Abstract
Cemento-ossifying fibromas are benign tumors, and, although cases of an aggressive type have been reported, no cases of cemento-ossifying fibroma transforming into osteosarcoma have been documented previously. Low-grade osteosarcoma is a rare type of primary bone tumor, representing 1%-2% of all osteosarcomas. A 45-year-old female patient was diagnosed with cemento-ossifying fibroma, treated with mass excision several times over a period of two years and eight months, and followed up. After biopsy gathered because of signs of recurrence, she was diagnosed with low-grade osteosarcoma. The patient underwent wide excision, segmental mandibulectomy, and reconstruction with fibula free flap. The aim of this report is to raise awareness of the possibility that cemento-ossifying fibroma can transform into osteosarcoma and of the consequent necessity for careful diagnosis and treatment planning.
Cemento-ossifying fibromas are benign fibro-osseous tumors that are composed of fibrous tissue and a variable mixture of calcified materials. They are well-defined unilocular or multilocular lesions with slowly progressing enlargement of the affected bone. The most frequent site is the mandibular premolar and molar areas, and the tumor has a definite female predilection. Occasionally, it may grow to a massive size and cause serious cosmetic and functional problems, and there are rare reports of lesions behaving in an aggressive fashion1. Low-grade central osteosarcoma is a rare type of osteosarcoma. In general, osteosarcomas of the jaw are high-grade lesions. Low-grade lesions are rare and include well-differentiated intramedullary osteosarcomas and parosteal osteosarcomas2. These low-grade osteosarcomas may be mistaken for fibro-osseous neoplasms3.
We report a case of low-grade osteosarcoma in the mandible that was transformed from a recurrent cemento-ossifying fibroma. This is the first reported case of the transformation of cemento-ossifying fibroma into malignant low-grade central osteosarcoma.
A 45-year-old female patient was referred for a radiolucent lesion of the left posterior mandible, with complaints of a three-month history gingival swelling and tooth pain in the left mandibular second premolar. On intraoral examination, the overlying mucosa was intact with no paresthesia on the left lower lip. Bony swelling was suspected in the left posterior vestibule. The second premolar was the vital tooth. A panoramic radiograph showed external root resorption of the second molar and a relatively well-defined radiolucent lesion involving the posterior mandibular body and ramus.(Fig. 1) Computed tomography (CT) imaging showed buccolingual cortical expansion and a soft tissue mass.(Fig. 1) The surrounding soft tissue did not appear to be involved. Under local anesthesia, extraction of the second molar was performed, and a biopsy was taken below the extraction socket for histopathological examination. A histopathological diagnosis of cemento-ossifying fibroma was made. Histopathological examination showed dense fibroblastic proliferation, woven bone, and cementum-like material.(Fig. 2) Conservative mass excision under general anesthesia was performed. The surgical specimen was sent to a pathologist, and the pathologist recommended close follow-up because of the high cellularity of the specimen.
