Abstract
Objectives
To assess the validity of the vertical tube-shift method using intraoral periapical radiography (IOPAR) for determining the relationship between the mandibular third molar roots and the inferior alveolar nerve (IAN) canal in comparison with cone-beam computed tomography (CBCT).
Materials and Methods
Fifty impacted mandibular third molars were analyzed using the IOPAR vertical tube-shift method and CBCT. The relationship of the IAN canal to the impacted mandibular third molar was recorded as buccal, lingual or in line with the apex and was compared with CBCT findings. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the vertical tube-shift method in depicting the relationship (buccal/lingual/in line with the apex) of the IAN canal to the third molar root apex was calculated.
Results
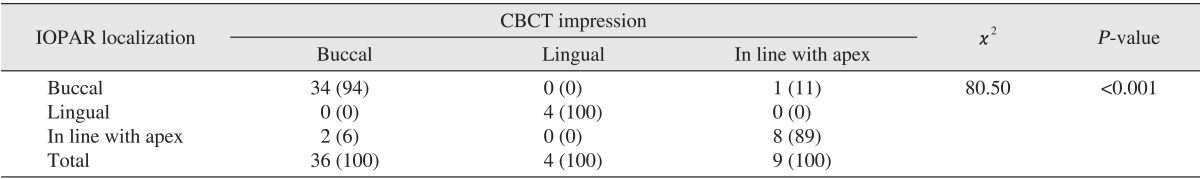
The sensitivity and specificity PPV and NPV of the IOPAR vertical tube-shift technique was found to be highest for a lingual relationship (100%) followed by buccal (94.4%, 92.3%, 97.1%, and 85.7%) and in line with the apex relationship (88.9%, 95.0%, 80.0%, and 97.4%) of the IAN canal with the third molar root apex, respectively. A statistically significant association was observed between the IOPAR vertical tube-shift method and the CBCT with a P-value <0.01.
Third molars have a high incidence of impaction and are associated with conditions such as pericoronitis, caries on the distal surface of the second molar, pain, external root resorption, and odontogenic cysts or tumors1, which often necessitate their surgical removal.
The surgical removal of impacted mandibular third molars is often associated with inferior alveolar nerve (IAN) damage, the incidence of which is reported to be 0.4%-8.4%2,3,4,5. To protect the nerve from mechanical injury during surgery, it is important to clearly assess the relative positions of the nerve and the root tip preoperatively3.
The complete radiographic assessment of impacted mandibular third molars includes morphology, its approximation to the IAN canal and its bucco-lingual position. The most commonly used radiographic methods are intraoral periapical radiography (IOPAR) and panoramic radiography (orthopantomography, OPG). These methods depict the IAN canal using superio-inferior and anterio-posterior relationships, but the bucco-lingual relationship or depth cannot be assessed. Computed tomography (CT) and cone-beam CT (CBCT) are excellent methods for localizing the IAN canal and its relationship to the lower third molar roots. CBCT images can be generated through the mandibular body in any plane6. However, owing to the cost, limited availability and radiation dose, CBCT is usually not the first radiographic technique of choice for a preoperative radiographic evaluation of lower impacted third molars7.
Localization techniques using conventional radiography can be used to assess the bucco-lingual dimension. Jaju8 and Morant et al.9 stressed the importance of assessing the relationship of the IAN canal to the third molar root apex buccolingually8,9,10. They suggested the use of Richard's vertical tube shift technique for localizing the IAN canal to the third molar root apex. The vertical tube-shift method uses two IOPARs taken at different vertical angulations to delineate the buccolingual relationship of the IAN canal to the mandibular third molar root apices. It is easily accessible, cost effective and has less radiation exposure.
The purpose of this study was to validate the vertical tube-shift method in determining the relationship between the impacted mandibular third molar roots and the IAN canal.
The preoperative IOPARs taken at 0° and -20° angulations and CBCT images of 50 impacted mandibular third molars of patients visiting the Department of Oral Medicine and Radiology from December 2012 to July 2014, The Oxford Dental College (Bangalore, India) were selected for the study. Ethical clearance was granted from The Oxford Dental College' s institutional review committee, and informed consent was obtained from all patients willing to participate in the present study.
