Abstract
Aggressive benign odontogenic neoplasms have substantial potential to grow to an enormous size with resulting bone deformities, and they often invade adjacent tissues and spread beyond their normal clinical and radiographic margins; as such, they have a high rate of recurrence. Historically, management (conservative versus aggressive) on the basis of clinical, radiographic and/or histopathologic characteristics has been controversial. However, recent advances in the understanding of the biological features of these lesions may provide greater evidence of the benefits of conservative management. Three patients with different complaints and final histopathologic diagnoses were enrolled in the study. All three cases were treated by a single operator with similar conservative surgical procedures. During follow-up, the patients had uneventful secondary healing and bone regeneration, less packing time than previously reported, no clinical or radiographic evidence of recurrence and no apparent deformity. The aggressive behavior of these lesions requires long clinical and radiographic follow-up. Conservative surgical management may be an option to reduce recurrence and morbidity and increase the probability of uneventful secondary healing and bone regeneration.
Ameloblastoma and odontogenic keratocyst (OKC) are known as aggressive benign odontogenic neoplasms (ABONs) due to their aggressive behavior. They have substantial potential to grow to enormous size with resulting bone deformities, invade the adjacent tissues and spread beyond their normal clinical and radiographic margins. Because of the aforementioned features, they may have a high rate of recurrence1,2,3. In the current academic literature, there is considerable controversy about treatment based on the clinical, radiographic and/or histopathologic characteristics of ABON. Previously, there has been general consensus advising the complete eradication of these lesions using an aggressive surgical approach, such as marginal or segmental resection with or without reconstruction2,4,5,6. However, resection without reconstruction may create severe postoperative deformities that have adverse psychosocial consequences, particularly in young patients; while resection with reconstruction may prevent such adverse psychosocial consequences, it entails additional surgery and is prohibitively expensive4,6. On the other hand, recent advances in the understanding of the biological features of these lesions may provide evidence of the benefits of conservative surgical treatment that is not only affordable, but also preserves both structural and functional integrity3,4,5,7.
Prior reported conservative treatment options for ABON include marsupialization, decompression, enucleation, curettage, and a combination of these techniques2,4. Of the aforementioned conservative surgical procedures, enucleation by itself has a high tumor recurrence rate; in order to reduce this risk, adjunctive procedures, such as peripheral ostectomy, Carnoy's solution and cryotherapy, have been reported, but each have their respective benefits and risks2,7. Carnoy's solution can penetrate and fix tissue to the depth of 1.54 mm into bone after 5 minutes of exposure8. Due to this property, it reduces rate of recurrence in ABON. On the other hand, the surgical space created by the removal of these lesions requires packing with aseptic dressing material to achieve uneventful wound healing because primary closure may lead to infection given the large amount of dead space3,7,9. Ideal dressing materials used in the mouth should be able to reduce postoperative pain, promote healing and prevent infection. Iodoform is one such dressing material as it is shown to reduce wound fluids through fibrinolytic activity, exhibit antimicrobial activity after topical application to wounds, and reduce pain by covering denuded bone surface10,11.
This case series was performed by a single operator to evaluate the success of treating ABON using a conservative surgical procedure, specifically enucleation with or without Carnoy's application followed by iodoform gauze dressing.
