Abstract
Objectives
The purpose of this study is to retrospectively evaluate the postoperative complication rates for absorbable type-I collagen sponge (Ateloplug; Bioland) use in third molar extraction.
Materials and Methods
From January to August 2013, 2,697 total patients undergoing third molar extraction and type-I collagen sponge application in the Department of Oral and Maxillofacial Surgery at Yonsei University Dental Hospital (1,163 patients) and Dong-A University Hospital (1,534 patients) were evaluated in a retrospective study using their operation and medical records.
Results
A total of 3,869 third molars in 2,697 patients were extracted and the extraction sockets packed with type-I collagen sponges to prevent postoperative complications. As a result, the overall complication rate was 4.52%, with 3.00% experiencing surgical site infection (SSI), 1.14% showing alveolar osteitis, and 0.39% experiencing hematoma. Of the total number of complications, SSI accounted for more than a half at 66.29%.
Extraction of third molars is a routine procedure for acute or chronic pericoronitis, tumors or cystic lesions, periodontal problems, and dental caries. Accurate understanding of the third molar status and proper surgical technique is necessary to prevent postoperative complications. Despite these efforts, immediate postoperative sequelae such as bleeding, pain, swelling, and trismus often occur and may result in more serious postoperative complications like surgical site infection (SSI), alveolar osteitis (AO), hematoma, and paresthesia. These complications are mostly transient and the incidence rates are low, but these complications can inconvenience the patients' daily social lives and may be costly and timeconsuming with the necessary additional visits.
Several risk factors associated with complications after extraction include age, gender, medication, site of extraction, smoking, previous infection, poor oral hygiene, anesthesia, and the surgeon's experience1,2,3,4,5,6. Previous reports suggest the use of additional interventions including local application of antimicrobials, antifibrinolytics, and anti-inflammatory medications to the extraction socket to prevent or minimize postoperative complications7,8. Type-I collagen sponges are also known to be useful in minimizing postoperative complications due to their effect on new granulation tissue formation, blood clot stabilization, and wound protection9. Thus, many maxillofacial surgeons have used the bullet-shape collagen sponges to obtain favorable results. Although there were several reports that collagen sponges can prevent tooth extraction complications9,10, the number of these previous reports are limited, and more studies are indicated in a larger number of patients. Thus, we aimed to evaluate the rate of complications after using absorbable type-I collagen sponges following third molar extractions, and to discuss the effectiveness of the absorbable collagen sponge insertion in minor oral surgery.
This study followed the Declaration of Helsinki on medical protocol and ethics, and was approved by the regional ethical review boards of Yonsei University Dental Hospital (IRB No. 2-2014-0009) and Dong-A University Hospital (IRB No. 14-144). This retrospective study was designed to evaluate postoperative complications after using type-I collagen sponges (Ateloplug; Bioland, Cheonan, Korea) following third molar extractions. The patients who had undergone collagen sponge insertion into the extraction socket in the Department of Oral and Maxillofacial Surgery from January to August in 2013 were included in this study, and a total 2,697 patients' charts (1,163 patients from Yonsei University Dental Hospital and 1,534 from Dong-A University Hospital) were reviewed.
Extraction was performed under local or general anesthesia, and the type-I collagen plugs were placed into the extraction sockets before wound closure. Extraction procedures were organized by surgical extractions and simple extractions. Surgical extractions were performed with a full-thickness mucoperiosteal flap reflection and odontomy, ostectomy using elevators, whereas the simple extractions were performed using elevators and forceps without flap elevation. The patient's extraction site was assessed when the patient visited the clinic for stitches removal or postoperative discomfort. The presence and the rate of each complication related to collagen plug application, including SSI, AO, and hematoma, was surveyed. SSI was diagnosed when pain at the extraction site was accompanied by suppurative exudate1. AO was clinically diagnosed by the development of severe, throbbing pain 2 to 5 days after the extraction, and the partial or complete loss of the blood clot1,3. Surgical complications irrelevant to collagen plug insertion, such as paresthesias, sinus perforation, and mandibular fracture were excluded from this study. PASW Statistics version 18.0 software (IBM Co., Armonk, NY, USA) was used for statistical analysis, using the Pearson chi-square test.
