Abstract
Herpes zoster virus (HZV) infections are caused by reactivation of the varicella zoster virus. Reactivation symptoms commonly affect the thoracolumbar trunk, and rarely affect the mandibular branches of the trigeminal nerve. When the mandibular branches are involved, lesions appear proximal to the innervation area. This condition may be associated with exfoliation of the teeth and osteonecrosis of the jawbone. We report a case of mandibular osteomyelitis after herpes zoster infection and we present a review of the literature on mandibular-branch involvement of HZV-related osteonecrosis.
Varicella zoster virus (VZV) causes chickenpox and herpes zoster (HZ). Though chickenpox usually only results in benign childhood illness, the virus remains in the sensory ganglia in a latent state. Reactivation of the latent virus causes HZ, which presents as a cutaneous vesicular eruption in the area innervated by the affected sensory nerve1. HZ usually occurs in middle-aged and elderly people, at an average rate of approximately 2-3 per 1,000 people per year. The incidence increases with age: the rate is 5 per 1,000 people per year among patients >50 years old, 7-8 per 1,000 people per year among patients >60 years old, and 10 per 1,000 people per year among patients >80 years old2. Predisposing factors include having human immunodeficiency virus (HIV)/AIDS, leukemia, lymphoma, or diabetes mellitus, or undergoing systemic steroid treatment, chemotherapy, or radiotherapy. Stress or trauma can also induce HZ34. The most commonly affected sites are the thoracic dermatomes (T3-L3, 56%) and the trigeminal ganglia (~20%). Of the three branches of the trigeminal nerve, the one that leads to the ophthalmic nerve is affected most frequently. Oral manifestations accompany other more common symptoms when the maxillary or mandibular branches are involved56. When there is maxillary or mandibular involvement, complications, such as alveolar bone necrosis or tooth exfoliation, are reported to occur34. Herein, we report a case of osteonecrosis in the mandible after a HZ infection that involved the mandibular branch of the trigeminal nerve and we present a literature review of similar cases.
A 64-year-old male patient visited at Department of Oral and Maxillofacial Surgery of Pusan National University Hospital (Busan, Korea) on December 16, 2013 and his chief complaint was alveolar bone exposure of the left mandible. Five weeks before he presented to the hospital, a skin lesion appeared along the left mandibular area and he was given an antiviral agent by a dermatologist.(Fig. 1. A) He no other relevant medical history. Intraoral examination showed alveolar bone exposure in the #34, #35 area and third degree tooth mobility in #31-#35.(Fig. 1. B) Radiographic examination showed a diffuse and irregular radiolucent bone lesion on the left mandible in panoramic view, and low-density soft tissue swelling was seen on computed tomography.(Fig. 2) We conducted incisional biopsy and found acute and chronic inflammation. The patient had no history of receiving a prescription for any medication that affects bone metabolism and had never received radiotherapy. We determined that the inflammation originated from the patients' teeth; thus, we diagnosed his condition as left mandibular osteonecrosis by trigeminal HZ. We treated him with sequestrectomy and we removed teeth #31-#35.(Fig. 3) According to histopathology, eosinophilic intranuclear inclusion bodies and multinuclear giant cells were observed in the epithelium, and immunohistochemical staining showed the cells were CD68+. In the necrotic bone, neutrophils, lymphocytes and plasma cells were identified in the acute and chronic inflammation areas.(Fig. 4) No additional tooth loss, bone exposure, or osteonecrosis occurred during the follow-up period. Also, no other complications, such as postherpetic neuralgia, occurred.
This study was approved by Institutional Review Board of Pusan National University Hospital (PNUH E-2014158).