The inclusion criteria were 0-degree IOPARs of patients showing any one of the following signs of a close relationship of the mandibular third molar root to the IAN canal: (1) darkening of the root, (2) narrowing of the IAN canal, (3) diversion of the IAN canal, or (4) interruption of the superior cortical line of the IAN canal. Patients not showing any close relationship between impacted mandibular third molar roots and the IAN canal on 0-degree IOPAR and patients with neuromuscular disorders were excluded.
Two IOPARs of impacted mandibular third molars were made using Richard's vertical tube-shift method10. An intraoral dental X-ray machine (BEST-X-DC; Toshiba Medical System Corp., Tokyo, Japan) at 70 kVp, 10 mA, and 0.7 seconds was used along with intraoral Kodak Ultra speed films of size 2 (31×41 mm), E-speed (Kodak H, New York, NY, USA).
The first IOPAR was made by directing the position indicating device (Fig. 1) at 0° vertical angulation. If any sign of a close relationship to the IAN canal was observed, a second IOPAR was taken by directing the position-indicating device at a vertical angulation of -20°. The processed radiographs were traced on the tracing paper.
The relationship of the IAN canal to an impacted mandibular third molar as determined by vertical tube-shift method was recorded as follows: (1) Buccal, if the IAN canal appeared to move upwards in relation to the root apex of the impacted mandibular third molar in the IOPAR taken at -20° vertical angulations as compared to IOPAR taken at 0° vertical angulations.(Fig. 2. A); (2) Lingual, if the IAN canal appeared to move downwards in relation to the root apex of the impacted mandibular third molar in IOPAR taken at -20° vertical angulations as compared to IOPAR taken at 0° vertical angulations.(Fig. 3. A); (3) In line with the apex, if no change was observed in the IAN canal position in relation to the root apex of the impacted mandibular third molar in IOPAR taken at -20° vertical angulations as compared to IOPAR taken at 0° vertical angulations.(Fig. 4. A)
CBCT examination (CS 9300; Kodak Carestream, Atlanta, GA, USA) was performed with 90 kVp, 10 mA, 20 seconds as exposure parameters, and cross-sectional images of the mandibular third molar region (Fig. 2. B, 3. B, 4. B) were recorded.
The relationship as determined by the vertical tube-shift method was further compared with the CBCT images. Statistical analyses were performed with the SPSS version 16.0 (SPSS Inc., Chicago, IL, USA). Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated using CBCT as the gold standard. A chi-square test was performed to evaluate the association between IOPAR localization and the CBCT impression results.
Out of our sample size of 50 cases, 49 cases were considered for statistical analysis and one case was excluded as the patient appeared to have three roots in CBCT. The IAN canal presented buccal in 35 cases, lingual in four cases, and in line with the apex of the third molar root in 10 cases using the IOPAR vertical tube-shift method. For CBCT, the canal was buccal in 36 cases, lingual in four cases and in line with the apex in nine cases. A chi-square test revealed a statistically significant association between IOPAR localization and the CBCT impression results with a P-value<0.001.(Table 1)
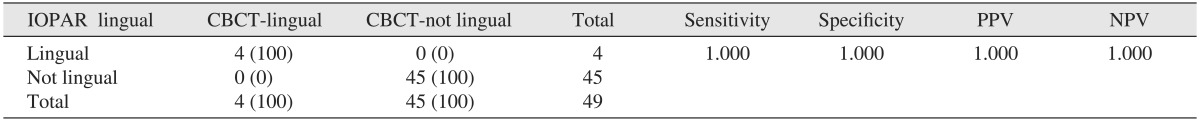
The sensitivity, specificity, PPV, and NPV of the IOPAR vertical tube-shift method was found to be 94.4%, 92.3%, 97.1%, and 85.7%, respectively, in localizing the IAN canal buccal to root apex of the third molar tooth as compared to CBCT.(Table 2) For localizing the IAN canal lingual to the root apex of the third molar tooth, the sensitivity, specificity, PPV, and NPV of the IOPAR vertical tube-shift method was 100% compared to CBCT.(Table 3)
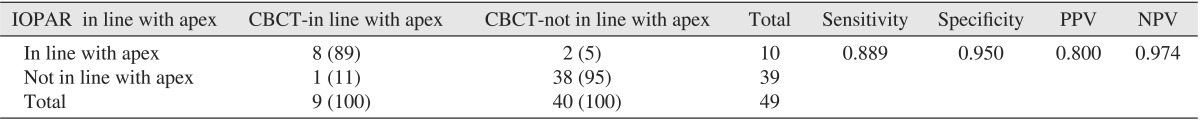
Sensitivity, specificity, PPV, and NPV value of the IOPAR vertical tube-shift method was found to be 88.9%, 95.0%, 80.0%, and 97.4%, respectively, at localizing the IAN canal in line with the root apex of the third molar tooth as compared to CBCT.(Table 4)
