suspicion of a squamous cell carcinoma, a computed tomography (CT) scan and biopsy were scheduled. During a second examination (Fig. 2) including palpitation, part of a foreign body embedded in a mucosal pocket near the ulceration was felt and subsequently removed. The foreign body was an iron supplement tablet (dried ferrous sulphate) that the patient had not been able to swallow a few days earlier without realizing it.(Fig. 3) It was only after this discovery that the patient remembered to inform the physician about the oral iron supplementation that she had started six months previously for iron deficiency anemia.
After removal of the tablet, the symptoms gradually decreased; one week later, the size of the ulcerative lesion was considerably reduced and had completely disappeared about six weeks later with no sequelae.
Go to : 
Foreign bodies in the oral cavity are usually superficial and can be removed easily by a general practitioner, ENT specialist, or the patients themselves.
Foreign bodies that have been reported include: metal elements, dental materials, and a part of a toothbrush91011. Initially, these objects were mistaken for benign masses, as the foreign bodies did not produce any symptoms. The lack of symptoms is likely because biocompatible foreign bodies do not generate inflammation.
Nevertheless, some tablets, when embedded in the mouth, might mimic malignancy by causing swelling, neuralgic pain, or sub-mentum swelling as a result of releasing their active principle. Our patient had similar symptoms in the floor of her mouth.
When suspecting oral cavity carcinoma, factors such as smoking, alcohol, human papillomavirus, and dental trauma injuries should be evaluated. In our case, the patient's medical history was negative for any risk factors.
A complete history, including past medical, social, and family histories, is crucial for efficient diagnosis and treatment.
A complete physical as well as careful head and neck examination should be performed on all patients. A systematic visualization of all mucosae of the upper aerodigestive tract is indispensable due to the field cancerization phenomenon.
Palpation of the primary lesion in order to assess submucosal spread should always be performed12.
Aphthous and traumatic lesions are the most frequent ulcerations in the mouth; however, it is possible to see infectious ulcerations (tuberculous, syphilitic, common germs, or viruses), inflammatory diseases of the gastrointestinal tract, bullous dermatosis of autoimmune, toxic, or unknown origin such as erythema multi-form, and erosive lichen planus.
Furthermore, some lesions, like the traumatic ulcerative granuloma with stromal eosinophilia (TUGSE)13 and rare cases of adenoid cystic carcinoma14, could begin as a mouth ulcer.
In all these eventualities, the general context or evolution of the disease will allow an effective diagnosis, which could become more precise in certain cases by complementary investigations, biopsy in particular. When an ulceration is isolated, it is necessary to first exclude squamous cell carcinoma, as well as other malignant tumors, such as lymphomas and salivary glands cancers. Thus, it is imperative that the histological examination confirms the diagnosis in order to formulate a prognosis and begin treatment.
When there is an ulcerated lesion that does not tend to heal, it is always wise to perform a biopsy and plan a CT with contrast for further evaluation. In our case, the biopsy was not performed since the removal of the tablet determined the spontaneous healing of the lesion. If a biopsy of the lesion induced by the iron supplement tablet had been made, the presence of crystalline iron would have been observed thereby confirming the diagnosis of iron supplement tablet-induced mucosal injury6.
If held in the oral cavity, tablets can cause inflammation and ulceration of the mucosa via release of their active ingredients. Palpation of the lesion allowed detection of the tablet shape, and its removal is usually sufficient to resolve the symptoms. The damage is presumably caused by the oxidation of iron from the ferrous to the ferric form, resulting in toxic epithelial injury15.
This oral lesion case showed a unique localization (the mouth floor), clinical characteristics (lockjaw, dysphagia, burning pain, and sialorrhea), and features (tumor-like).
Thus, it is recommended in the case of oral lesions, to obtain a detailed medical history and to perform an accurate clinical evaluation before further examinations. However unlikely, it is possible that a difficulty in swallowing pills or tablets could generate tumor-like lesions.
Go to : 
References
1. Abraham SC, Yardley JH, Wu TT. Erosive injury to the upper gastrointestinal tract in patients receiving iron medication: an underrecognized entity. Am J Surg Pathol. 1999; 23:1241–1247. PMID: 10524525.
2. Clarke BE, Kim ST. Iron-induced bronchial injury. Histopathology. 2002; 41:472–473. PMID: 12405917.

3. Evrard C, Coffin O, Kaladji C, Brun J, Benard Y, Doumert J. Massive hemoptysis ten days after bronchial extraction of an accidentally inhaled tablet of ferrous sulfate. Ann Chir. 1991; 45:726–728. PMID: 1768033.
4. Godden DJ, Kerr KM, Watt SJ, Legge JS. Iron lung: bronchoscopic and pathological consequences of aspiration of ferrous sulphate. Thorax. 1991; 46:142–143. PMID: 2014497.

5. Raos M, Kovac K, Dodig S. Bronchial impairment of main bronchus by aspiration of ferrous sulphate tablet. Lijec Vjesn. 2004; 126:194–196. PMID: 15754788.
6. Cimino-Mathews A, Broman JH, Westra WH, Illei PB. Iron pill-induced tumefactive mucosal injury of the hypopharynx. Am J Surg Pathol. 2010; 34:1720–1722. PMID: 20975344.

7. Arora BK, Ruprecht A. Foreign body in tongue. Oral Surg Oral Med Oral Pathol. 1978; 45:823–825. PMID: 276800.

8. Price C, Whitehead FI. Impression materials as foreign bodies. Br Dent J. 1972; 133:9–14. PMID: 4507102.

9. Lin CJ, Su WF, Wang CH. A foreign body embedded in the mobile tongue masquerading as a neoplasm. Eur Arch Otorhinolaryngol. 2003; 260:277–279. PMID: 12750919.

10. Sathish R, Suhas S, Gayathri G, Ravikumar G, Chandrashekar L, Omprakash TL. Embedded toothbrush foreign body in cheek: report of an unusual case. Eur Arch Paediatr Dent. 2011; 12:272–274. PMID: 21993069.
11. McKinney RV Jr, Brady GL, Singh BB. Metallic foreign body embedded in the cheek for 20 years. J Am Dent Assoc. 1981; 102:331–333. PMID: 7007469.

12. Seikaly H, Rassekh CH. Oropharyngeal cancer. In : Bailey BJ, Johnson JT, Newlands SD, editors. Head and neck surgery: otolaryngology. 4th ed. Philadelphia: Lippincott Williams & Wilkins;2006. p. 1674–1690.
13. Kwon JI, Kim HW, Nam W, Cha IH, Kim HJ. Traumatic ulcerative granuloma misjudged as oral squamous cell carcinoma (SCC) on the buccal cheek: case report. J Korean Assoc Oral Maxillofac Surg. 2010; 36:217–220.

14. Khan S, Agwani K, Bhargava P, Kumar SP. Adenoid cystic carcinoma presenting as an ulcer on the floor of the mouth: a rare case report. J Korean Assoc Oral Maxillofac Surg. 2014; 40:253–257. PMID: 25368840.

15. Aruoma OI, Halliwell B. Superoxide-dependent and ascorbate-dependent formation of hydroxyl radicals from hydrogen peroxide in the presence of iron. Are lactoferrin and transferrin promoters of hydroxyl-radical generation? Biochem J. 1987; 241:273–278. PMID: 3032157.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download