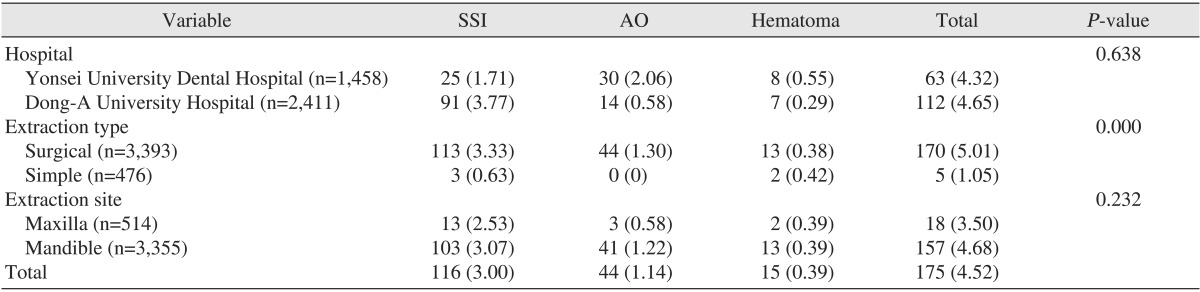
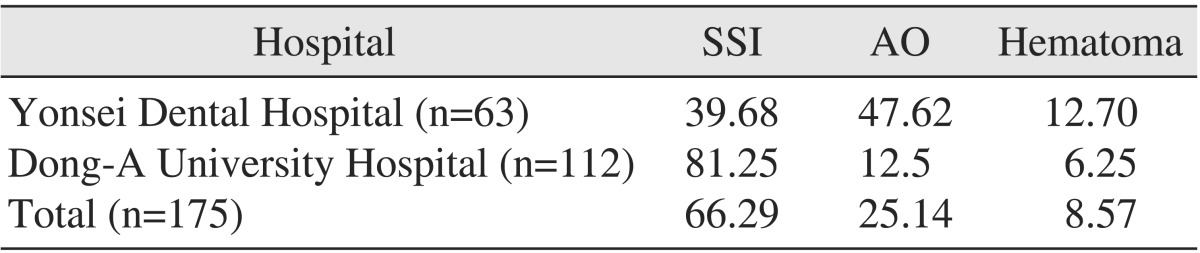
A total of 3,869 third molars (514 maxillary third molars and 3,355 mandibular third molars) from 2,697 patients were extracted, and the extraction sockets were packed with type-I collagen plugs. Of these patients, 1,458 molars from 1,163 patients were from Yonsei University Dental Hospital and 2,411 molars from 1,534 patients were from Dong-A University Hospital. Surgical extraction was performed on 3,393 cases, while the remaining 476 cases were treated with simple extraction. The overall complication rate associated with collagen plug insertion was 4.52% (175 teeth). Respectively, 116 subjects (3.00%), 44 subjects (1.14%), and 15 subjects (0.39%) developed SSI, AO, and hematoma. Comparing the two hospitals, the total complication rates were similar at 4.32% (Yonsei University Dental Hospital) and 4.65% (Dong-A University Hospital) (P=0.638; P>0.05). However, the complication ratios showed marked differences, especially for SSI and AO (P=0.000; P<0.05). At Yonsei University Dental Hospital, the incidence of SSI and AO were 1.71% and 2.06%, respectively. In contrast, the complication rates at Dong-A University Hospital were 3.77% and 0.58%. Notably, the complication rates were significantly different according to the extraction method, with surgical extraction (5.01%) resulting in a much higher rate than simple extraction (1.05%) (P=0.000; P<0.05). The extraction site was also compared, showing a complication rate of 3.50% for maxillary extractions, and 4.68% for mandibular extractions, which were not significantly different (P=0.232; P>0.05).(Table 1) When assessing the total number of complications, SSI accounted for more than half, at 66.29%. However, a single hospital study at Yonsei University Dental Hospital showed that AO accounted for almost half of the complications at a rate of 47.62%, while SSI accounted for more than half of the complications.(Table 2)
The purpose of this retrospective study was to evaluate the efficacy of type-I collagen sponge application after third molar extraction by assessing the rate of complications, including SSI, AO, and hematoma, to explore whether collagen sponges prevent these complications. The total complication rate was 4.52%, of which, 3.00% were SSI, 1.14% were AO, and 0.39% were hematomas.
According to previous studies, the complication rates after third molar extraction had been reported in various numbers. Reported rates of SSI vary from 0.8% to 4.2%2,3,11 and 0.9% to 4.3%1,4,12 in each study. Chiapasco et al.12 reported that mandibular extractions result in a higher rate of SSI than maxillary extractions, with rates of 1.5% and 0.2%, respectively. In the study of Bui et al.4, the lowest rate of SSI was reported at 0.8%, and 94.3% of those patients received postoperative antibiotics. The incidence of SSI in our study was 3.00%, which is consistent with previous studies. The AO rates reported in previous studies were more widely spread, 0.3% to 26%3, 1% to 3%4, and 0.5% to 68.4%1,13, and the AO rate has been reported up to 30% in cases of impacted mandibular third molars4. In our study, the AO rate was relatively low, at 1.14%, which may be explained by the effects of the collagen sponge.
Besides, the rates of SSI and AO had variation between two hospitals with 1.71% to 3.77% and 0.58% to 2.06%. These wide variations may have been due to different diagnostic criteria and various conditions, including the patient's status, surgical technique, and surgeon experience. When comparing the surgical techniques in this study, the minimally traumatic procedure may result in the lowest complications, also in case of collagen sponge insertion (P=0.000; P<0.05). Hematoma formation was rarely mentioned in other studies, but it could be associated with common complications, especially bleeding and hemorrhage, which ranged from 0.2% to 5.8%3. In this study, bleeding was treated as a normal postoperative sequelae and not included as a postoperative complication.
