Abstract
Benign fibrous histiocytoma (FH) is a benign tumor composed of fibroblasts and histiocytes in varying proportions. This tumor is usually found in adult extremities but rarely occurs in deep soft tissues of the oral cavity. As it is difficult to diagnose with physical and radiologic exams, deep benign FH can only be diagnosed by histopathology. We report a case of a 36-year-old female patient who came to our department with painless swelling in the right buccal mucosa. This case report reviews the clinical, radiological, and histological aspects of this tumor.
Go to : 
Fibrous histiocytoma (FH), first reported by Kauffman and Stout in 1961, is composed of fibroblasts and histiocytes in varying proportions12. FH can be benign or malignant, and malignant FH is usually found in the lower extremities, upper extremities, and retroperitoneum, in order of frequency. Malignant FH in the head and neck area accounts for less than 10% of all malignant FH, and less than 0.5% of all malignant head and neck tumors34. The treatment of choice for malignant FH is surgical excision, and obtaining a clear surgical margin is crucial due to its survival benefit235. Benign FH is usually found in adult extremities, the head and neck area, and the retroperitoneum. However, the occurrence of benign FH in the oral cavity is rare67. Benign FH can be categorized into superficial and deep forms. Deep benign FH is very rare, comprising less than 5% of all benign FH tumors6. We encountered a patient with painless swelling in the right buccal mucosa. Based on magnetic resonance imaging (MRI), we suspected that the lesion was a minor salivary gland tumor or a neurofibroma. Excisional biopsy was performed and the intraoperative mass appeared to be a pleomorphic adenoma. The final pathologic diagnosis was deep benign FH. This case report reviews the clinical, radiological, and histological aspects of this tumor.
Go to : 
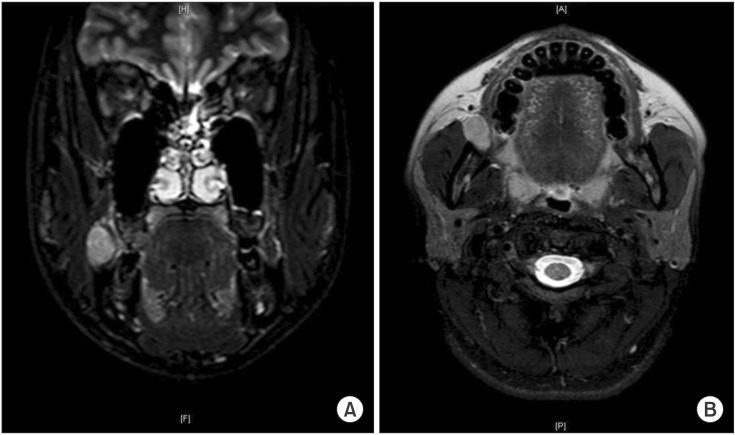
A 36-year-old female patient came to our department with painless swelling in the right buccal mucosa which had started 3 weeks previously. There was no specific medical history or history of trauma. A palpable mass was found at the right buccal mucosa, having an induration consistency without tenderness on palpation. However, no gross abnormality was found by observation. After the physical examination, we suspected a lipoma. MRI revealed a well-marginated 1.8 cm enhancing ovoid lesion in the right buccal space.(Fig. 1)
An excisional biopsy was performed under local anesthesia. An incision was created over the mass at the buccal mucosa and extraoral pressure was applied with a finger during the dissection. A well-encapsulated 2.3×1.3×1.3 cm mass was easily separated and removed.(Fig. 2, 3) It appeared to be a pleomorphic adenoma based on the intraoperative findings.
Histopathologic examination showed predominantly spindle cells and areas of myxoid stroma.(Fig. 4. A) A high power view revealed a prominent storiform pattern of fibroblastic spindle cells with focal bundles of dense collagen, foam cells, and multinucleated giant cells.(Fig. 4. B)
The patient is being regularly followed-up, and there has been no sign of recurrence during 6 months of follow-up.
Go to : 
Benign FH is divided into superficial benign FH and deep benign FH, and usually occurs in the extremities of adults6. It has been clinically reported on under several names4. Deep benign FH accounts for less than 5% of all benign FH tumors and occurs predominantly in males in their 2nd to 4th decade in the lower extremities and head and neck areas, in order of frequency67.
In most cases, benign FH is a painless mass without symptoms and is well-marginated8910. It is difficult to diagnose deep benign FH with only physical examination.
Deep benign FH rarely occurs in the oral cavity. For this reason, it is difficult to distinguish at first sight and is easily misdiagnosed as a benign tumor such as fibroma or lipoma, which are easily found in the oral cavity. Imaging of deep benign FH shows nonspecific signal intensities on computed tomography and MRI11. As it is difficult to diagnose with physical and radiologic exams, deep benign FH can only be diagnosed by its histopathology.
Complete resection of deep benign FH is recommended since it has a higher recurrence rate after operation than other forms of FH. The prognosis of patients with benign FH is usually excellent. Less than 5%-10% recurrence has been reported in the case of large tumors or positive margins after operation12. As the reported mean time interval between operation and recurrence is 2 years13, follow-up for more than 2 years is suggested. No metastasis has been reported, and radiation therapy and chemotherapy are rarely needed for the management of benign FH.
Go to : 
References
1. Kauffman SL, Stout AP. Histiocytic tumors (fibrous xanthoma and histiocytoma) in children. Cancer. 1961; 14:469–482. PMID: 13751857.