The preoperative assessment of the third molar root apex and the IAN canal can be done using conventional radiographs as well as advanced imaging modalities, including CBCT and CT. In oral and maxillofacial surgery practice, OPG is the most widely used technique for evaluating the lower third molar position and its relationship with the IAN canal6. Several clinical studies have determined specific radiographic signs, such as darkening of the root, narrowing or diversion of the IAN canal and interruption of the superior cortical line of the IAN canal wall, being highly suggestive of the close proximity between the lower third molars and the IAN canal1,2,3,6,11,12.
OPG has several projection-geometric limitations that may decrease its accuracy. It only provides information regarding the position of the IAN canal in the vertical plane. OPG has variable magnification, and lingual-positioned structures are projected upward, producing a sharp image layer (focal trough) of limited width. Moreover, the IAN canal is frequently positioned at the periphery of this focal trough, located buccal or lingually2.
On the other hand, CBCT provides better three-dimensional images, which show the relationship between the third molar roots and all adjacent structures with a high resolution4. Considering the high cost, limited availability, and higher radiation exposure, CBCT is usually not the first radiographic technique of choice for all impacted lower third molars. Moreover, not all CBCT devices are alike. For example, the variation in resolution might affect the outcomes, and the results with one CBCT system cannot necessarily be generalized to all CBCT systems. Heurich et al.13 were able to reconstruct the course of the IAN canal exactly with the help of CBCT (New Tom, Marburg, Germany) in only 75 cases out of 81 cases (93%) before lower third molar extractions. In a study by Neugebauer et al.3 the vertical and horizontal position of the root tip of the third molars relative to the IAN canal could not be precisely identified in 1% and 2.8% of the CBCT examinations, respectively. In another study, 3D Accuitomo CBCT was reported to give a high sensitivity (93%) with a specificity of 77% in predicting exposure of the neurovascular bundle11.
In comparison with advanced imaging modalities, IOPARs are readily available at any basic dental set-up and provide excellent image details when performed efficiently. They involve minimum risk of exposure to ionizing radiation and are cost-effective. With the vertical tube-shift method, the precise location of the IAN canal with respect to third molar roots can be assessed.
No previous studies have validated the vertical tube shift method for establishing the bucco-lingual relationship of the IAN canal with respect to the lower third molars. Until now, only two studies have assessed the performance of the vertical tube shift method in localizing the IAN canal bucco-lingually to third molar root apices. In 2010, Kositbowornchai et al.6 reported the performance of the shift tube method in comparison with CBCT in identifying this relationship. The aim was to compare the ability of two radiographic methods: the OPG in combination with a -20° angle IOPAR versus two IOPARs at 0° and -20°. Another study was reported by Jasa et al.14 in 2014 and evaluated the use of lateral oblique radiography at two different angles (0° and -30°) for the buccolingual topographic localization of the IAN canal with respect to the lower third molars.
In our study, a buccal relationship of the IAN canal to the lower third molar root apex was found to be present in 35 cases by the IOPA vertical tube-shift method as compared to 36 cases on CBCT. The sensitivity, specificity, PPV, and NPV of the vertical tube-shift method for buccal relation was calculated as 94.4%, 92.3%, 97.1%, and 85.7%, respectively. In contrast, the study by Kositbowornchai et al.6 reported a much lower sensitivity (85.7%) and specificity (38.9%), which included only 14 buccal placed IAN canals. Jasa et al.14 reported similar results as those found in our study, such as sensi tivity (91.3%), specificity (91.7%), PPV (95.8%), and NPV (85.7%).