After extraction, the extraction socket fills with blood clot and goes through inflammation, epithelialization, fibroplasia, and remodeling. The gingival tissue grows into the blood clot-filled socket, thus strengthening the fibrin-covered clot to be fixed to the alveolus. Fibroplasia into the clot continues with the cellular elimination of fibrin and blood debris. Then, granulation tissue gradually replaces the clot7. Extraction socket blood clots act as a scaffold for angiogenesis and fibroplasia. Therefore, the maintenance of clots during the healing period may be one of the most important factors in preventing inflammatory complications. With this information, various attempts have been made to stabilize the blood clot and to accelerate the healing process by way of systemic and local administration of medication. Compared to systemic medication, topical application to the extraction socket has the advantages of minimizing systemic side effects and reaching a greater concentration in a shorter amount of time. Local application of antimicrobials, antifibrinolytics, and anti-inflammatory medications has been recommended. However, the insertion of topical substances should be performed with follow-up for undesirable local reactions7,8.
Collagen is one of the most common substances for topical application in extraction sockets because it has extensive effects on hemostasis, biocompatibility, biodegradability, and bone conductivity. Type I collagen is a fibrillar collagen, and is the main component of the extracellular matrix. It is also a natural matrix for osteoblast migration, and has been used for both soft tissue healing and hard tissue reconstruction14. In a previous study of collagen sponge application to the extraction socket, the collagen sponge appeared to be replaced by natural tissue and matured in the process of its resorption10. Ateloplug is an absorbable collagen sponge extracted from pig dermis and is composed of 100% type I collagen to minimize antigenicity, and is cross-linked by heat treatment for biocompatibility. Due to its bullet-shaped matrix, it is easily placed in the extraction socket and provides excellent hemostasis by physical compression immediately after extraction. Also, it accelerates tissue regeneration and enhances natural healing by protecting the extraction site from the inflow of food and debris. Not only does the collagen sponge preserve the capacity of the blood clot, but it also prevents soft tissue collapse into the socket, which lacks the support of alveolar bone9.
Thus, type-I collagen plugs are indicated for filling extraction wounds to enhance hemostasis, facilitate granulation tissue formation, and protect the wound surface. Collagen sponges also reduce swelling and pain postoperatively. In our study, the use of collagen plugs in third molar extractions resulted in relatively low complication rates compared to previous studies on general conditions, although these differences were not significant. To manage extraction complications, the risk factors associated with complications should be assessed prior to extraction. Most complications of third molar extraction are inflammatory complications, such as SSI and AO, and they are thought to be associated with the surgeon's level of experience15. However, these risk factors are often not modifiable by the surgeons. Thus, the risk factors that cannot be modified by surgeons, like patient's sex, age, and third molar impaction level, should be fully evaluated, and surgeons should take additional preventive measures into account according to the severity of the risk factors. In an effort to control complications after third molar extraction (e.g., perioperative antibiotics, modifications of surgical technique), the application of absorbable collagen sponges should be considered.
To minimize complications after third molar extraction, the topical application of type-I collagen sponges in the extraction sockets could be a useful method due to its effectiveness in hemostasis, wound stabilization, and promotion of healing. The relatively low incidence of complications in this study supports the collagen sponge's effects. Therefore, in addition to the evaluation and control of risk factors associated with extraction, application of absorbable collagen sponges may also help prevent complications, and better results may be expected after third molar extractions.
References
1. Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: postoperative complications and their risk factors. J Can Dent Assoc. 2007; 73:325. PMID: 17484797.
2. Bloomer CR. Alveolar osteitis prevention by immediate placement of medicated packing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 90:282–284. PMID: 10982947.

