Abstract
Objectives
This study investigated patients with oral and maxillofacial lacerations who visited the emergency room over a three-year period in an effort to determine the optimal treatment for these injuries.
Materials and Methods
This study examined 1,742 patients with oral and maxillofacial lacerations with 2,014 different laceration locations who visited the emergency room of Pusan National University Hospital (Busan, Korea) over three years, from January 2011 to December 2013. Patients were classified by sex, age, visit day, cause of injury, injury site, and the presence or absence of soft tissue and tooth injuries.
Results
The male to female ratio was 2.50:1. Patients under 10 years old were seen most frequently. Most emergency room visits were on weekends. Among intra-oral lacerations, the lip area was the most vulnerable site; among extra-oral lacerations, the chin area was most frequently injured. The most frequent etiology was a slip down. Most lacerations occurred without bone fracture or tooth damage.
Go to : 
The number of individuals who visit hospital emergency rooms (ERs) due to oral and maxillofacial lacerations continues to increase with the diversification of industry, the exposure of individuals to expanded human activities, and an increasing number of traffic accidents1. The oral and maxillofacial regions are exposed outwardly, and therefore, carry a high risk of trauma. If oral and maxillofacial lacerations are not managed adequately and immediately, they may lead not only to functional or esthetic disability, but also, at times, to more serious health concerns.
The types of oral and maxillofacial trauma can be classified into facial bone fractures, dento-alveolar trauma, and soft tissue injuries. Most related studies have been limited to hard tissue trauma, such as facial bone fracture and dento-alveolar trauma2. In contrast, soft tissue injuries, like facial lacerations, have neglected their studies3. However, laceration is a frequent clinical problem arising from oral and maxillofacial trauma that brings patients to the ER. According to a study by Singer et al.4, nearly 28% of all patients visiting the ER with lacerations had facial lacerations.
The facial area is different from other body areas, as it has rich blood supply, which reduces the risk of postoperative infection. However, due to the possibility of scarring, oral and maxillofacial lacerations can cause not only aesthetic problems, but also psychological issues5. Therefore, oral and maxillofacial laceration treatment requires prompt and accurate evaluation, depending on the location and extent of the damaged area.
A study on the frequency and causes of facial laceration would allow for a better understanding of the types of lacerations and their development, and would enable faster and more accurate diagnosis. This study included oral and maxillofacial laceration patients who visited the ER and investigate laceration types and trends to ensure effective treatment of future patients with facial lacerations.
Go to : 
This study included 1,742 patients with oral and maxillofacial lacerations with 2,014 different laceration locations, for which they visited the ER of Pusan National University Hospital (Busan, Korea) over three years, from January 2011 to December 2013. With the subjects' basic reference data accessed from their clinical charts and radiographs, patients were classified by sex, age, visit day, etiology of injury, injury site, and the presence or absence of soft tissue and tooth damage. Exclusion criteria included patients with a scalp laceration, and those who returned home or passed away without treatment.