The studies by Kositbowornchai et al.6 and Jasa et al.14 as well as the present study reported a sensitivity, specificity, PPV, and NPV of the vertical tube-shift method as 100% for lingual relationships. These two previous studies had a minimal number of lingual placed IAN canals 2 and 3. Even in our study, a lingual placed IAN canal was present only in four cases. This small incidence could be because of a lower prevalence of lingual-placed IAN canals to the third molar root apex15.
Ten cases had an in line with apex relationship of the IAN canal to the lower third molar root apex by the IOPA vertical tube-shift method as compared to nine cases on CBCT. The sensitivity, specificity, PPV, and NPV of the vertical localization technique for the in line with apex relation was calculated as 88.9%, 95.0%, 80.0%, and 97.4%, respectively, whereas a 31.3% sensitivity and an 81.3% specificity was reported by Kositbowornchai et al.6 as they evaluated 16 in line with apex IAN canals in their study. In Jasa et al.'s study14, the sensitivity, specificity, PPV, and NPV were reported to be 88.9%, 92.3%, 96.3%, and 81.8%. This similarity was found to be nearly correlated with our study results.
The difference in results between the present study and Kositbowornchai et al.6 could be attributed to the involvement of two observers in their study and also to the images being interpreted twice.
In the present study, among buccal and in line with apex relations, the probability of diagnosing the IAN canal buccal to the third molar root apex (i.e., the sensitivity) was more than in line with apex. At the same time, the probability of the IAN canal not being in line with the apex (i.e., specificity) is 3% more than not being buccal to the third molar root apex.
PPV was found to be highest for lingual relation followed by buccal and in line with apex, whereas NPV was highest for lingual relation followed by in line with apex and buccal, respectively. Therefore, the precision of diagnosing an IAN canal as not being in line with the apex requires more than simply not being buccal.
For the vertical tube-shift method to be efficient, the change in vertical angulation parameter must be followed. In order to observe the apparent movement of the IAN canal in the radiographic image, it is necessary to change the vertical angle sufficiently as the distance between the IAN canal and the third molar is less or they might be superimposed. In our study, -20° vertical angulations for IOPA were found to be adequate to interpret the images. In contrast, Jasa et al.14 stressed that the vertical angle should be changed to a minimum of -30°. This desired alteration could be because of the lateral oblique radiograph used in their study, which can be associated with image distortion or magnification.
Overall, Kositbowornchai et al.'s study6 commented that a panoramic radiograph with vertical periapical tube shift and two different vertical angulation periapical radiographs provided a high potential for detecting the closeness of the relationship of the third molar root and the IAN canal. In contrast, Jasa et al.14 stressed that lateral oblique radiographs taken at 0° and -30° may be successfully used to determine the bucco-lingual relationship between the mandibular canal and the lower third molar.
The present study showed that the IOPA vertical tube-shift method can be relied upon at par with CBCT to assess the relationship of the IAN canal to the lower third molar root apex. A -20° tube shift is sufficient to apply Richard's technique for localization of the IAN canal with the third molar root apex.
References
1. Neves FS, Souza TC, Almeida SM, Haiter-Neto F, Freitas DQ, Bóscolo FN. Correlation of panoramic radiography and cone beam CT findings in the assessment of the relationship between impacted mandibular third molars and the mandibular canal. Dentomaxillofac Radiol. 2012; 41:553–557. PMID: 22282507.