Five months after the first operation, the patient complained of tooth pain in the left mandibular second premolar and underwent root canal treatment. Periodic follow-up was performed, and there were no signs of recurrence on either clinical or radiographic examination for 16 months. After 16 months, however, follow-up panoramic radiograph and CT displayed signs of recurrence, including a mixed high-attenuation intrabony lesion and a partially multilocular lesion. Mass excision was performed under local anesthesia, the surgical specimen was submitted for histological examination; the pathological diagnosis was cemento-ossifying fibroma. One year after the second operation, the patient complained of discomfort in the left mandibular canine area, and CT revealed expansion of the lesion and signs of recurrence. Intentional root canal treatment of the left mandibular first premolar and mass excision were performed under general anesthesia.(Fig. 3) The pathological diagnosis was the same as previously, but the surgical specimen showed high cellularity and an infiltrative growth pattern into normal bone tissue without mitotic figures or cellular atypia.
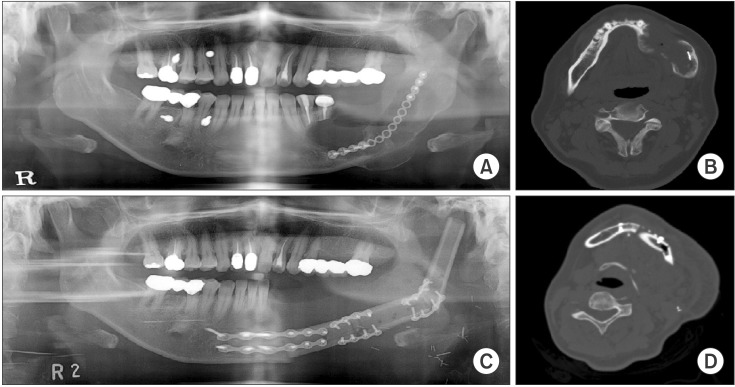
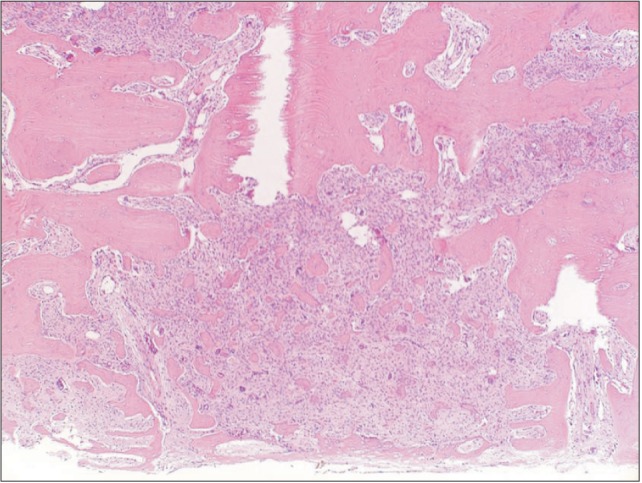
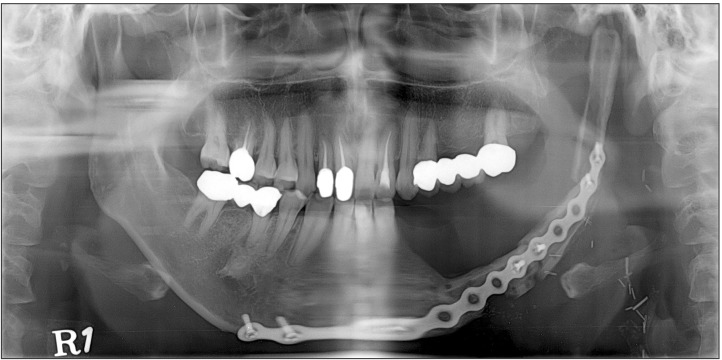
Three months after the third operation, tumor recurrence was suspected at the parasymphysis area on follow-up radiograph (Fig. 4), and a biopsy was taken from the buccal side of the lesion. The specimen showed minimal cellular atypia and irregular bony trabeculae with few mitotic figures (Fig. 5), so a diagnosis of low-grade osteosarcoma was made. No regional or distant metastasis was shown on magnetic resonance imaging or positron emission tomography-CT imaging. The patient underwent wide excision, segmental mandibulectomy, and reconstruction with fibula free flap.(Fig. 6)
Cemento-ossifying fibromas are benign fibro-osseous lesions of the jaw which have been described as demarcated or rarely encapsulated neoplasms consisting of fibrous tissue and various amounts of mineralized material such as bone and/or cementum4. The most frequent location is mandibular, involving the premolar and molar regions5. Radiologically, cemento-ossifying fibromas are initially characterized by well-differentiated osteolytic images5. As they evolve, the images show irregular opacities forming concentric bony trabeculae circumscribed by peripheral osteocondensation5. They are benign lesions, but sometimes may behave in an aggressive manner and cause extensive bone destruction6. In aggressive cases, en bloc resection or partial resection of the jaw is preferred to avoid or minimize the possibility of recurrence7. No cases of aggressive cemento-ossifying fibroma transforming into osteosarcoma have been previously documented.
Osteosarcomas of all sites account for 40%-60% of primary malignant bone tumors, and osteosarcomas of the mandible affect approximately 1 in 10 million persons per year, mostly young adults8. Low-grade osteosarcomas are very rare in the jaw. Only 14 cases have been reported in the literature2. The histopathology of low-grade central osteosarcoma usually shows bundles of spindle cells with minimal cytological atypia, rare mitotic figures, and a variable amount of osteoid formation9. Metastasis is less commonly seen than with conventional osteosarcoma9. Resection with wide surgical margins is the most important factor in determining prognosis and provides a 5-year survival rate of 80%. Adjuvant chemotherapy or radiotherapy seems to be inefficacious in cases of low-grade central osteosarcoma2.
In our case, the patient was treated with mass excision several times over a period of two years and eight months because of recurrent cemento-ossifying fibroma. Recurrence of these benign tumors following surgery is considered rare, although the reported recurrence rate varies between 0% and 30%4. This is the first reported case of low-grade osteosarcoma arising from cemento-ossifying fibroma, so there are insufficient data for evaluating this malignant transformation. However, oral and maxillofacial surgeons should be aware of the rare possibility that cemento-ossifying fibroma can transform into osteosarcoma and that careful diagnosis and regular follow-up are required in patients with cemento-ossifying fibromas.
References
1. Zupi A, Ruggiero AM, Insabato L, Senghore N, Califano L. Aggressive cemento-ossifying fibroma of the jaws. Oral Oncol. 2000; 36:129–133. PMID: 10889933.