This study was approved by the Institutional Review Board of Pusan National University Hospital (PNUH E-2015045).
Go to : 
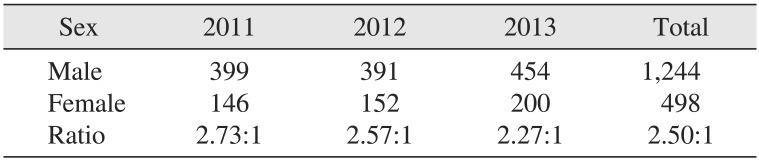
A total of 1,742 patients with oral and maxillofacial lacerations visited the ER of Pusan National University Hospital over three years. Each year, the number of male and female patients gradually increased. The ratio of male to female patients was 2.73:1 in 2011, and 2.27:1 in 2013, a slight decrease. Across time, the total male to female ratio was 2.50:1; 1,244 of the 1,742 patients were male and 498 patients were female.(Table 1)
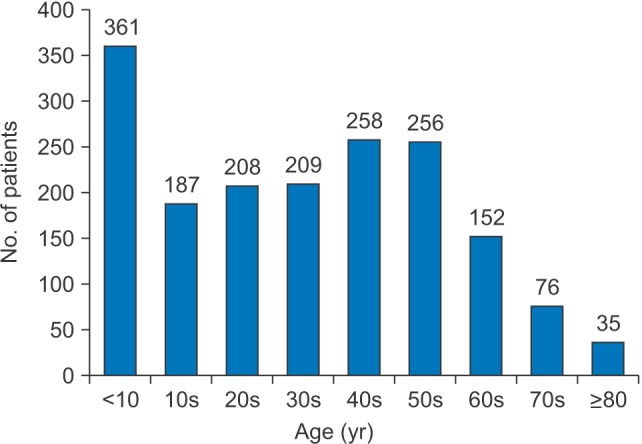
Patients under 10 years old were most frequently seen, comprising 20.7% of all patients, followed by those in their 40s at 14.8% and individuals in their 50s at 14.7%. Individuals over 80 years old were the least frequently seen, comprising 2.0% of all patients.(Fig. 1)
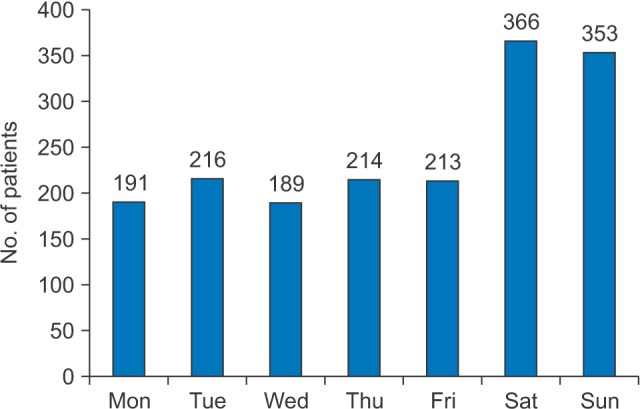
The distribution of patient visit days was as follows: the most patients sought treatment on Saturdays (21.0%), followed by Sundays (20.2%). Wednesdays received the fewest number of visits by individuals with oral and maxillofacial lacerations (10.8%).(Fig. 2)
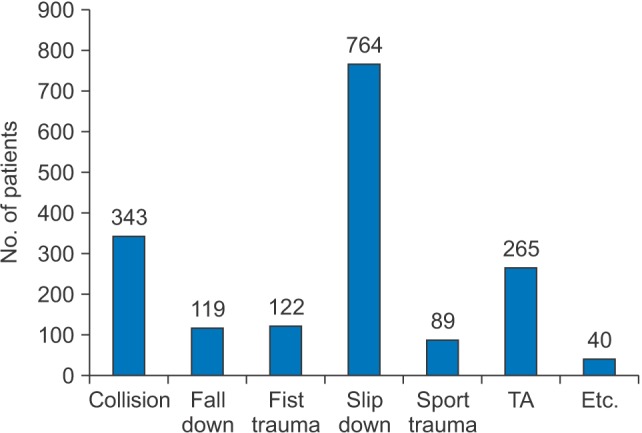
The distribution by trauma etiology showed that slip down was most common source of injury (43.9%), followed by collisions (19.7%) and traffic accident (15.2%), while sports trauma was the least common etiology (5.1%).(Fig. 3)
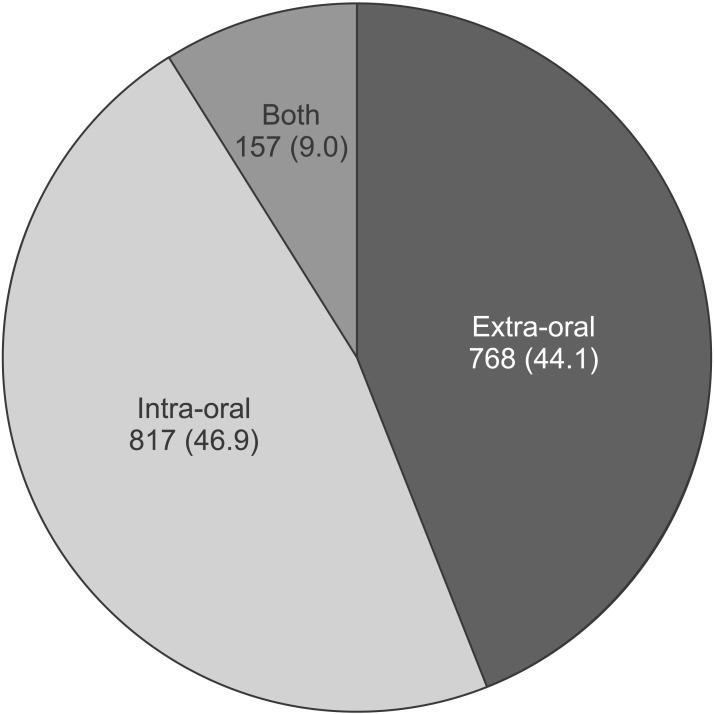
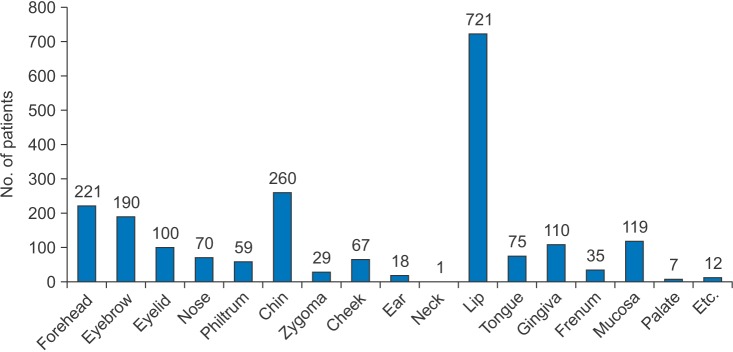
During the study period, 817 patients had intra-oral lacerations exclusively, a number slightly higher than the 768 patients with extra-oral lacerations exclusively; 157 patients had complex intra-oral and extra-oral lacerations.(Fig. 4) Complex laceration represents a case in which intra-oral and extra-oral lacerations occur simultaneously in a patient, and includes a penetrating wound. When the intra-oral laceration locations were further broken down, the lips were the most common laceration location, found in 721 patients. Among the extra-oral laceration cases, the chin was the most common location, found in 260 patients.(Fig. 5)
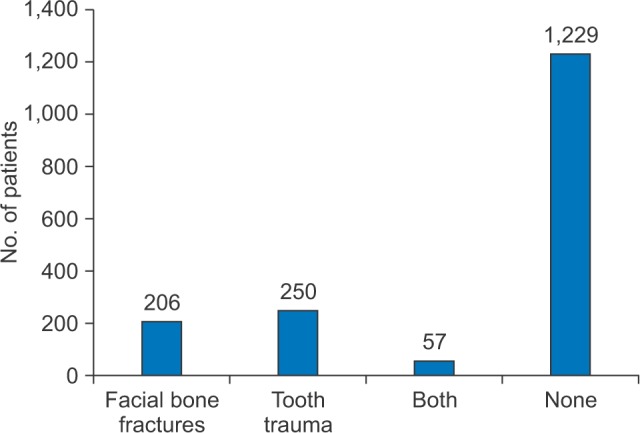
A total of 206 patients had a laceration accompanied by facial bone fractures, 250 experienced tooth injuries, and 57 patients experienced both. Laceration alone was found in 1,229 patients.(Fig. 6)
Go to : 
This study investigated the relationship of oral and maxillofacial lacerations to age, etiology, distribution, and other related locations among 1,742 individuals who visited the ER over a three-year period. A previous study noted that oral and maxillofacial area lacerations were the primary cause of ER visits. Kim et al.6 noted that soft tissue damage, tooth damage, facial bone damage, tooth pain, bleeding, infection, and temporomandibular joint luxation were the sequential causes of ER visits. Cho et al.7 reported the following were the sequential causes of ER visits: oral and maxillofacial area laceration, facial bone fracture, tooth damage, abscess, and bleeding. According to a study report by Jang et al.8, laceration with soft tissue damage was a common cause for ER visits, comprising 71% of ER visits; 21% sought treatment for abrasions and 7.4% for contusions.
