Abstract
Bisphosphonate-related osteonecrosis of the jaw (BRONJ) occurs mainly in female patients. In males the occurrence rate is low, which seems to be related to the low incidence of osteoporosis in men. Unfortunately, BRONJ tends to be ignored in general dental clinics in male patients with a history of osteoporosis treatment. BRONJ occurred in a male patient due to the clinician's lack of interest in the patient's history. In this case, the male patient was on bisphosphonate therapy because of a orchiectomy, and a dental treatment was performed without consideration of his medical history, resulting in BRONJ. We performed careful examinations and treatment with antibiotics and surgical operations. The postoperative healing was successful. In light of this particular case, we concluded that careful listening to the patient's history is very important.
In Korea, the number of cases of bisphosphonate-related osteonecrosis of the jaw (BRONJ) occurring in female patients as a result of dental treatment following medication for postmenopausal osteoporosis has been recently increasing1. The American Association of Oral and Maxillofacial Surgeons (AAOMS) define BRONJ as medication-related osteonecrosis of the jaw in cases where antiresorptive or antiangiogenic agents have been administered, continuous bone exposure in the maxillofacial area for a period of more than eight weeks has been confirmed, and radiation therapy of the maxillofacial area has not been performed2. The AAOMS also describe treatment methods according to the classifications determined by the patient's symptoms2. Although BRONJ occurs more frequently in females, there are cases of BRONJ occurring in males as well. These are mainly related to a history of malignancy, multiple myeloma, and osteoporosis which occurs as a result of aging3.
A male patient in his late eighties visited our department from a local clinic for treatment of osteonecrotic lesions of the right posterior maxillary region. He had undergone a tooth extraction (the first right upper molar) at a local clinic three years ago. The sequestrum was exposed through the unhealed extraction wound with purulent discharge. The surrounding soft tissue showed erythematous and edematous gingiva.(Fig. 1)
The patient's medical history revealed that he had a orchiectomy to remove diffuse large B cell lymphoma from his testicles followed by chemotherapy and radiation therapy to his para-aortic lymph nodes and pelvic region six years prior. Two years after the cancer treatments, he was diagnosed with osteoporosis and took alendronate (Fosamax Tab. 70 mg; MSD Korea, Seoul, Korea) once a week until visiting our department. At the time of osteoporosis diagnosis, his bone mineral density T-score was -2.7.
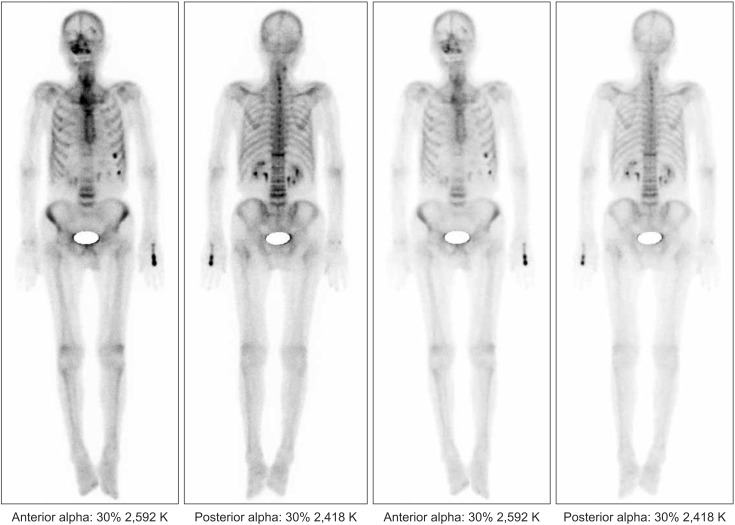
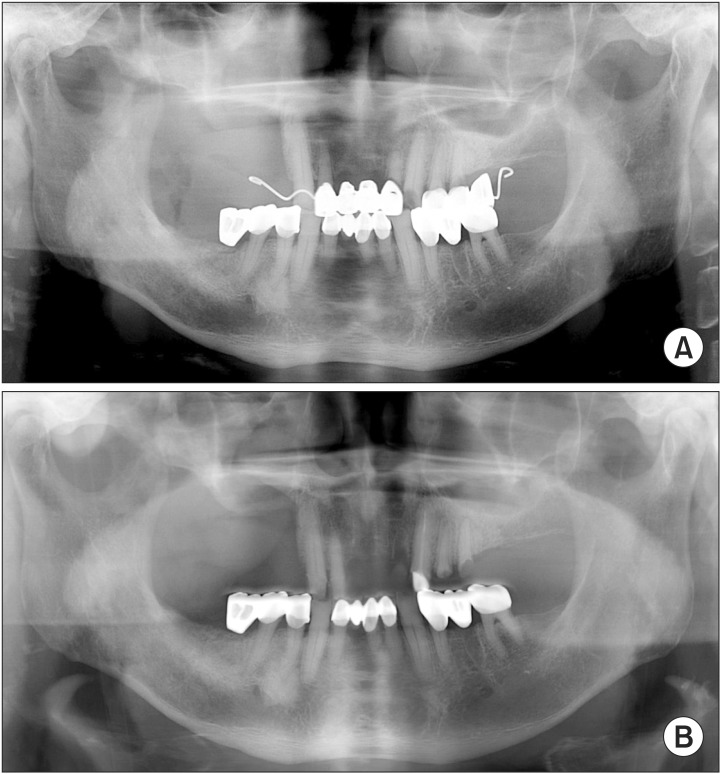
Upon a radiologic study, we found sequestrum formation in the #16 area, which had a well-defined margin, making it easily distinguishable4. The region extended beyond the alveolar bone into the right maxillary sinus (Fig. 2), and a bone scan image showed increased intake in the right maxillary area.(Fig. 3)
Because there was an exposed bone lesion that extended to the right maxillary sinus, the patient was diagnosed with stage 3 BRONJ according to the AAOMS classification criteria2, and conservative treatment was primarily given.
The laboratory tests showed carboxy-terminal collagen crosslinks (CTX) in serum 0.174 ng/mL, vitamin D 11.9 ng/mL (reference value, 30.1-100.0 ng/mL), and serum osteocalcin 1.4 ng/mL (reference value, 5-25 ng/mL). After an endocrinology consult, it was confirmed that surgical intervention would be possible and vitamin D (0.5 µg, once a day, Onealfa Tab.; Ilsung Pharmaceuticals, Seoul, Korea) was prescribed.
After admission, intravenous antibiotics (four times a day, Fullgram Injection 300 mg; Samjin Pharm, Seoul, Korea) were given. We performed a surgical operation including sequestrum resection, partial maxillectomy, and extraction of the first and second premolars. The defect area was covered with a buccal fat pad flap.(Fig. 4) In order to relieve sinus symptoms, mucolytics and nasal decongestants were administered for two weeks following surgery.