A 21-year-old male patient presented to our hospital with a 5-month history of swelling and occasional pain in the lower left posterior teeth region that had gradually worsened. He did not have a history of dental infection or trauma. His medical history was unremarkable. On extraoral examination, facial asymmetry was apparent with diffuse swelling involving the left side of mandible, measuring 4.5×4.0 cm. The swelling was soft and tender on palpation. Intraoral examination revealed multiple retained and missing teeth as well as cortical expansion of teeth #75, #36, and #37 with vestibular obliteration.
A panoramic view radiograph showed a unilocular welldefined radiolucent lesion extending from the distal surface of the left mandibular first premolar to the apices of the second molar and <1 cm of residual bone remaining in the lower border and alveolar process of the second molar with inferior alveolar nerve (IAN) involvement.(Fig. 1. C) Axial computed tomography (CT) revealed a fairly large (3.5×3.2×3.0 cm) well-defined rounded cystic destructive lesion involving the left mandibular body with a large exophytic component (Fig. 1. A), while three-dimensional CT of the mandible revealed a complete loss of the osseous component in the same region. (Fig. 1. B) Fine needle aspiration yielded 10 mL of blood-mixed fluid submitted along with tissues obtained from the lesion for histopathologic examination, which revealed findings suggestive of luminal unicystic ameloblastoma.
A healthy 6-year-old male patient was referred to our hospital for painful swelling of the area surrounding the lower left posterior teeth which began 6 weeks prior and gradually progressed with worsening pain. His medical and family history was unremarkable with no history of trauma. On extraoral examination, facial asymmetry was apparent with diffuse swelling involving the left side of the mandible, measuring 3.5×3.0 cm. The swelling was hard and tender on palpation. Intraoral examination revealed caries on two of the lower left teeth, #74 and #75, and buccal cortical plate expansion along with vestibular obliteration in the same region.
An orthopantomogram revealed an ill-defined unilocular radiolucent lesion that was situated at the apices of the primary molars, and this made it difficult to discern between the #35 tooth bud and the cystic lining.(Fig. 2. A) Chest X-ray revealed a bifid 10th rib on the left side.(Fig. 2. B)
The patient underwent fine needle aspiration cytology (FNAC), and histopathologic examination revealed the presence of inflammatory infiltrates with necrotic material, few epithelial cells and the absence of malignant cells, findings that are suggestive of a benign cystic lesion of the mandible. Taken together, the clinical, radiologic, and cytological findings were suggestive of OKC.
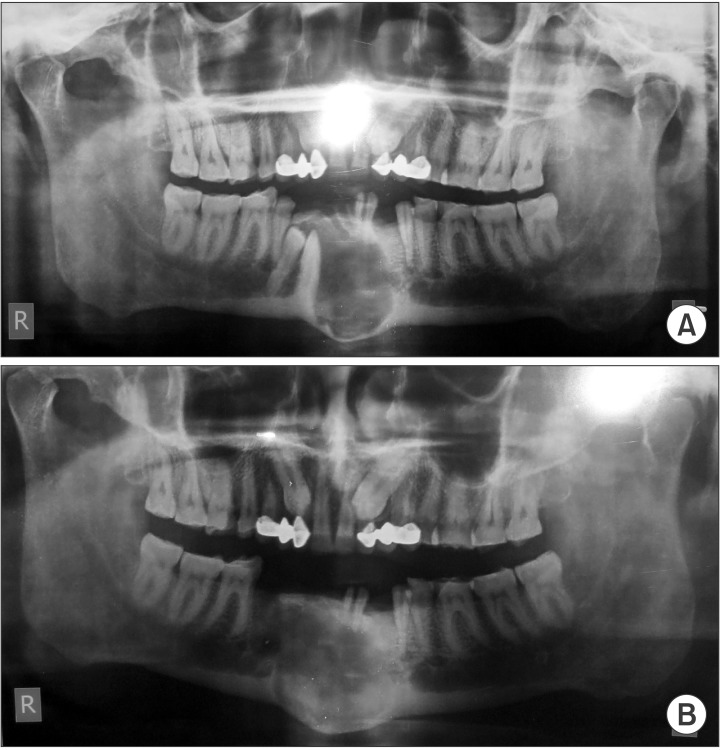
A 58-year-old male presented to our hospital for the evaluation of swelling and thick discharge from the anterior region of the mandible for the previous 15 days. Relevant medical history included hepatitis B infection. On clinical examination, there was mild facial asymmetry. Intraoral examination revealed mild swelling, mucosal breach and buccal expansion in anteroposterior direction on the anterior mandibular region. There was no lymphadenopathy. The patient was evaluated with panoramic radiography, which revealed a unilocular lucency that extended from the mesial surface of #33 to the mesial surface of #45, impacted #43 and #44 and maxillary bilateral canine impaction.(Fig. 3. A)
Fine needle aspiration yielded thick yellowish material that was submitted along with tissue obtained from the lesion for histopathologic examination, which revealed findings suggestive of OKC.
Surgery was performed by a single operator using a set of standard techniques with all standard precautions for blood-borne pathogens. Of these three cases, the first two surgeries were performed under general anesthesia and the last case under local anesthesia. In all cases, the surgical site was exposed using a lower vestibular incision and the perioperative findings were recorded. Of note, the lesions appeared encapsulated and brownish-blue. In case 1, there was a complete anteroposterior loss of the osseous component with <1 cm of residual bone in the alveolus and lower border. In case 2, the #35 tooth bud was associated with the cystic lining.