Compared to facial bone fractures related to the study of Kim et al.9, underwent the same period, in the sex distribution of oral and maxillofacial laceration, the male to female ratio was 2.50:1, with 1,244 male subjects and 498 female subjects. Over three years, the male-to-female ratio decreased, due to the increase in the number of female patients. In the case of fracture patients, the male-to-female ratio was 4.31:1, higher than the overall 2.50. It appears that men are exposed to more external injury than women, as fractures are caused by a greater external force than are lacerations. Slip down caused 43.9% of the lacerations and 33.7% of the fractures, the most common etiology for both injuries. Most of the laceration patients (20.7%) were under 10 years old, and most of the fracture patients (22.2%) were in their twenties. The lacerations among those under 10 years old were often light injuries caused by parents or by the patients' own carelessness.
In a previous study by Kim et al.10 exploring ER visits for soft tissue injuries, patients under 10 years of age visited the ER most frequently for such procedures, comprising 41.8% of patients seen; patients in their 20s comprised 11.6% of the population, and patients in their 30s, 11.1%. As for the causes of the injuries, 47.7% were from fall down, 19.1% were slip down, 9.4% were fist-related traumas, and 9.2% were traffic accidents. Likewise, Jang et al.8 reported that most of the patients (56.6%) were under 10 years of age; 14.5% were between 10 and 20 years old, and 12.9% were in their 20s. As for the causes of the lacerations, most of the patients (48.8%) were slip down, and 25.5% were fist trauma. In this study, the age distribution of the etiology of injury and the highest frequency of injuries were among those under 10 year old was consistent with other studies; those over 40 years old had a higher injury rate than in other studies. This higher injury rate among those over 40 was attributed to the high frequency of slip down and collisions, as well environmental issues brought on by the large entertainment district near the hospital. Carelessness after drinking in the nearby entertainment district was believed to have resulted in more frequent injuries.
In this study, 47% of the lacerations were solely intraoral lacerations, and 44% were solely extra-oral lacerations; only 9% were complex (intra-oral and extra-oral) lacerations. In the study by Kim et al.10, 66.7% of the cases were intra-oral lacerations, 10.8% were extra-oral lacerations, and 19.4%, complex lacerations. From 1992 to 1996, a study that examined individuals who visited the ER of same hospital revealed that 42% of visits were for intra-oral lacerations with soft tissue damage, 17.8% for extra-oral lacerations, and 34.1% for complex lacerations. These figures show a higher frequency of intra-oral lacerations than in the current study6. This discrepancy is thought to originate from differences in emergency department care systems and cooperation among other departments for maxillofacial trauma areas.
In the aforementioned study, the extra-oral lacerations occurred mostly in the upper third of the oral and maxillofacial area and were affected by the protrusion of the forehead and the eyebrows1112. Researchers found 221,190 lacerations on the forehead and eyebrows, and these lacerations showed a pattern similar to that in previous studies. They also found a high frequency of injuries (260 cases) in the chin area, which is in the lower third of oral and maxillofacial area. These differences came from possibility of common location damages in the chin area in relation to mandible fracture and tooth trauma so it is thought that the lower third of laceration area works is entrusted to the Department of Oral and Maxillofacial Surgery. The lip area had the greatest number (721 cases) of lacerations. This figure is considered very high, much higher than the 260 laceration cases in the chin area, where extra-oral lacerations occur most frequently. Because the lip area is a protruding structure and is near hard structures (i.e., teeth), it carries a high risk of injury and is the most easily perceived area of intra-oral lacerations at the time of the initial diagnosis in the ER.