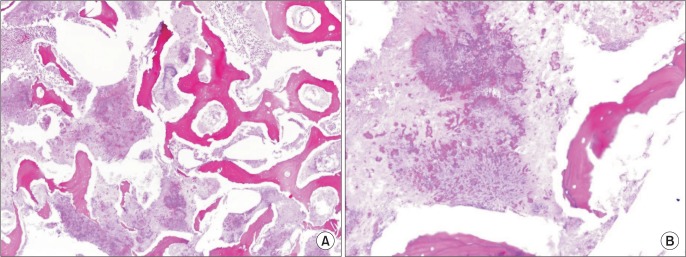
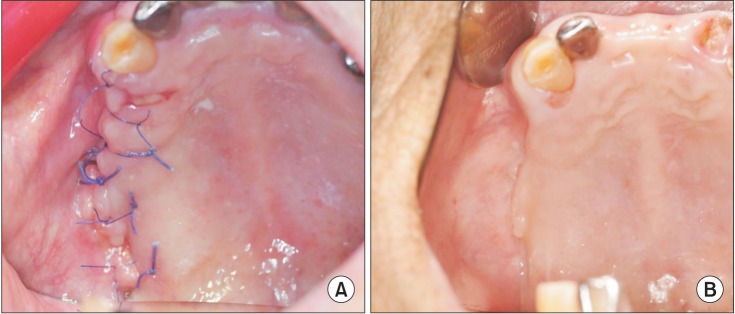
Biopsy results confirmed actinomycotic osteomyelitis4.(Fig. 5) Postoperative healing was uneventful. After discharge, regular follow-up visits were conducted. There were no signs of recurrence and a clean and fully healed mucosa was observed in the intraoral picture taken sixty days postoperatively.(Fig. 6) The postoperative X-ray showed a clearly resected bone margin and an uneventfully healed maxilla.(Fig. 7)
Underlying diseases related to BRONJ include primarily malignant tumors, multiple myeloma and osteoporosis3. In this case, the patient's past medical history was significant for malignancy and osteoporosis, although osteoporosis was the primary indication for bisphosphonate treatment.
BRONJ is more common in females because menopause is the main etiology of osteoporosis. The male-to-female incidence ratio of BRONJ is about 4:6, regardless of the underlying diseases56. In our research from 2007 to 2014, there were 11 male and 213 female BRONJ patients. In accordance with this, a medical history including osteoporosis is likely to be overlooked more frequently in male patients before dental treatment. In this case, osteoporosis developed as a result of aging and hypogonadism after receiving an orchiectomy and the patient was treated with alendronate (Fosamax Tab. 70 mg) for about four years. In this condition, bone turnover activity is suppressed and the tooth extraction was performed indiscriminately. We conclude that BRONJ might have developed through this serial pathway.
Osteoporosis in males can occur due to a variety of reasons, such as old age, steroid abuse, alcoholism and hypogonadism7. Among these, hypogonadism is a commonly occurring consequence associated with orchiectomy7. Because complications such as pelvic fracture may frequently occur with hypogonadism, bisphosphonate therapy is necessary for this group of patients. When a dentist first meets these patients, a careful medical history is required as there is a risk of BRONJ. Osteoporosis in males tends to be overlooked or underestimated compared with females. Only 10% of male patients receive treatment for osteoporosis due to lack of awareness8, and the incidence of osteoporosis tends to increase more significantly in males over 70 years of age compared with females7.
Cases of BRONJ affecting the maxilla are rarer than those in the mandible9. However, in the case of advanced maxillary lesions, sinusitis or intracranial complications can occur1011. As most of these patients are elderly and many have a history of variable diseases, they require prompt treatment.
In many BRONJ cases, infections and recurrence may occur; in other words, the healing process is often compromised for many reasons. Because of impaired vascularity, the healing alveolus may be vulnerable to bacterial infections. In order to reduce exposure to bacterial infections, primary closure is important12. We performed a sequestrectomy and partial maxillectomy, and primary closure with a buccal fat pad flap. The buccal fat pad flap is useful to cover soft tissue defects in the posterior maxillary regions, as well as other open wounds of the oral and maxillofacial regions, because it has high vascularity and adipose tissue stem cells which accelerate the healing process of necrotic lesions13.
In this case, after successful primary closure with local mucosa and the buccal fat pad flap, the wound healed uneventfully.
Notes
References
1. Park YD, Kim YR, Kim DY, Chung YS, Lee JK, Kim YG, et al. Awareness of Korean dentists on bisphosphonate related osteonecrosis of the jaws: preliminary report. J Korean Assoc Oral Maxillofac Surg. 2009; 35:153–157.
2. Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, et al. American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw: 2014 update. J Oral Maxillofac Surg. 2014; 72:1938–1956. PMID: 25234529.
3. Ikebe T. Pathophysiology of BRONJ: drug-related osteoclastic disease of the jaw. Oral Science International. 2013; 10:1–8.