After surgical exposure, all lesions were enucleated carefully and sharp edges were smoothed with a rotary instrument. Carnoy's solution was applied for 5 minutes after enucleation only in case 3. In case 1, preventive measures were taken to preserve as much of the periosteum and residual bone as possible to achieve uneventful healing. Finally, the resulting cavity was irrigated and packed with iodoform gauze. During follow-up, the wound was evaluated and the packing was changed every 7 days until complete soft tissue healing was achieved6,12. All enucleated tissues were sent for histopathologic examination. Microscopic examination of cases 1 and 3 was similar to the respective initial diagnoses while case 2 revealed a radicular cyst, which was different from the initial provisional diagnosis of OKC.
During the first four follow-up wound evaluations, slight bleeding was noted, but resolved after repeated wound packing with iodoform gauze. Complete soft and hard tissue healing were achieved at about 4 months and 1 year in case 1 (Fig. 1. D), 6 weeks and 5 months in case 2 (Fig. 2. C), and 5 months and 1 year in case 3 (Fig. 3. B), respectively. In addition, there was no evidence of recurrence and secondary healing and bone regeneration were uneventful. The aggressive nature of ABON required long clinical and radiographic follow-up.
Ameloblastoma and OKC are two of the most aggressive ABONs, which is demonstrated by their relatively high recurrence rate, rapid growth and tendency to invade adjacent tissues3,4,6,7,9,13,14,15. Treatment of ameloblastoma and OKC remains a controversial subject. The treatment approach should be based on the size and site of the lesion, recurrence status and radiographic evidence of cortical perforation. There has been a general consensus in the literature, guided by the aforementioned characteristics, for complete lesion eradication with aggressive surgical approaches, such as resection with or without reconstruction. These aggressive approaches may lead to deformities, which can have adverse psychosocial consequences, particularly for young patients. Therefore, the primary aim should be the preservation of structural and functional integrity whenever possible3,6,7,14,15,16.
Previous studies reported high recurrence rates with enucleation alone, but recurrence rates can be reduced when performed with adjunctive procedures6,9,17,18. However, adjunctive procedures, including peripheral ostectomy, Carnoy' s solution, and cryotherapy, come with additional risks7. For example, Carnoy's solution and other chemical cauterization could potentially damage nearby vital structures such as the IAN and/or permanent tooth buds in mixed dentition. When operating near such vital structures, the appropriate choice would instead be marsupialization or decompression7,9. However, if lesions are not near the aforementioned vital structures, then the application of Carnoy's solution is commonly accepted given its ability to penetrate and fix tissues up to a depth of 1.54 mm into the bone after 5 minutes of exposure6,7, 8,17,18. Cryotherapy is another adjunctive procedure with similar results, but its application can be complicated and wound dehiscence is observed in all cases7,19. Peripheral ostectomy is impractical in large lesions due to the presence of very thin bony walls, and should be avoided in cases with ameloblastoma because it may implant ameloblastoma foci more deeply in the bone7,14. On other hand, a large surgical cavity created by enucleation should undergo secondary wound healing rather than primary wound closure to reduce the risk of postoperative infection secondary to dead space3,7,9. Dressing material used for secondary wound healing in the mouth should have the following properties: reduction of postoperative