Understanding the causes, severity, and distribution of oral and maxillofacial trauma is known to be of great help in generating effective precautionary measures and treatments13. Most previous ER-related research focused on facial bone fracture patients or general patients who visited the ER. In particular, research on soft tissue damage was very briefly mentioned or excluded from studies. This study focused exclusively on oral and maxillofacial lacerations, which occur most frequently with soft tissue damage and could cause permanent complications. It examined oral and maxillofacial lacerations in the context of diverse relevant factors. In this study, patients who were treated only in the Department of Oral and Maxillofacial Surgery were included, a potential limitation. If a study focused on oral and maxillofacial laceration progress, including collaboration with other departments, it would be more comprehensive. In this study, because the medical chart information was not entered by a facial trauma specialist, some information, such as the size and depth of the laceration, was not included. This implies the need for specialized facial trauma charting in future studies. Most lacerations patients were not hospitalized and did not receive regular follow up after stitches were removed. Thus, we were unable to include the frequency of postoperative complications, such as infection and scar formation. Therefore, it will be necessary to collect long-term data on oral and maxillofacial laceration patients. A future study on lacerations should be performed to validate the results of this study, which would be of great help in the evaluation and treatment of oral and maxillofacial laceration patients seen in the ER.
Go to : 
This study included 1,742 patients with oral and maxillofacial lacerations who visited the ER of Pusan National University Hospital over three years, from January 2011 to December 2013. A total of 2,094 laceration locations were examined. The overall male to female ratio was 2.50:1; 1,244 of the 1,742 patients were male and 498 were female. Most of the patients were under 10 years old, and most of the patients' visits were on weekends. Most of the lacerations were caused by slip down, followed by collisions and traffic accidents, in that order; a majority of the lacerations were either exclusively intra-oral or exclusively extra-oral lacerations rather than complex lacerations. Among intra-oral lacerations, the lip area was the most vulnerable site; among extra-oral lacerations, the chin area was more commonly injured. Most of the lacerations occurred without facial bone fracture and tooth damage. Laceration may differ in large part as compared with the fracture. Therefore, it is necessary to continue collecting data from oral and maxillofacial laceration patients over time to establish optimal diagnosis and treatment strategies for oral and maxillofacial laceration patients who visit the ER.
Go to : 
References
1. Huelke DF, Compton CP. Facial injuries in automobile crashes. J Oral Maxillofac Surg. 1983; 41:241–244. PMID: 6572693.