4. Ohe JY, Kwon YD, Kim YG, Lee BS, Yoon BW, Choi BJ. Features of histopathologic and radiographic findings in bisphosphonate-related osteonecrosis of jaw: clinical review. J Korean Assoc Oral Maxillofac Surg. 2008; 34:550–554.
5. Assaf AT, Smeets R, Riecke B, Weise E, Gröbe A, Blessmann M, et al. Incidence of bisphosphonate-related osteonecrosis of the jaw in consideration of primary diseases and concomitant therapies. Anticancer Res. 2013; 33:3917–3924. PMID: 24023329.
6. Tsao C, Darby I, Ebeling PR, Walsh K, O'Brien-Simpson N, Reynolds E, et al. Oral health risk factors for bisphosphonate-associated jaw osteonecrosis. J Oral Maxillofac Surg. 2013; 71:1360–1366. PMID: 23582590.

7. Gielen E, Vanderschueren D, Callewaert F, Boonen S. Osteoporosis in men. Best Pract Res Clin Endocrinol Metab. 2011; 25:321–335. PMID: 21397201.

8. Kaufman JM, Reginster JY, Boonen S, Brandi ML, Cooper C, Dere W, et al. Treatment of osteoporosis in men. Bone. 2013; 53:134–144. PMID: 23201268.

9. Maurer P, Sandulescu T, Kriwalsky MS, Rashad A, Hollstein S, Stricker I, et al. Bisphosphonate-related osteonecrosis of the maxilla and sinusitis maxillaris. Int J Oral Maxillofac Surg. 2011; 40:285–291. PMID: 21163624.