Herpes zoster virus (HZV) most often affects the thoracic dermatomes and the incidence of activation in the trigeminal nerve is 13%. In these cases, the ophthalmic nerve is affected most often, followed by the maxillary nerve and then the mandibular nerve7. Vesicular lesions can appear on the face, in the oral cavity, the eyes and the tongue. Additionally, acute pulpitis, toothache, root resorption and periapical lesions are often observed when the maxillary and mandibular nerves are involved. Rarer still, some cases involve osteonecrosis and tooth exfoliation489. Jain et al.4 reported osteonecrosis and tooth exfoliation in HZV cases, with an average age of 57.6 years old and no difference by gender410.
The pathologic mechanisms behind HZ-involving osteonecrosis are controversial, and several hypotheses are under debate. One hypothesis states that it is due to local vasculitis caused by direct extension of a neural inflammatory response to adjacent blood vessels11, which may cause infarction of the trigeminal vessels and lead to jawbone necrosis by triggering ischemia8912. The second hypothesis argues that generalized infection in the trigeminal nerves is the cause of vasculitis of the periosteum and periodontium, which induces osteonecrosis and tooth exofoliation13. The third hypothesis argues that osteonecrosis is caused by denervation of the bone, but that it does not induce serious osteonecrosis during a short time period14. The fourth hypothesis states that systemic viral infection leads to damage to the odontoblasts, which induces pulp necrosis. The fifth hypothesis argues that pre-existing pulpitis, periodontitis, or prior surgical procedures can induce osteonecrosis10.
The treatment goal for HZV infection is to reduce acute viral infection, acute pain, and postherpetic neuralgia. Immediate administration of an anti-viral agent and active use of painkillers for postherpetic neuralgia are required6. Acyclovir, valacyclovir, and famciclovir reduce infection symptoms. Acyclovir at 800-mg doses, five times a day for a week, or valacyclovir at 1,000-mg doses, three times a day for a week, reduce HZ-related pain and incidence of postherpetic neuralgia as well as duration of atypical sensation15. Once postherpetic neuralgia occurs, there are no effective treatments. Tricyclic antidepressants, anticonvulsant agents, gabapentin and opioids are sometimes used to reduce pain, but administration of these drugs is limited because of systemic side effects16. The most effective modality is prophylactic vaccination with a zoster virus vaccine17.
Generally, HZV-related osteomyelitis or osteonecrosis appears 2 to 6 weeks (average, 21.2 days) after HZ reactivation10. When HZV-related osteonecrosis of the jaw occurs, it can be managed by proper antibiotic administration, curettage or debridement of necrotic tissue and periodic follow-up3414. In our case, we successfully managed the lesions with sequestrectomy and we performed a peripheral ostectomy until unaffected bone was exposed.
There are many predisposing factors for osteonecrosis of the jawbone. Although HZV infection involving the trigeminal nerve can cause osteonecrosis and tooth exfoliation, this condition can be managed by immediate administration of an antiviral agent, safe pain control and surgical removal of the necrotic tissue.
References
1. Volvoikar P, Patil S, Dinkar A. Tooth exfoliation, osteonecrosis and neuralgia following herpes zoster of trigeminal nerve. Indian J Dent Res. 2002; 13:11–14. PMID: 12420562.
2. Gross G, Schöfer H, Wassilew S, Friese K, Timm A, Guthoff R, et al. Herpes zoster guideline of the German Dermatology Society (DDG). J Clin Virol. 2003; 26:277–289. PMID: 12637076.
3. Mendieta C, Miranda J, Brunet LI, Gargallo J, Berini L. Alveolar bone necrosis and tooth exfoliation following herpes zoster infection: a review of the literature and case report. J Periodontol. 2005; 76:148–153. PMID: 15830651.