2. Diniz AF, Filho JA, Alencar Rde C, Garcia RR, Silva MR, Ribeiro-Rotta RF, et al. Low-grade central osteosarcoma of the mandible: a case study report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:246–252. PMID: 17234543.

3. Demicco EG, Deshpande V, Nielsen GP, Kattapuram SV, Rosenberg AE. Well-differentiated osteosarcoma of the jaw bones: a clinicopathologic study of 15 cases. Am J Surg Pathol. 2010; 34:1647–1655. PMID: 20975343.
4. Peravali RK, Bhat HHK, Reddy S. Maxillo-mandibular cemento-ossifying fibroma: a rare case report. J Maxillofac Oral Surg. 2013; doi: 10.1007/s12663-013-0507-6.

5. Trijolet JP, Parmentier J, Sury F, Goga D, Mejean N, Laure B. Cemento-ossifying fibroma of the mandible. Eur Ann Otorhinolaryngol Head Neck Dis. 2011; 128:30–33. PMID: 20846921.

6. Hemavathy S, Roy S. Aggressive ossifying fibroma presenting as extensive mandibular swelling: a case report. Indian J Dent. 2011; 2:107–112.
7. Toro C, Millesi W, Zerman N, Robiony M, Politi M. A case of aggressive ossifying fibroma with massive involvement of the mandible: differential diagnosis and management options. Int J Pediatr Otorhinolaryngol Extra. 2006; 1:167–172.

8. Thariat J, Julieron M, Brouchet A, Italiano A, Schouman T, Marcy PY, et al. Osteosarcomas of the mandible: are they different from other tumor sites? Crit Rev Oncol Hematol. 2012; 82:280–295. PMID: 21868246.

9. Kumar A, Varshney MK, Khan SA, Rastogi S, Safaya R. Low grade central osteosarcoma--a diagnostic dilemma. Joint Bone Spine. 2008; 75:613–615. PMID: 18457982.
Fig. 2
Preoperative histological image shows woven bone and cementum-like material (H&E staining, ×40).
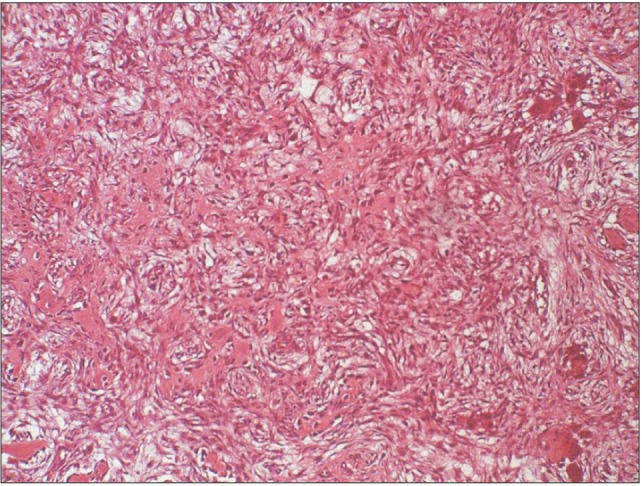
Fig. 3
Panoramic images after the first operation (A), before the second operation (B), after the second operation (C), and before the third operation (D).
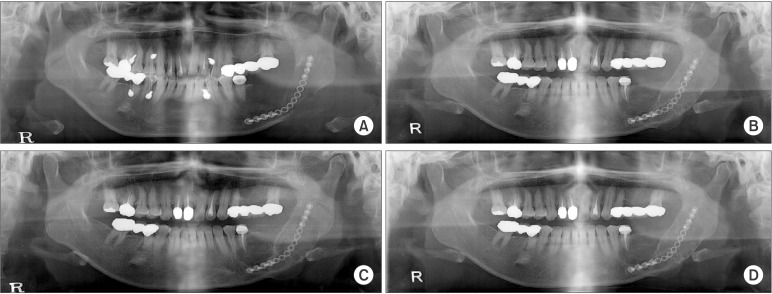
Fig. 4
A, B. Before operation, panorama and computed tomography (CT). C, D. After the final operation, panorama and CT.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download