10. Choi BJ, Kwon YD, Lee BS, Walter C, Nawas BA. Maxillary sinusitis as a complication of oral bisphosphonate related osteonecrosis of the jaw: a case report. J Korean Assoc Oral Maxillofac Surg. 2009; 35:39–40.
11. Khan AM, Sindwani R. Bisphosphonate-related osteonecrosis of the skull base. Laryngoscope. 2009; 119:449–452. PMID: 19235747.

12. Rotaru H, Kim MK, Kim SG, Park YW. Pedicled buccal fat pad flap as a reliable surgical strategy for the treatment of medication-related osteonecrosis of the jaw. J Oral Maxillofac Surg. 2015; 73:437–442. PMID: 25544302.

13. Farré-Guasch E, Martí-Pagè C, Hernádez-Alfaro F, Klein-Nulend J, Casals N. Buccal fat pad, an oral access source of human adipose stem cells with potential for osteochondral tissue engineering: an in vitro study. Tissue Eng Part C Methods. 2010; 16:1083–1094. PMID: 20078198.
Fig. 1
Initial intraoral picture. The sequestrum was seen in the right upper molar area surrounding with edematous and erythematous gingiva.

Fig. 2
Preoperative radiography. A. Panoramic X-ray. B-E. Cone-beam computed tomography (CBCT). In radiologic study, the sequestrum formation was seen on #16 area with well-defined margin extended beyond the alveolar bone reaching to the right maxillary sinus. The CBCT images show increased haziness on the right maxillary sinus.
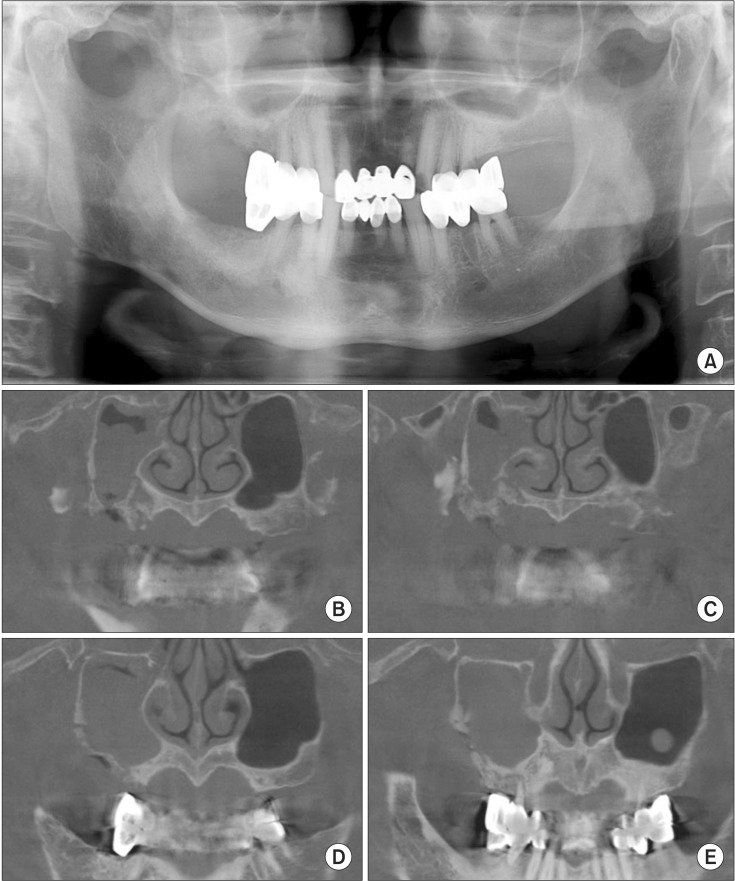
Fig. 4
Intraoperative pictures. A. The excised specimen of right maxilla. B-D. Surgical procedure. After partial maxillectomy, we can see clear margin (B). To close the wound primarily, we use the buccal fat pad flap (C) and suture (D).
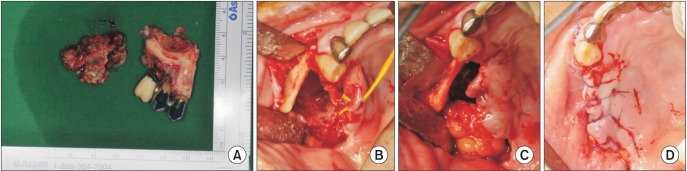
Fig. 5
Microscopic pictures of specimen (H&E staining, A: ×40, B: ×200). Sample shows the sulfur granule and bacterial colony, which is a histologic character of Actinomyces.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download