2. Min BI, Kim JW, Kim YK. The clinicopathologic study of malignant fibrous histiocytoma. J Korean Assoc Oral Maxillofac Surg. 1988; 14:77–81.
3. Hardison SA, Davis PL 3rd, Browne JD. Malignant fibrous histiocytoma of the head and neck: a case series. Am J Otolaryngol. 2013; 34:10–15. PMID: 22999710.

4. Blitzer A, Lawson W, Biller HF. Malignant fibrous histiocytoma of the head and neck. Laryngoscope. 1977; 87:1479–1499. PMID: 197358.

5. Spector GJ, Ogura JH. Malignant fibrous histiocytoma of the maxilla. A report of an unusual lesion. Arch Otolaryngol. 1974; 99:385–387. PMID: 4364984.

6. Fletcher CD. Benign fibrous histiocytoma of subcutaneous and deep soft tissue: a clinicopathologic analysis of 21 cases. Am J Surg Pathol. 1990; 14:801–809. PMID: 2167613.
7. Gray PB, Miller AS, Loftus MJ. Benign fibrous histiocytoma of the oral/perioral regions: report of a case and review of 17 additional cases. J Oral Maxillofac Surg. 1992; 50:1239–1242. PMID: 1328571.

8. Pandey NK, Sharma SK, Banerjee S. A rare case of fibrous histiocytic tumor of the tongue. Indian J Surg. 2013; 75(Suppl 1):1–5. PMID: 24426494.

9. Weiss SW, Enzinger FM. Malignant fibrous histiocytoma: an analysis of 200 cases. Cancer. 1978; 41:2250–2266. PMID: 207408.
10. Huh HY, Jin WJ, Shin HK, Kim OW. A case report of malignant fibrous histiocytoma of the maxilla. J Korean Assoc Oral Maxillofac Surg. 1988; 14:139–145.
11. Machiels F, De Maeseneer M, Chaskis C, Bourgain C, Osteaux M. Deep benign fibrous histiocytoma of the knee: CT and MR features with pathologic correlation. Eur Radiol. 1998; 8:989–991. PMID: 9683707.

12. Ferrari Parabita G, Viva E, Derada Troletti G, Girardi E. Rare case of a fibrous histiocytoma located in the parotid. Minerva Stomatol. 1982; 31:693–696. PMID: 6298590.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download