Abstract
Maxillary transverse deficiency is one of the most common deformities among occlusal discrepancies. Typical surgical methods are segmental Le Fort I osteotomy and surgically-assisted rapid maxillary expansion (SARME). This patient underwent a parasagittal split with a Le Fort I osteotomy to correct transverse maxillary deficiency. During follow-up, early transverse relapse occurred and rapid maxillary expansion (RME) application with removal of the fixative plate on the constricted side was able to regain the dimension again. RME application may be appropriate salvage therapy for such a case.
Maxillary transverse deficiency with posterior crossbite is one of the most common dentofacial deformities. Orthodontic treatment such as rapid palatal expansion (RPE) and rapid maxillary expansion (RME) are widely used to correct the problem1. After completion of skeletal maturation, palatal expansion without surgery causes more dentoalveolar movement than bony displacement. This can lead to many problems, including extrusion of the molars and periodontal complications2. Therefore, combined surgical and orthodontic treatment is more effective and safe for the correction of transverse discrepancies in adults3.
The segmental Le Fort I osteotomy and surgically-assisted rapid maxillary expansion (SARME) are the most commonly used surgical methods to treat transverse discrepancy. Although many studies have reported short-term stability surgical outcomes, few data support long-term stability. However, most studies reported that SARME is more stable and has lower morbidity in complications than segmental osteotomy1.
In our case, a Le Fort I osteotomy with paramedian split was performed on an adult patient to expand the maxillary transverse dimension and skeletal class III facial deformity. However, the patient experienced maxillary constriction shortly after the operation. This patient's maxillary constriction was successfully recovered with an RME device after a Le Fort I osteotomy with paramedian split.
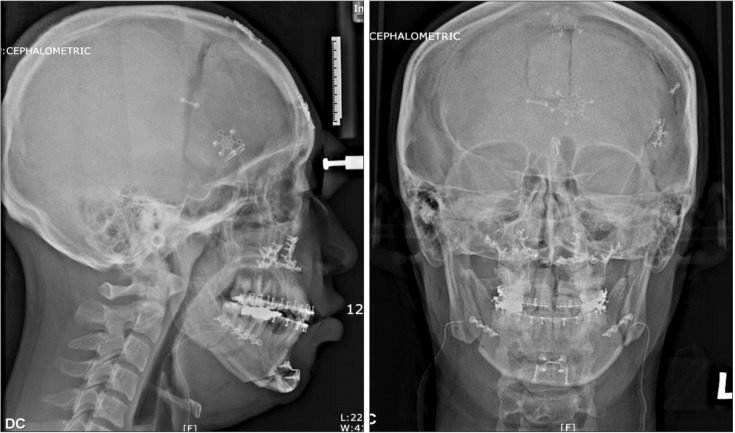
A male patient in his mid-twenties visited our orthodontic department with the chief complaint of mandibular prognathism with a maxillary bilateral crossbite and tooth crowding through a high, narrow palate.(Fig. 1) Aligning and leveling were performed during presurgical orthodontics. The horizontal discrepancy of the posterior molars with the crossbite was noted in the maxillary dental arch.(Fig. 2) Parasagittal splitting with a Le Fort I osteotomy for maxillary transverse deficiency and bisagital split ramus osteotomy (BSSRO) with genioplasty were performed to treat mandibular prognathism and maxillary transverse deficiency.(Fig. 3) The patient was transferred to the orthodontic department for postsurgical orthodontic treatment 6 weeks postoperatively. Loss of horizontal width and crossbite on the right side molars were observed after removal of the surgical wafer. The wafer on the affected side which had a crossbite was removed after the cut between the right maxillary canine and the first premolar. The rest of the wafer was placed and intermaxillary fixation was performed afterwards.(Fig. 4) A week later, an RME device was inserted and fixative plates were removed on the right side. Activation was performed twice a day with a daily expansion rate of 0.5 mm until the necessary expansion was achieved. The RME device was left in place for 4 months as a fixed retainer, which was replaced with a transpalatal retainer for further retention.(Fig. 5) The palatal transverse width was successfully increased and the correction of posterior crossbite was achieved.(Fig. 6) We did not observe complications or relapse during 3 years of follow-up, and the occlusion has remained stable.(Fig. 7)
Surgical procedures such as SARME and the Le Fort I osteotomy have been reported to be an effective treatment to correct transverse maxillary deficiency in adults. However, indications for these procedures remain controversial4. Vandersea et al.1 reported that the SARME technique is indicated in cases with a deficit of 7 mm or more who also have isolated transverse deficiency not required correction in the vertical or sagittal plane. Segmental Le Fort I osteotomy can be applied in patients who have a transverse deficiency of less than 7 mm that also require vertical or sagittal repositioning of the maxilla. We treated a skeletally mature patient with transverse maxillary deficiency with a para-sagittal split and a Le Fort I osteotomy. However, six weeks after surgery, we observed a relapse in the crossbite of the right molars.
