Abstract
Extraction of an impacted third molar is one of the most frequently performed techniques in oral and maxillofacial surgery. Surgeons can suffer numerous external injuries while extracting a tooth, with percutaneous injuries to the hand being the most commonly reported. In this article, we present a case involving a percutaneous injury of the surgeon's femoral region caused by breakage of the fissure bur connected to the handpiece during extraction of the third molar. We also propose precautions to prevent such injuries and steps to be undertaken when they occur.
The majority of tooth extraction procedures are performed using a handpiece accompanied by a thin bur to remove both the tooth and the bone. Several articles have reported on the risk of percutaneous injuries to the surgeon caused by the bur, and injuries to the hand are the most commonly reported123.
In many cases, when the surgeons use the elevator to dislocate the third molar, they must stand beside the patient. Thus, due to the proximity of the handpiece to the surgeon's leg, the bur can accidently penetrate the lower limb, leading to an external injury. This report presents one such case and considers the precautions needed to avoid similar accidents.
A 24-year-old male patient with no systemic medical history visited the Department of Oral and Maxillofacial Surgery of Wonkwang University Daejeon Dental Hospital (Daejeon, Korea) because of discomfort in his mandibular third molar. The tooth was extracted by creating an envelope flap and exposing the tooth and the bone, and a fissure bur connected to a handpiece was used to remove the bone of patient. After performing luxation using the elevator to dislocate the tooth, the surgeon, who was in a standing position, turned his body to pick up another instrument. At that moment, because the location of handpiece in a fixed upright position at the front of the instrument tray, the fissure bur broke and penetrated the surgeon's right femoral region. The handpiece was immediately removed, but the head of the bur was not found. Once the surgeon finished extracting the patient's tooth, the injured area was disinfected with potadine ointment (povidone iodine 450 g/bottle.; Samil, Seoul, Korea).
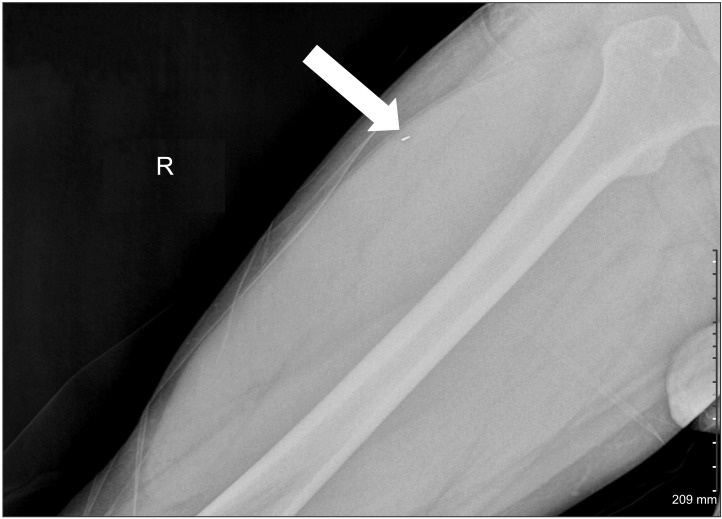
Radiographs of the right femoral region were then obtained at various angles to determine the location of the head of the bur, which was found in the upper medial area of the right vastus lateralis muscle.(Fig. 1) Under local anesthesia, a 1-cm incision was made to verify the radiographic findings, and the bur was removed.(Fig. 2) Subsequently, the area was dressed with potadine ointment and sutured using 5-0 nylon sutures. To prevent tetanus and bacterial infection, intramuscular Hyper-TET Injection (Green Cross, Yongin, Korea) was administered, and antibiotics and analgesics were also administered for 3 days. Daily wound dressing was also performed for 10 days, and the treatment regimen was concluded with stitch removal. Approximately 1 month after the incident, no postoperative complications had been observed.
Occupational injuries caused by sharp instruments such as needles, burs, blades and surgical wires occur frequently among dentists. Previous studies have described the danger of percutaneous injuries to the hands and fingers of both the patient and the surgeon due to the tools used during dental treatment. However, percutaneous injuries caused by burs have rarely been reported. Cleveland et al.2 reported in 1995 the percentage of percutaneous injuries associated with dental tools: endodontic files 1%, utility knives 5%, burs 2%, explorers 2%, needles 1%, pliers 1%, excavators 1%, and other instruments 1%. Also in 2007, a target study conducted with dental healthcare personnel reported that the percentage of percutaneous injuries associated with needles is 46%, burs 10%, scalpels 7%, scalers 5%, elevators 5%, explorers 4%, wires 3%, and other instruments 20%4. Even though instrument breakage in surgical procedures involving the bur is common5, Carlton et al.6 noted that puncture wounds occurred frequently in patients during oral maxillofacial surgery, but the proportion of such wounds occurring in the surgeon is low. To the best of our knowledge, this article is the first to report a case in which the surgeon suffered a percutaneous injury in the femoral area due to bur breakage.
Complications from cutaneous penetration of burs include infections through direct contact with patient blood, including viral transmission (e.g., human immunodeficiency virus, hepatitis B and C viruses) and tetanus. A puncture wound from contaminated instruments carries the same health risks as a human bite7. In this case, the injury was not serious, as it did not result in a severe soft tissue laceration, and the bur did not damage the bone or move to other parts of the body. We should have performed serological tests immediately, as blood-borne pathogens can lead to cross-infection. However, the patient didn't have a relevant medical history, so we thought that serological tests were not necessary. If a similar incident resembling our report occurs in the future, blood tests should be considered. The main treatment method in cases involving penetration of foreign substances is to completely remove the debris and to provide prophylaxis against potential infections with antibiotic treatment8, as well as through tetanus immunoglobulin shots9.
Similar to the case described in this report, numerous dentists experience light abrasions from the scaler tip because of the relatively close location of the dentist's chair to the patient. Although changing the design of the handpiece delivery system to that of the European dental unit (Continental Dental Unit; Adec Inc., Bristol, IN, USA) could help prevent such injuries, several studies have reported no difference in the incidence of percutaneous injuries associated with these systems10. In addition, the main reason for bur breakage is the reuse and repeated disinfection of the instrument5. Therefore, it is important to avoid overuse of the equipment. The most important factor, however, is to focus on prevention and care. Through this article, we hope to have provided guidance for oral and maxillofacial surgeons regarding the procedures and precautions necessary to avoid (or care for) accidental penetration of the femoral region with a piece of equipment, which can occur during extraction of the third molar.
References
1. Siew C, Gruninger SE, Miaw CL, Neidle EA. Percutaneous injuries in practicing dentists. A prospective study using a 20-day diary. J Am Dent Assoc. 1995; 126:1227–1234. PMID: 7560582.
2. Cleveland JL, Lockwood SA, Gooch BF, Mendelson MH, Chamberland ME, Valauri DV, et al. Percutaneous injuries in dentistry: an observational study. J Am Dent Assoc. 1995; 126:745–751. PMID: 7797730.