pain, promotion of healing and prevention of infection. Iodoform is one such dressing material because it reduces wound fluids by fibrinolytic activity, exhibits antimicrobial activity after topical application and covers denuded bone surfaces to reduce pain10,11. Recent studies reported that decompression and marsupialization alter the epithelial lining of keratocystic odontogenic tumor into a less aggressive form, and some tumors have completely resolved clinically and radiographically with treatment3,7. Based on the above findings, the author recommends performing enucleation with or without Carnoy's solution application followed by iodoform gauze dressing for all cases.
Recent studies suggest that management of Ackermann histological subtype-1 ameloblastoma by enucleation is associated with good prognosis. However, in cases with cortical perforation, the tumor behaves like a solid ameloblastoma and should therefore be managed accordingly. On other hand, if there is IAN involvement, then the application of Carnoy's solution should be avoided to limit postoperative paresthesia 1,7,13. Typically, the management of case 1 would involve radical surgery with or without reconstruction1, but given the young age of the patient, the author opted for a conservative approach of enucleation followed by iodoform gauze packing. The application of Carnoy's solution was contraindicated because the involvement of IAN and exposed periosteum increased the risk of paresthesia had it been applied. Case 2 followed a similar approach because developing tooth buds were a contraindication for Carnoy's solution application. However, case 3 did not have any such contraindications, so it was managed by enucleation with Carnoy's solution application followed by iodoform gauze dressing. There was no evidence of recurrence during the follow-up period for any of the cases.
Zhou et al.7 reported requiring local anesthesia for the first two dressing changes, observing minor bleeding during each dressing change for the first two months that ultimately resolved after repacking, and noting that the average duration of required packing was 10.2 months (range, 7-15 months) and packing was performed by clinical assistants. In the current case series being reported, no local anesthesia was required in any dressing changes, slight bleeding was observed in the first 4 dressing changes (1 month) that resolved by repacking, and the average duration of required packing was 3.67 months (range, 2-5 months); packing was performed by a doctor. These differences could be due to differences in postoperative care by a doctor as compared with clinical assistants. Other possible reasons could be the difference in the age of the patients and size of the lesions.
Yildirim et al.3 and Hadziabdic et al.20 reported that radiographically complete bone healing was achieved in about 12 and 16 months in their respective studies. Similar results were achieved in cases 1 and 3, but a considerably shorter duration of complete bone healing was achieved in case 2 (about 5 months). This shorter duration of healing might be due to the age of the patient and size of the lesion.
Management of ABON remains controversial, but in light of prior clinical trials, there is a general consensus recommending complete lesion eradication with radical surgical procedures, which may cause deformity. These deformities can have adverse psychosocial consequences, particularly for young patients. Therefore, the primary aim should be to preserve structural and functional integrity for a better postoperative quality of life for patients. Enucleation with or without Carnoy's solution application followed by iodoform gauze dressing can be recommended as a good conservative treatment option that has a low recurrence rate with uneventful secondary healing for ABON. The author also recommends a long clinical and radiographic follow-up due to the aggressive nature of ABON.
References
1. Gupta N, Saxena S, Rathod VC, Aggarwal P. Unicystic ameloblastoma of the mandible. J Oral Maxillofac Pathol. 2011; 15:228–231. PMID: 22529587.