2. Szalma J, Lempel E, Jeges S, Szabó G, Olasz L. The prognostic value of panoramic radiography of inferior alveolar nerve damage after mandibular third molar removal: retrospective study of 400 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:294–302. PMID: 19846324.

3. Neugebauer J, Shirani R, Mischkowski RA, Ritter L, Scheer M, Keeve E, et al. Comparison of cone-beam volumetric imaging and combined plain radiographs for localization of the mandibular canal before removal of impacted lower third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 105:633–642. PMID: 18299225.

4. Tantanapornkul W, Okochi K, Bhakdinaronk A, Ohbayashi N, Kurabayashi T. Correlation of darkening of impacted mandibular third molar root on digital panoramic images with cone beam computed tomography findings. Dentomaxillofac Radiol. 2009; 38:11–16. PMID: 19114418.

5. Marciani RD. Third molar removal: an overview of indications, imaging, evaluation, and assessment of risk. Oral Maxillofac Surg Clin North Am. 2007; 19:1–13. PMID: 18088860.

6. Kositbowornchai S, Densiri-aksorn W, Piumthanaroj P. Ability of two radiographic methods to identify the closeness between the mandibular third molar root and the inferior alveolar canal: a pilot study. Dentomaxillofac Radiol. 2010; 39:79–84. PMID: 20100918.

7. Akçiçek G, Uysal S, Avcu N, Kansu Ö. Comparison of different imaging techniques for the evaluation of proximity between molars and the mandibular canal. Clin Dent Res. 2012; 36:2–7.
8. Jaju PP. Localization of mandibular canal by buccal object rule. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:799. PMID: 20451840.

9. Morant RD, Eleazer PD, Scheetz JP, Farman AG. Array-projection geometry and depth discrimination with Tuned-Aperture Computed Tomography for assessing the relationship between tooth roots and the inferior alveolar canal. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 91:252–259. PMID: 11174606.

10. Richards AG. Roentgenographic localization of the mandibular canal. J Oral Surg (Chic). 1952; 10:325–329. PMID: 12991124.
11. Tantanapornkul W, Okouchi K, Fujiwara Y, Yamashiro M, Maruoka Y, Ohbayashi N, et al. A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:253–259. PMID: 17234544.

12. Shahidi S, Zamiri B, Bronoosh P. Comparison of panoramic radiography with cone beam CT in predicting the relationship of the mandibular third molar roots to the alveolar canal. Imaging Sci Dent. 2013; 43:105–109. PMID: 23807934.

13. Heurich T, Ziegler C, Steveling H, Wörtche R, Mühling J, Hassfeld S. Digital volume tomography--an extension to the diagnostic procedures available for application before surgical removal of third molars. Mund Kiefer Gesichtschir. 2002; 6:427–432. PMID: 12447656.
14. Jasa GR, Vizzotto MB, Silveira PF, Silveira HE, Silveira HL, Correa LR, et al. Buccal-lingual localization of the mandibular canal in relationship with the third molar using the lateral oblique technique. J Oral Maxillofac Radiol. 2014; 2:15–20.

15. Miller CS, Nummikoski PV, Barnett DA, Langlais RP. Crosssectional tomography. A diagnostic technique for determining the buccolingual relationship of impacted mandibular third molars and the inferior alveolar neurovascular bundle. Oral Surg Oral Med Oral Pathol. 1990; 70:791–797. PMID: 2263343.
Fig. 1
Intraoral periapical radiography exposure was made by directing the position-indicating device at 0° (A) and -20° (B) vertical angulations. Informed consent was obtained from patient willing to participate in the present study.