3. Bouloux GF, Steed MB, Perciaccante VJ. Complications of third molar surgery. Oral Maxillofac Surg Clin North Am. 2007; 19:117–128. vii. PMID: 18088870.

4. Bui CH, Seldin EB, Dodson TB. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg. 2003; 61:1379–1389. PMID: 14663801.

5. Phillips C, White RP Jr, Shugars DA, Zhou X. Risk factors associated with prolonged recovery and delayed healing after third molar surgery. J Oral Maxillofac Surg. 2003; 61:1436–1448. PMID: 14663809.

6. Hwang JK, Kim KW. Complications of impacted third molar extraction: retrospective study. J Korean Assoc Oral Maxillofac Surg. 2010; 36:119–124.

7. Vezeau PJ. Dental extraction wound management: medicating postextraction sockets. J Oral Maxillofac Surg. 2000; 58:531–537. PMID: 10800909.

8. Alexander RE. Dental extraction wound management: a case against medicating postextraction sockets. J Oral Maxillofac Surg. 2000; 58:538–551. PMID: 10800910.

9. Konishi J, Miyamoto T, Miura A, Osaki K. An investigation into the wound healing action of the atelocollagen tooth extraction wound protection material (TRE-641) on tooth extraction site. J Jpn Soc Biomater. 1998; 16:266–275.
10. Niki H, Uchida H, Kubo H, Kakudo K, Shimizutani K, Koseki Y, et al. Computed tomographic examination of bone healing after placement of collagen sponge matrix in the tooth extraction site. J Osaka Odontol Soc. 2001; 64:369–374.
11. Haug RH, Perrott DH, Gonzalez ML, Talwar RM. The American Association of Oral and Maxillofacial Surgeons age-related third molar study. J Oral Maxillofac Surg. 2005; 63:1106–1114. PMID: 16094577.

12. Chiapasco M, Crescentini M, Romanoni G. Germectomy or delayed removal of mandibular impacted third molars: the relationship between age and incidence of complications. J Oral Maxillofac Surg. 1995; 53:418–422. PMID: 7699496.
13. Houston JP, McCollum J, Pietz D, Schneck D. Alveolar osteitis: a review of its etiology, prevention, and treatment modalities. Gen Dent. 2002; 50:457–463. PMID: 12448899.
14. Nam JW, Kim KW. The effects of atelo-collagen sponge insertion on the periodontal healing of second molars after impacted mandibular third molar extraction. J Korean Assoc Oral Maxillofac Surg. 2009; 35:112–119.
15. Chuang SK, Perrott DH, Susarla SM, Dodson TB. Risk factors for inflammatory complications following third molar surgery in adults. J Oral Maxillofac Surg. 2008; 66:2213–2218. PMID: 18940482.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download