2. Abdullah WA. Surgical treatment of keratocystic odontogenic tumour: a review article. Saudi Dent J. 2011; 23:61–65. PMID: 24151416.

3. Yildirim G, Ataoglu H, Kalayci A, Ozkan BT, Kucuk K, Esen A. Conservative treatment protocol for keratocystic odontogenic tumour: a follow-up study of 3 cases. J Oral Maxillofac Res. 2010; 1:e7. PMID: 24421977.

4. Hasegawa T, Imai Y, Takeda D, Yasuoka D, Ri S, Shigeta T, et al. Retrospective study of ameloblastoma: the possibility of conservative treatment. Kobe J Med Sci. 2013; 59:E112–E121. PMID: 24598272.
5. Kahairi A, Ahmad RL, Islah LW, Norra H. Management of large mandibular ameloblastomas: a case report and literature reviews. Arch Orofac Sci. 2008; 3:52–55.
6. Giuliani M, Grossi GB, Lajolo C, Bisceglia M, Herb KE. Conservative management of a large odontogenic keratocyst: report of a case and review of the literature. J Oral Maxillofac Surg. 2006; 64:308–316. PMID: 16413905.

7. Zhou H, Hou R, Ma Q, Wu K, Ding Y, Qin R, et al. Secondary healing after removal of large keratocystic odontogenic tumor in the mandible: enucleation followed by open packing of iodoform gauze. J Oral Maxillofac Surg. 2012; 70:1523–1530. PMID: 22330329.

8. Hellstein J, Hopkins T, Morgan T. The history and mystery of Carnoy's solution: an assessment of the need for chloroform. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:e24.
9. Kalaskar R, Unawane AS, Kalaskar AR, Pandilwar P. Conservative management of unicystic ameloblastoma in a young child: report of two cases. Contemp Clin Dent. 2011; 2:359–363. PMID: 22346168.

10. Mizokami F, Murasawa Y, Furuta K, Isogai Z. Iodoform gauze removes necrotic tissue from pressure ulcer wounds by fibrinolytic activity. Biol Pharm Bull. 2012; 35:1048–1053. PMID: 22791151.

11. Freedman M, Stassen LF. Commonly used topical oral wound dressing materials in dental and surgical practice--a literature review. J Ir Dent Assoc. 2013; 59:190–195. PMID: 24156211.
12. Maria A, Sharma Y, Chabbria A. Marsupialization as a treatment option of a large odontogenic keratocyst: a case report with the review of literature. Peoples J Sci Res. 2012; 5:46–51.
13. Dolanmaz D, Etoz OA, Pampu A, Kalayci A, Gunhan O. Marsupialization of unicystic ameloblastoma: a conservative approach for aggressive odontogenic tumors. Indian J Dent Res. 2011; 22:709–712. PMID: 22406718.

14. Ramesh RS, Manjunath S, Ustad TH, Pais S, Shivakumar K. Unicystic ameloblastoma of the mandible--an unusual case report and review of literature. Head Neck Oncol. 2010; 2:1. PMID: 20157425.

15. Park SH, Kim NK, Kim KH, Kang SH, Park HS, Kim HJ, et al. Postoperative recurrences of odontogenic keratocyst: the behavior and proposal of critical follow-up period. J Korean Assoc Oral Maxillofac Surg. 2008; 34:456–459.
16. Shin MY, Lee HK, Choi JW, Shin SS, Park YH, Park JW. Literature review and case report: the conservative treatment of unicystic ameloblastoma. J Korean Assoc Oral Maxillofac Surg. 2005; 31:70–73.
17. Güler N, Sençift K, Demirkol O. Conservative management of keratocystic odontogenic tumors of jaws. ScientificWorldJournal. 2012; 2012:680397. PMID: 22454609.

18. Lee PK, Samman N, Ng IO. Unicystic ameloblastoma--use of Carnoy's solution after enucleation. Int J Oral Maxillofac Surg. 2004; 33:263–267. PMID: 15290793.

19. Carneiro JT, Guerreiro Rodrigues, Dias Carreira AS. Use of gas combination cryosurgery for treating ameloblastomas of the jaw. J Craniomaxillofac Surg. 2012; 40:e342–e345. PMID: 22421467.