3. Callan RS, Caughman F, Budd ML. Injury reports in a dental school: a two-year overview. J Dent Educ. 2006; 70:1089–1097. PMID: 17021289.

4. Cleveland JL, Barker LK, Cuny EJ, Panlilio AL. National Surveillance System for Health Care Workers Group. Preventing percutaneous injuries among dental health care personnel. J Am Dent Assoc. 2007; 138:169–178. PMID: 17272371.

5. Manikandhan R, Anantanarayanan P, Mathew PC, Kumar JN, Narayanan V. Incidence and consequences of bur breakage in orthognathic surgery: a retrospective study with discussion of 2 interesting clinical situations. J Oral Maxillofac Surg. 2011; 69:2442–2447. PMID: 21665345.

6. Carlton JE, Dodson TB, Cleveland JL, Lockwood SA. Percutaneous injuries during oral and maxillofacial surgery procedures. J Oral Maxillofac Surg. 1997; 55:553–556. PMID: 9191635.

7. Fux Noy A, Shapira J. A percutaneous injury by a contaminated instrument is a human bite equivalent. Int J Paediatr Dent. 2011; 21:74–76. PMID: 20731737.

8. Motamedi MH. Primary treatment of penetrating injuries to the face. J Oral Maxillofac Surg. 2007; 65:1215–1218. PMID: 17517308.

9. Mallick IH, Winslet MC. A review of the epidemiology, pathogenesis and management of tetanus. Int J Surg. 2004; 2:109–112. PMID: 17462232.

10. Harte J, Davis R, Plamondon T, Richardson B. The influence of dental unit design on percutaneous injury. J Am Dent Assoc. 1998; 129:1725–1731. PMID: 9854923.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download