Fig. 2
A. Intraoral periapical radiography at 0°, -20° by vertical tube-shift method and their tracing showing the inferior alveolar nerve (IAN) canal moving upwards predicting the canal as buccal to the third molar root apex. B. Cone-beam computed tomography of the same patient as in Fig. 2A, showing the IAN canal buccal to the third molar root apex.
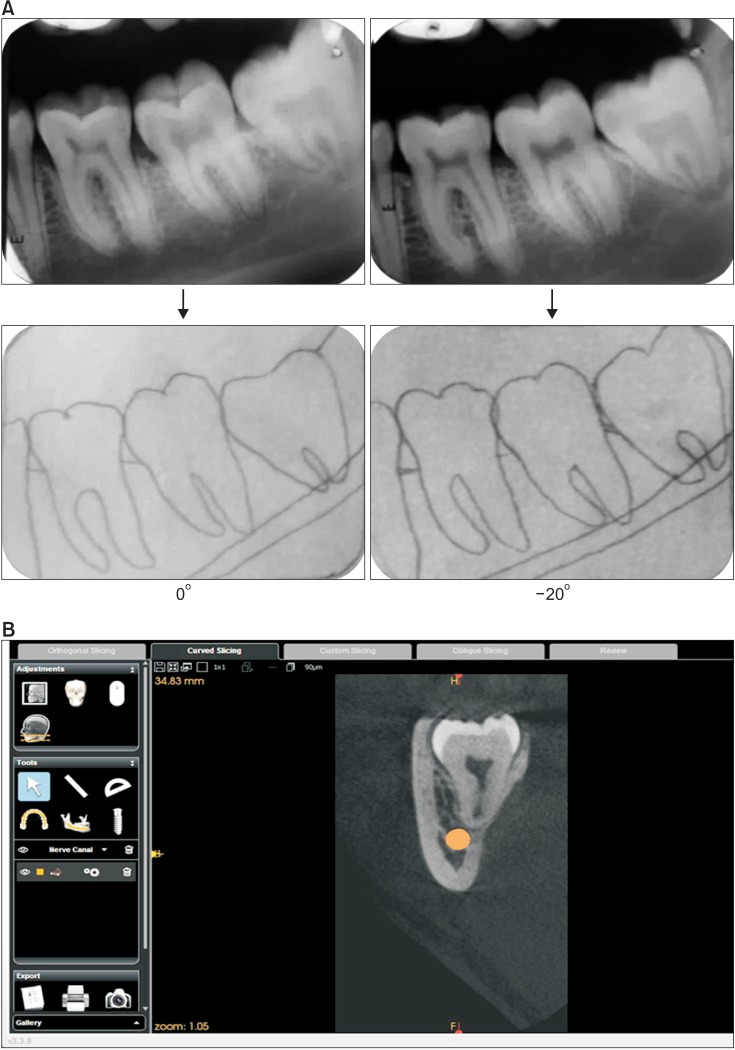
Fig. 3
A. Intraoral periapical radiography at 0°, -20° by vertical tube-shift method and their tracing showing inferior alveolar nerve (IAN) canal moving downwards predicting canal lingual to the third molar root apex. B. Cone-beam computed tomography of the same patient as in Fig. 3A, showing the IAN canal lingual to the third molar root apex.
