Abstract
Intraoral lipomas are a rare clinical entity, comprising only 0.1% to 5% of all benign tumors in the intraoral cavity. A 56-year-old woman suffering from diabetes presented with this relatively rare intraoral lipoma and was treated by surgical excision under general anesthesia. Because the mass was located adjacent to the mental foramen, a precise dissection was necessary to ensure minimal nerve damage. No abnormalities or recurrence was noted at 1-year follow-up and the patient did not complain of numbness. We studied the occurrence of oral lipoma in this diabetic patient and reviewed the relationship between oral lipoma and diabetes in the literature.
Go to : 
Lipomas are benign tumors comprising mature adipocytes and they can occur anywhere that adipocytes are present. They account for 15% to 20% of all benign tumors and 4% to 5% of benign tumors in the head and neck region12. Intraoral lipomas are rare and comprise only 0.1% to 5% of all benign tumors in the intraoral cavity3. Although lipomas can occur anywhere in the intraoral cavity, the major salivary glands (especially the parotid gland) are most frequently affected, followed by the buccal mucosa, lip, tongue, palate, floor of the mouth, and gingiva4. Small lipomas in the intraoral cavity may be asymptomatic, but large tumors may cause discomfort, difficulty chewing, dysphagia, and dyspnea. Typically, there is no pain or tenderness. Lipomas generally have well-defined margins, so surgical excision is recommended5. If they occur in the parotid gland, however, conservative treatment is preferred to preserve the facial nerve6. The rate of recurrence is 1% to 2%7. Herein, we review the literature and report a case of intraoral lipoma on the mandibular vestibule treated by surgical excision. We also study the relationship between oral lipoma and diabetes.
Go to : 
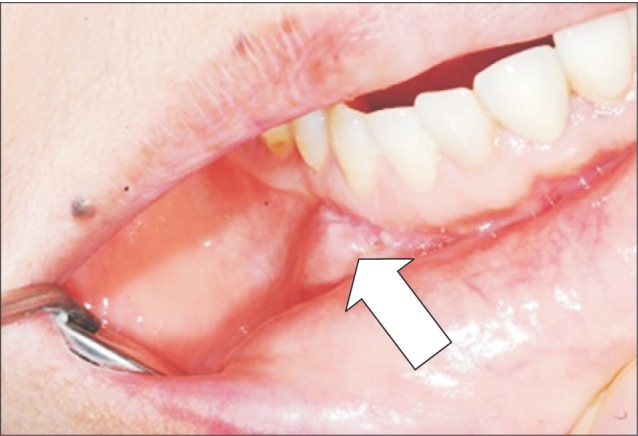
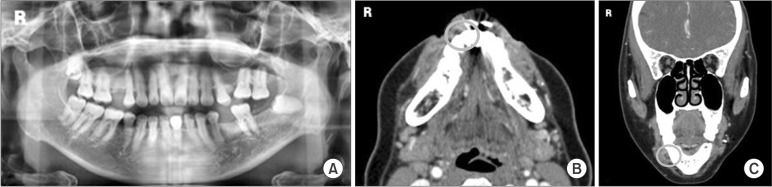
A 56-year-old woman visited the Department of Oral and Maxillofacial Surgery at Hallym University Kangdong Sacred Heart Hospital because of gingival swelling that started one month prior. The swelling had worsened over the previous two weeks and she had discomfort while eating. Upon intraoral examination, we observed swelling at the right first premolar mandibular vestibule and palpated a relatively solid mass, measuring approximately 2.0×1.5 cm and covered with normal gingival tissue. The patient did not complain of any pain when the mass was palpated. Aspiration analysis showed negative findings. We did not observe any masses at other sites in the intraoral cavity and cervical lymph nodes were not swollen. Fig. 1 shows an intraoral photograph of the mass and normal surrounding tissues. Specific findings related to the gingival swelling were not observed in the panoramic radiograph.(Fig. 2. A) The patient was treated for diabetes in our endocrinology department and otherwise had no predisposing medical or familial history.
In consultation with the endocrinology specialist, surgical excision and general anesthesia was planned. Because the mass was located adjacent to the mental foramen, a precise dissection was necessary to ensure minimal nerve damage.
Biochemical tests and urinalysis results were unremarkable except for values associated with diabetes (blood sugar test 96-254 mg/dL, HbA1c-National Glycohemoglobin Standardization Program [HbA1c-NGSP] 8.0%, HbA1c-International Federation of Clinical Chemistry [HbA1c-IFCC] 64 mmol/mol). Computed tomography of the neck revealed an ill-defined hypodense mass approximately 2 cm in diameter at the first right mandibular premolar.(Fig. 2. B, 2. C)
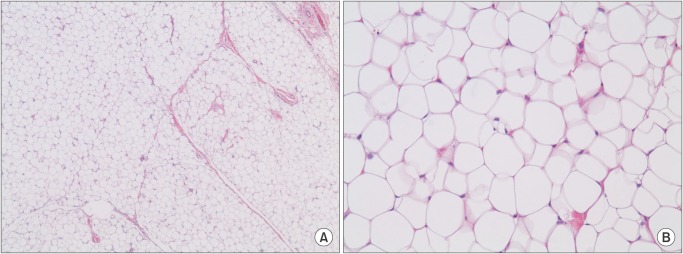
The mass was surgically excised under general anesthesia. The mass was encapsulated and well-defined within the surrounding tissue and measured approximately 1.1×1.0×0.6 cm.(Fig. 3, 4) Histopathologic examination revealed thin septa of connective tissue separating lobules of adipose tissue formed by mature, uniform adipose cells.(Fig. 5)
The patient was discharged the day following surgery. No abnormalities or recurrence was noted at 1-year follow-up and the patient did not complain of numbness.(Fig. 6)
This report was approved by the Ethics Committee at Hallym University Kangdong Sacred Heart Hospital (14-3-04). The patient agreed to be included in this research study.
Go to : 
Lipomas are the most common benign soft tissue tumors. Lipomas can occur in patients of all ages and are more common in females than males. Intraoral lipomas are rare, but are more likely to affect males over 40 years of age8.