20. Hadziabdic N, Sulejmanagic H, Selimovic E, Sulejmanagic N. Therapeutic approach to large jaw cysts. HealthMed. 2011; 5:1793–1799.
Fig. 1
A. Preoperative axial computed tomography (CT) shows unilocular lucency involving the left mandibular body with a large exophytic component. B. Preoperative three-dimensional CT shows a complete loss of cortical and cancellous bone in the left mandibular body region and <1 cm residual bone remaining in the alveolus and lower border. C. Preoperative panoramic radiograph shows unilocular lucency extending from the angle of the mandible to the left first premolar tooth along with <1 cm residual bone remaining in the alveolus and lower border. D. One-year postoperative panoramic radiograph shows good bone regeneration and no sign of recurrence.
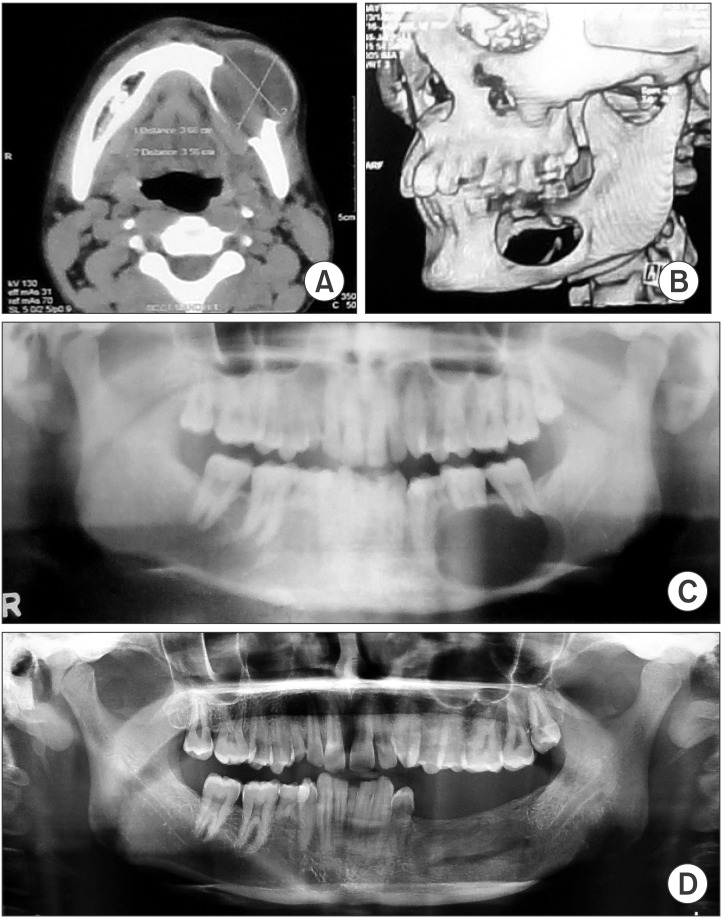
Fig. 2
A. Preoperative panoramic radiograph shows unilocular lucency extending from the mesial root of the left mandibular first molar to the left deciduous canine. B. Chest X-ray reveals a bifid 10th rib on the left side (arrow). C. Five-month postoperative panoramic radiograph shows good bone regeneration and no sign of recurrence.
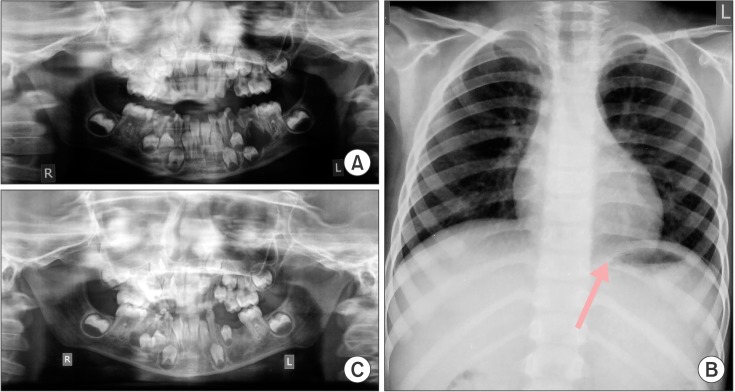
Fig. 3
A. Preoperative panoramic radiograph shows unilocular lucency extending from the mesial surface of the left mandibular canine to the mesial surface of the right 2nd premolar along with impacted #43 and #44. B. Five-month postoperative panoramic radiograph shows good bone regeneration and no sign of recurrence.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download