2. Hausamen JE. The scientific development of maxillofacial surgery in the 20th century and an outlook into the future. J Craniomaxillofac Surg. 2001; 29:2–21. PMID: 11467489.

3. Ong TK, Dudley M. Craniofacial trauma presenting at an adult accident and emergency department with an emphasis on soft tissue injuries. Injury. 1999; 30:357–363. PMID: 10505131.

4. Singer AJ, Thode HC Jr, Hollander JE. National trends in ED lacerations between 1992 and 2002. Am J Emerg Med. 2006; 24:183–188. PMID: 16490648.

5. Hollander JE, Singer AJ, Valentine S, Henry MC. Wound registry: development and validation. Ann Emerg Med. 1995; 25:675–685. PMID: 7741347.

6. Kim JR, Chung IK, Yang DK, Park BW. A clinical study on the emergency patients of oral and maxillofacial surgery during recent 5 years. J Korean Assoc Maxillofac Plast Reconstr Surg. 2001; 23:155–162.
7. Cho KS, Kim KY, Lee SH, Park HJ, So KS, Cho YK, et al. A clinical study on oral & maxillofacial patients visiting Chonnam Univ-hospitial emergency room. J Korean Assoc Maxillofac Plast Reconstr Surg. 1997; 19:435–446.
8. Jang CS, Lee CY, Kim JW, Yim JH, Kim JY, Kim YH, et al. A clinical study on the dental emergency patients visiting an University Hospital emergency room. J Korean Assoc Oral Maxillofac Surg. 2011; 37:439–447.

9. Kim HG, Son YH, Chung IK. Facial bone fracture patients visiting Pusan National University Hospital in Busan and Yangsan: trends and risks. Maxillofac Plast Reconstr Surg. 2014; 36:140–145.

10. Kim SH, Kim DY, Baek JS, Jung TY, Park SJ. Characteristics of dental emergency patients at Busan Paik Hospital. J Korean Assoc Maxillofac Plast Reconstr Surg. 2012; 34:58–64.
11. Hill CM, Burford K, Martin A, Thomas DW. A one-year review of maxillofacial sports injuries treated at an accident and emergency department. Br J Oral Maxillofac Surg. 1998; 36:44–47. PMID: 9578256.

12. Worrall SF. Mechanisms, pattern and treatment costs of maxillofacial injuries. Injury. 1991; 22:25–28. PMID: 2030025.

13. Hogg NJ, Stewart TC, Armstrong JE, Girotti MJ. Epidemiology of maxillofacial injuries at trauma hospitals in Ontario, Canada, between 1992 and 1997. J Trauma. 2000; 49:425–432. PMID: 11003318.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download