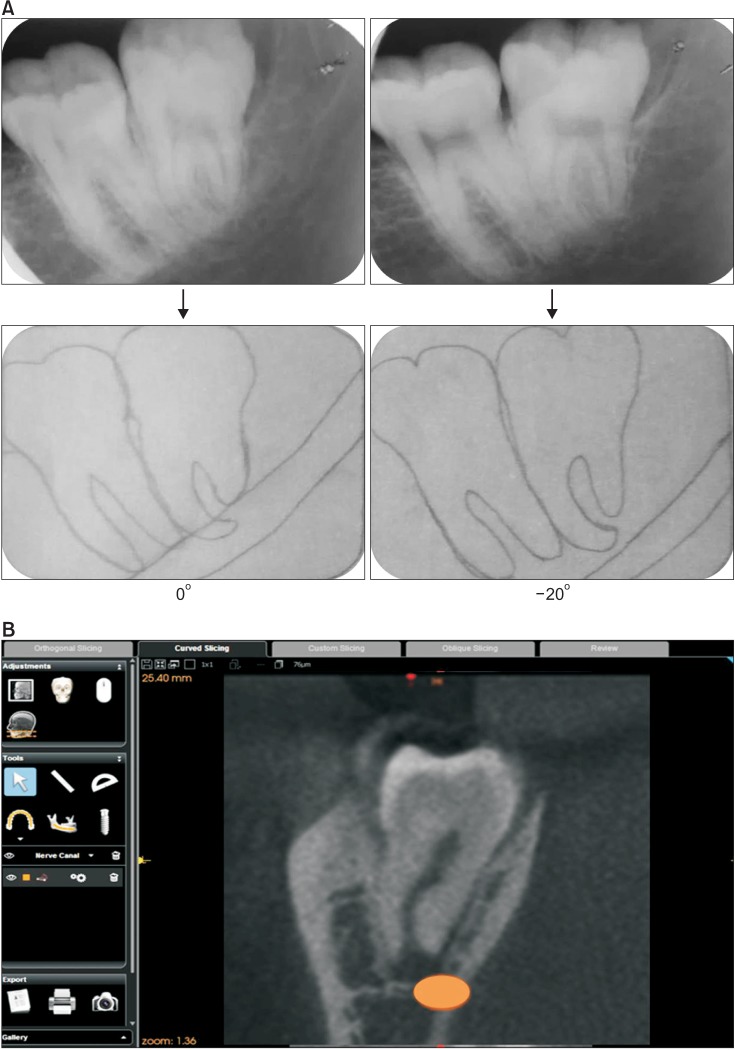
Fig. 4
A. Intraoral periapical radiography at 0°, -20° by vertical tube-shift method and their tracing showing no change in the inferior alveolar nerve (IAN) canal position relative to the third molar root apex. B. Cone-beam computed tomography of the same patient as in Fig. 4A showing no change in the IAN canal position relative to the third molar root apex.
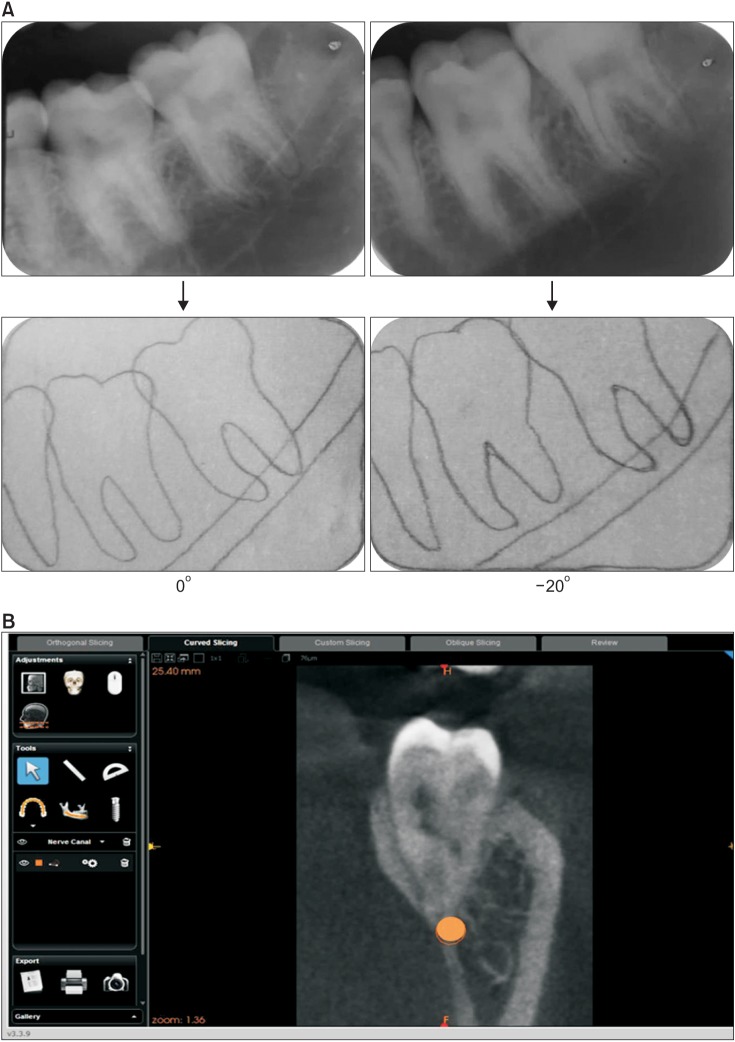
Table 2
Sensitivity, specificity, PPV, and NPV of the vertical localization technique for buccal placed IAN canal
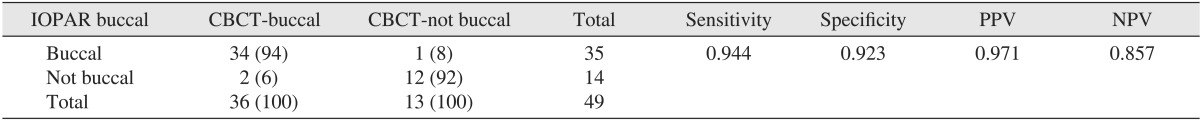
Table 3
Sensitivity, specificity, PPV, and NPV of the vertical localization technique for lingual placed IAN canal




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download