4. Jain MK, Manjunath KS, Jagadish SN. Unusual oral complications of herpes zoster infection: report of a case and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 110:e37–e41. PMID: 20692192.

5. Carbone V, Leonardi A, Pavese M, Raviola E, Giordano M. Herpes zoster of the trigeminal nerve: a case report and review of the literature. Minerva Stomatol. 2004; 53:49–59. PMID: 15041920.
6. Gershon AA, Gershon MD, Breuer J, Levin MJ, Oaklander AL, Griffiths PD. Advances in the understanding of the pathogenesis and epidemiology of herpes zoster. J Clin Virol. 2010; 48(Suppl 1):S2–S7. PMID: 20510263.

7. Tidwell E, Hutson B, Burkhart N, Gutmann JL, Ellis CD. Herpes zoster of the trigeminal nerve third branch: a case report and review of the literature. Int Endod J. 1999; 32:61–66. PMID: 10356471.

8. Muto T, Tsuchiya H, Sato K, Kanazawa M. Tooth exfoliation and necrosis of the mandible--a rare complication following trigeminal herpes zoster: report of a case. J Oral Maxillofac Surg. 1990; 48:1000–1003. PMID: 2395037.

9. Garty BZ, Dinari G, Sarnat H, Cohen S, Nitzan M. Tooth exfoliation and osteonecrosis of the maxilla after trigeminal herpes zoster. J Pediatr. 1985; 106:71–73. PMID: 3965684.

10. Mintz SM, Anavi Y. Maxillary osteomyelitis and spontaneous tooth exfoliation after herpes zoster. Oral Surg Oral Med Oral Pathol. 1992; 73:664–666. PMID: 1437032.

11. Wright WE, Davis ML, Geffen DB, Martin SE, Nelson MJ, Straus SE. Alveolar bone necrosis and tooth loss. a rare complication associated with herpes zoster infection of the fifth cranial nerve. Oral Surg Oral Med Oral Pathol. 1983; 56:39–46. PMID: 6576309.

12. Hall HD, Jacobs JS, O'Malley JP. Necrosis of maxilla in patient with herpes zoster: report of a case. Oral Surg Oral Med Oral Pathol. 1974; 37:657–662. PMID: 4524373.
13. Gilden D, Cohrs RJ, Mahalingam R, Nagel MA. Varicella zoster virus vasculopathies: diverse clinical manifestations, laboratory features, pathogenesis, and treatment. Lancet Neurol. 2009; 8:731–740. PMID: 19608099.

14. Shevick IM. Mandibular herpes zoster; with report on the use of cortisone in a case with geniculate ganglion symptoms. Calif Med. 1953; 79:444–448. PMID: 13106732.
15. Mustafa MB, Arduino PG, Porter SR. Varicella zoster virus: review of its management. J Oral Pathol Med. 2009; 38:673–688. PMID: 19691461.

16. Nalamachu S, Morley-Forster P. Diagnosing and managing postherpetic neuralgia. Drugs Aging. 2012; 29:863–869. PMID: 23038608.

17. Gan EY, Tian EA, Tey HL. Management of herpes zoster and postherpetic neuralgia. Am J Clin Dermatol. 2013; 14:77–85. PMID: 23456596.

Fig. 2
Preoperative radiographs. A. Preoperative panoramic view. B. Preoperative computed tomography view.
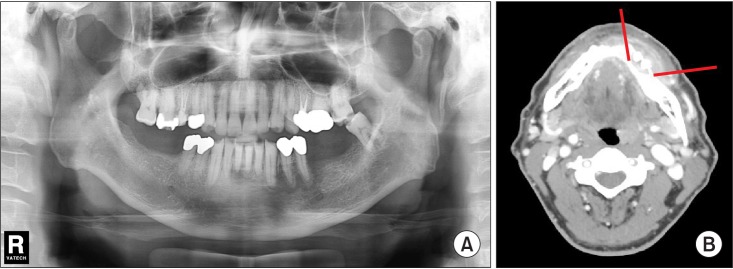
Fig. 3
Sequestrectomy and teeth removal were conducted. A sound bone bed was exposed and primarily closed.
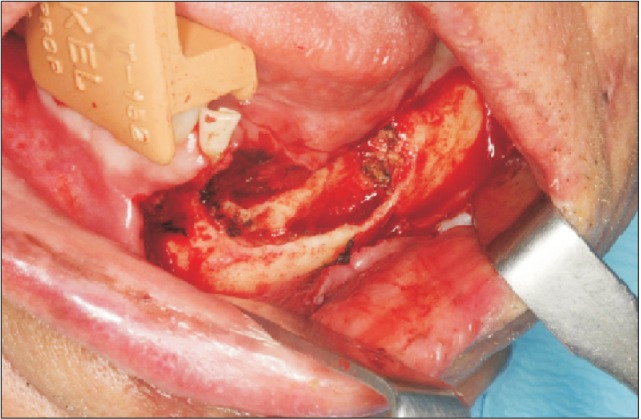
Fig. 4
Histologic findings. A. Eosinophilic intranuclear inclusion bodies and multinucleated giant cells are observed (H&E staining, ×400). B. Stained cells were CD68+ (IHC staining, ×200). C. Scattered neutrophils, lymphocytes, and plasma cells, which indicated acute and chronic inflammation, were observed (H&E staining, ×400).





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download