From a clinical standpoint, intraoral lipomas are usually asymptomatic and grow slowly. The period from when patients notice the lipoma to when they seek medical care ranges from 1 month to 10 years, with a mean of 2 years89. The most affected areas are buccal mucosa, lip, tongue, palate, floor of the mouth, and gingiva. Lipomas mostly appear as round or oval shaped well-defined rigid masses. In some cases, the mass may be soft, depending on the amount of fibrous tissue.
It is usually easy to diagnose lipomas based on the macroscopic appearance except when they are located deeply. The histopathologic differential diagnosis includes fibroma, leiomyoma, pleomorphic adenoma in a minor salivary gland, papilloma, epidermoid cyst, and others10. On histopathologic examination, fibromas have a nodular mass of fibrous connective tissue covered by stratified squamous epithelium. Leiomyomas are well-circumscribed tumors that consist of interlacing bundles of spindle-shaped smooth muscle cells. The nuclei are elongated, pale staining, and blunt ended. Pleomorphic adenomas are typically well-circumscribed, encapsulated tumors. However, the capsule may be incomplete or show infiltration by tumor cells. This lack of complete encapsulation is more common for minor gland tumors, especially along the superficial aspect of palatal tumors beneath the epithelial surface. Papillomas are characterized by a proliferation of keratinized stratified squamous epithelium arrayed in finger-like projections with fibrovascular connective tissue cores. Epidermoid cysts have a cavity lined by stratified squamous epithelium resembling epidermis. A well-developed granular cell layer is seen, and the lumen is filled with degenerating orthokeratin11.
On histopathological analysis, fibro-connective tissue and blood vessels are observed between mature adipocyte in lipomas, and around that, a thin fiber tabernacle is encircled. There is a phospholipid vesicle in the center of the adipocyte, and cytoplasm and nuclei are observed at the border. An encircling fiber sac explains why they are well-defined in surrounding tissues.
Lipomas are known to arise from submucosa generally. Adipocytes within lipomas are multi-lobed and divided by fibro-connective tissue and blood vessels. About 80% are the general type, composed primarily of mature adipocytes; 20% are classified as fibro-lipomas and are composed of more fibrous tissues, and angiolipomas are composed of more angiotissues2912. Most lipomas occur singly, but they can be multiple1013 and then should be distinguished from liposis.
The recommended treatment for lipoma is surgical excision. Superficial lipomas are easily removed, but if they are positioned deeply, excision is difficult. After surgical excision, relapse and malignant alteration are rare9. In this case, to present there have been no specific changes after the excision.
Lipomas are associated with chronic stimulation, trauma, heredity, familial history, and have recently been correlated with diabetes. Das Gupta14 argued the hypertrophy theory that obesity and local growth of adipose tissue may both be responsible for the formation of a lipoma. The relationship between obesity and diabetes is well known.
In 1996, Suzuki et al.15 reported a case of mitochondrial diabetes caused by tRNA mutation. Over 12 years of follow-up, they observed two important clinical features: (1) lower limb paresthesia manifesting even with mild hyperglycemia and (2) lipoma (round, 10 mm diameter) manifesting at age 44 over the left breast. Low et al.16 hypothesized that lipid peroxidation under hyperglycemic conditions causes mitochondrial DNA mutations. Berkovic et al.17 described cases of four patients: two with multiple symmetric lipomatoses and two with lipoma and multisystem disorders; all patients had mitochondrial dysfunction. Holme et al.18 suggested that mitochondrial DNA mutations may be either a direct or an indirect cause of perturbation of the maturation process of adipocytes. In view of this, diabetes patients are exposed to DNA mutations and a high frequency of lipoma occurrence in diabetes patients can be assumed. So when a diabetic patient complains of an asymptomatic gingival swelling in the intraoral area, lipoma should be prominent in the differential diagnosis. We also recommend biopsy to confirm the diagnosis of lipoma.
Go to : 
References
1. Fregnani ER, Pires FR, Falzoni R, Lopes MA, Vargas PA. Lipomas of the oral cavity: clinical findings, histological classification and proliferative activity of 46 cases. Int J Oral Maxillofac Surg. 2003; 32:49–53. PMID: 12653233.