In our case study, the short retention period may have caused the immediate relapse. However, relapse of the transverse expansion may be attributed to many causes. First, mechanical resistance from circummaxillary sutures could be a factor. According to Isaacson and Ingram5, maxillary articulations, which are adjacent to the midpalatal suture, are the main points of resistance to expansion of the maxilla. This finding is inconsistent with previous studies insisting that the midpalatal suture is the main cause of resistance to expansion of force. Lines6 insisted that facial skeletal resistance to expansion came from zygomaticotemporal, zygomaticofrontal, and zygomaticomaxillary sutures. Koudstaal et al.7 reviewed previous studies indicating that the zygomaticomaxillary junction was the major site of resistance. This suggests that the parasagittal osteotomy alone cannot guarantee sufficient expansion.
Many studies reported a higher relapse rate after segmental Le Fort I osteotomy than after SARME. We chose the Le Fort I osteotomy technique because the patient required 3 mm of transverse expansion and vertical repositioning to correct asymmetry. Proffit et al.8 performed segmental Le Fort I osteotomy and found a 0.1 mm relapse in intercanine teeth in 5% of patients and a 2 mm relapse in intermolar teeth in 50% of patients. Phillips et al.9 reported a relapse rate of 49% in molars and 30% in premolars after Le Fort I and segmental osteotomy, followed by orthodontic treatment in 39 patients. However, according to a study using a Reflex microscope on dental casts, the relapse rates between Le Fort I with orthodontic expansion and multisegment Le Fort I osteotomies were not significantly different10. Kretschmer et al.11 studied surgical expansion of the maxilla and found high relapse rates in the dentoalveolar portion suggesting that orthodontic relapse matters in these cases. Although the resisting pillars in the zygomatico-maxillary area were released via surgical methods, tough palatal mucosa would limit surgical expansion.
The relapse rate of SARME was reported as 5%-25% in various papers. Pogrel et al.12 reported that patients with 1 year of orthodontic treatment after the surgery showed an 11.8% relapse rate in the first molar. Bays and Greco13 retrospectively evaluated 19 patients more than 6 months after removal of orthodontic appliances, and reported mean relapse rates of 8.8% in the intercuspids and 7.7% in intermolar expansion. Northway and Meade14 also reported a 4% relapse rate with 0.2 mm of intercanine distance and a 3% relapse rate with 0.2 mm of intermolar distance. They concluded that SARME achieved excellent stability which does not require overcorrection. Berger et al.15 insisted that SARME could correct transverse discrepancies with minimal relapse.
Third, previous studies recommended over-expansion and longer retention periods to prevent relapse. In our case, the retention period was 6 weeks, which is shorter than the recommendation. Moreover, overexpansion was not considered. The retention period following the expansion of dento-osseous segments plays a significant role in preventing relapse1. An occlusal splint should be placed at the mid-palatal osseotomies as a retainer where bone begins to fill the space at least 6 weeks after surgery. The relapse rate with a 6-month stabilization period16 was lower than the relapse rate with a 3-month stabilization period3. Pogrel et al.12 recommended that retention should be maintained for at least 3 months until the palatal gap is filled by bone tissue, whereas Phillips et al.9 reported that only a 6-week period would be required for retention. The length of the retention period is a controversial issue in the literature. Petrick et al.17 investigated the bone density of the midpalatal suture 7 months after SARME in adults and showed that the density achieved was only 1/2 to 3/4 of the pretreatment value. They reported that retention periods after SARPE should be lengthened to prevent relapse.
In our case, the surgical wafer was maintained for 6 weeks and transverse relapse occurred almost immediately after wafer removal. This relapse can be explained by the short retention period, and could have been prevented by a longer retention period. The retention period after transverse gain in adult patients should be at least 3 months18, and lengthening of the retention period is recommended when it is critical to maintain arch width. Phillips et al.9 suggested that overexpansion of 2 to 3 mm should be performed to prevent relapse.
Based on the literatures, correction of transverse maxillary deficiency seems to be one of the least stable surgical movements. However, this shortcoming can be overcome with forthcoming advances, and an RME application may be a good option for treating early relapse of maxillary transverse expansion. For long-term stability, the proper retention period also should be considered on a case-by-case basis.
References
1. Vandersea BA, Ruvo AT, Frost DE. Maxillary transverse deficiency: surgical alternatives to management. Oral Maxillofac Surg Clin North Am. 2007; 19:351–368. PMID: 18088890.
2. Sokucu O, Kosger HH, Bicakci AA, Babacan H. Stability in dental changes in RME and SARME: a 2-year follow-up. Angle Orthod. 2009; 79:207–213. PMID: 19216605.

3. Byloff FK, Mossaz CF. Skeletal and dental changes following surgically assisted rapid palatal expansion. Eur J Orthod. 2004; 26:403–409. PMID: 15366385.

4. Silverstein K, Quinn PD. Surgically-assisted rapid palatal expansion for management of transverse maxillary deficiency. J Oral Maxillofac Surg. 1997; 55:725–727. PMID: 9216505.

5. Isaacson RJ, Ingram AH. Forces produced by rapid maxillary expansion II: forces present during treatment. Angle Orthod. 1964; 34:261–270.
6. Lines PA. Adult rapid maxillary expansion with corticotomy. Am J Orthod. 1975; 67:44–56. PMID: 803165.

7. Koudstaal MJ, Poort LJ, van der Wal KG, Wolvius EB, Prahl-Andersen B, Schulten AJ. Surgically assisted rapid maxillary expansion (SARME): a review of the literature. Int J Oral Maxillofac Surg. 2005; 34:709–714. PMID: 15961279.

8. Proffit WR, Turvey TA, Phillips C. Orthognathic surgery: a hierarchy of stability. Int J Adult Orthodon Orthognath Surg. 1996; 11:191–204. PMID: 9456622.
9. Phillips C, Medland WH, Fields HW Jr, Proffit WR, White RP Jr. Stability of surgical maxillary expansion. Int J Adult Orthodon Orthognath Surg. 1992; 7:139–146. PMID: 1291607.
10. Hoppenreijs TJ, van der Linden FP, Freihofer HP, Stoelinga PJ, Tuinzing DB, Jacobs BT, et al. Stability of transverse maxillary dental arch dimensions following orthodontic-surgical correction of anterior open bites. Int J Adult Orthodon Orthognath Surg. 1998; 13:7–22. PMID: 9558532.
11. Kretschmer WB, Baciut G, Baciut M, Zoder W, Wangerin K. Transverse stability of 3-piece Le Fort I osteotomies. J Oral Maxillofac Surg. 2011; 69:861–869. PMID: 21050640.

12. Pogrel MA, Kaban LB, Vargervik K, Baumrind S. Surgically assisted rapid maxillary expansion in adults. Int J Adult Orthodon Orthognath Surg. 1992; 7:37–41. PMID: 1453038.
13. Bays RA, Greco JM. Surgically assisted rapid palatal expansion: an outpatient technique with long-term stability. J Oral Maxillofac Surg. 1992; 50:110–113. PMID: 1732482.

14. Northway WM, Meade JB Jr. Surgically assisted rapid maxillary expansion: a comparison of technique, response, and stability. Angle Orthod. 1997; 67:309–320. PMID: 9267580.
15. Berger JL, Pangrazio-Kulbersh V, Borgula T, Kaczynski R. Stability of orthopedic and surgically assisted rapid palatal expansion over time. Am J Orthod Dentofacial Orthop. 1998; 114:638–645. PMID: 9844202.

16. Anttila A, Finne K, Keski-Nisula K, Somppi M, Panula K, Peltomäki T. Feasibility and long-term stability of surgically assisted rapid maxillary expansion with lateral osteotomy. Eur J Orthod. 2004; 26:391–395. PMID: 15366383.

17. Petrick S, Hothan T, Hietschold V, Schneider M, Harzer W, Tausche E. Bone density of the midpalatal suture 7 months after surgically assisted rapid palatal expansion in adults. Am J Orthod Dentofacial Orthop. 2011; 139(4 Suppl):S109–S116. PMID: 21435528.

18. Bailey LJ, White RP Jr, Proffit WR, Turvey TA. Segmental LeFort I osteotomy for management of transverse maxillary deficiency. J Oral Maxillofac Surg. 1997; 55:728–731. PMID: 9216506.

Fig. 1
Intraoral photos and radiographs (cephalometric and posteroanterior view) at the initial visit. We observed a maxilla with a narrow, high vault palate, maxillary bilateral crossbite, and teeth crowding through the relatively narrow maxilla compared to the mandible.
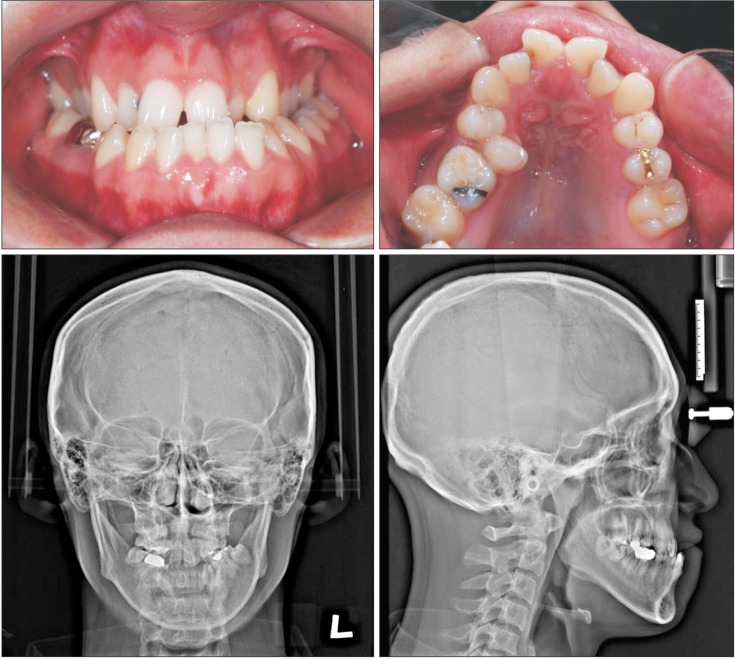
Fig. 4
Removal of the surgical wafer precipitated immediate transverse relapse, and the surgical wafer was trimmed out in the constricted side to allow re-expansion.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download