2. Guillou L, Dehon A, Charlin B, Madarnas P. Pleomorphic lipoma of the tongue: case report and literature review. J Otolaryngol. 1986; 15:313–316. PMID: 3773049.
3. de Visscher JG. Lipomas and fibrolipomas of the oral cavity. J Maxillofac Surg. 1982; 10:177–181. PMID: 6957523.

4. Pass B, Guttenberg S, Childers EL, Emery RW. Soft tissue lipoma with the radiographic appearance of a neoplasm within the mandibular canal. Dentomaxillofac Radiol. 2006; 35:299–302. PMID: 16798930.

5. Han CH, Kook MS, Park HJ, Oh HK, Ryu SY, Cho JH. Infiltrating lipoma of the cervical and parotid area: report of a case. J Korean Assoc Oral Maxillofac Surg. 2006; 32:598–602.
6. Debnath SC, Saikia A. Lipoma of the parotid gland extending from the superficial to the deep lobe: a rarity. Br J Oral Maxillofac Surg. 2010; 48:203–204. PMID: 19910088.

7. Malave DA, Ziccardi VB, Greco R, Patterson GT. Lipoma of the parotid gland: report of a case. J Oral Maxillofac Surg. 1994; 52:408–411. PMID: 8133376.

8. Hatziotis JC. Lipoma of the oral cavity. Oral Surg Oral Med Oral Pathol. 1971; 31:511–524. PMID: 4926907.

9. Horton JE. Lipomas of the tongue: report of a fibrolipoma. Oral Surg Oral Med Oral Pathol. 1968; 25:914–918. PMID: 5239745.
10. Greer RO, Richardson JF. The nature of lipomas and their significance in the oral cavity: a review and report of cases. Oral Surg Oral Med Oral Pathol. 1973; 36:551–557. PMID: 4580925.
11. Neville BW. Clinical review of oral and maxillofacial surgery. 3rd ed. St. Louis: Saunders Elsevier;2008.
12. Kacker A, Taskin M. Atypical intramuscular lipoma of the tongue. J Laryngol Otol. 1996; 110:189–191. PMID: 8729513.

13. Pisanty S. Bilateral lipomas of the tongue. Oral Surg Oral Med Oral Pathol. 1976; 42:451–453. PMID: 1067545.

14. Das Gupta TK. Tumors and tumor-like conditions of the adipose tissue. Curr Probl Surg. 1970; 7:3–60.

15. Suzuki Y, Tsukuda K, Atsumi Y, Goto Y, Hosokawa K, Asahina T, et al. Clinical picture of a case of diabetes with mitochondrial tRNA mutation at position 3271. Diabetes Care. 1996; 19:1304–1305. PMID: 8908402.

16. Low PA, Nickander KK, Tritschler HJ. The roles of oxidative stress and antioxidant treatment in experimental diabetic neuropathy. Diabetes. 1997; 46(Suppl 2):S38–S42. PMID: 9285497.

17. Berkovic SF, Andermann F, Shoubridge EA, Carpenter S, Robitaille Y, Andermann E, et al. Mitochondrial dysfunction in multiple symmetrical lipomatosis. Ann Neurol. 1991; 29:566–569. PMID: 1650162.

18. Holme E, Larsson NG, Oldfors A, Tulinius M, Sahlin P, Stenman G. Multiple symmetric lipomas with high levels of mtDNA with the tRNA(Lys) A-->G(8344) mutation as the only manifestation of disease in a carrier of myoclonus epilepsy and ragged-red fibers (MERRF) syndrome. Am J Hum Genet. 1993; 52:551–556. PMID: 8447321.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download