Abstract
Keratocystic odontogenic tumor (KCOT) is a common benign tumor of osseous lesions in dental and maxillofacial practice. We describe three cases of large KCOT located in the posterior part of the mandible extending to the angle and ramus region, which were enucleated via sagittal split osteotomy (SSO) of the mandible. There are cases in which a conventional enucleation procedure does not ensure complete excision of the entire lesion without damage to vital structures like the inferior alveolar nerve. In such cases, a SSO approach could be a better choice than conventional methods. The purpose of this article is to describe our experience using unilateral mandibular SSO for removal of a KCOT from the mandible.
Keratocystic odontogenic tumor (KCOT) is the most common benign tumor of the maxillofacial area. This tumor accounts for 3% to 21.5% of odontogenic tumors1. KCOTs were renamed in 2005 by the World Health Organization; they were originally referred to as odontogenic keratocysts2. KCOT is defined as "a benign uni- or multicystic, intraosseous tumor of odontogenic origin, with a characteristic lining of parakeratinized stratified squamous epithelium and the potential for aggressive, infiltrative behavior." Multiple KCOTs are usually associated with nevoid basal cell carcinoma (NBCC) or Gorlin-Goltz syndrome. Histopathological studies show that NBCCs are associated with KCOT3.
Various treatments have been suggested for KCOTs, but the gold standard treatment is still under debate. Treatments for this tumor range from enucleation to resection with or without cauterization4. Large cystic lesions in the retromolar region with extension into the ascending ramus make surgical approached challenging. When the cystic lesion is small, enucleation through an intraoral approach is acceptable; however, problems arise with large lesions, as the removal of large amounts of bone increases the potential for mandibular fracture and damage to the inferior alveolar nerve. Moreover, enucleation by an extraoral approach may leave an unsightly scar and lead to facial nerve injury. To avoid these complications, the use of a unilateral sagittal split osteotomy (SSO) technique has been introduced5.
The purpose of this article is to describe our unilateral SSO procedure for removal of large KCOT of the mandible. This report protocol was reviewed and approved by the Pusan National University Dental Hospital's Institutional Review Board (IRB No. PNUDH-2014-044).
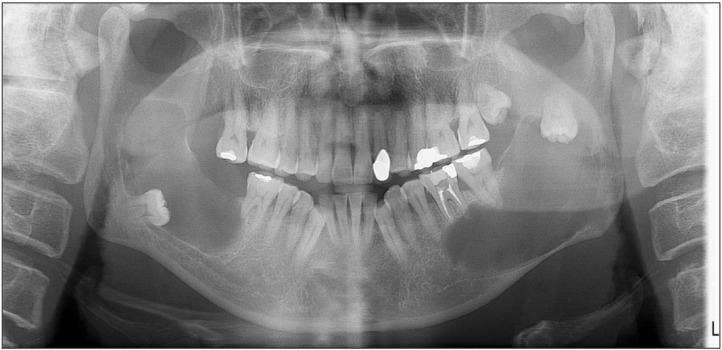
A 52-year-old man was referred to the Department of Oral and Maxillofacial Surgery at Pusan National University Dental Hospital due to the onset of symptoms involving a #37 tooth fracture. The patient has no specific medical history. Upon clinical examination, there was no swelling, hypoesthesia or pain. The large radiolucent unicystic lesions were observed bilaterally (right 3.5×6.5 cm, left 7.5×4.0 cm) including the mandibular body, ramus, and coronoid process of the mandible shown via panoramic radiography.(Fig. 1) The lesions involved the third molar teeth; the right molar was displaced downward and the left molar was displaced upward. In addition to tooth displacement, both sides of inferior alveolar nerve were deviated inferiorly by the lesions. Conebeam computed tomography (CBCT) showed expansion of the buccal bone and cortical thinning.
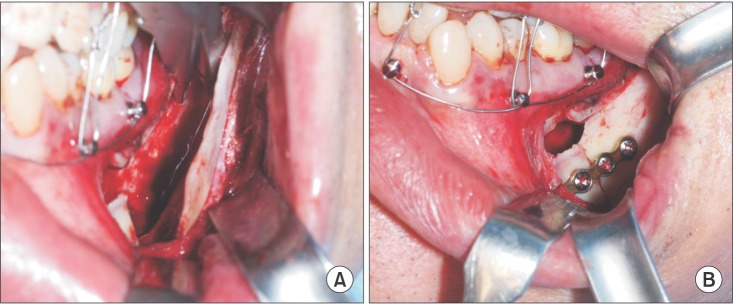
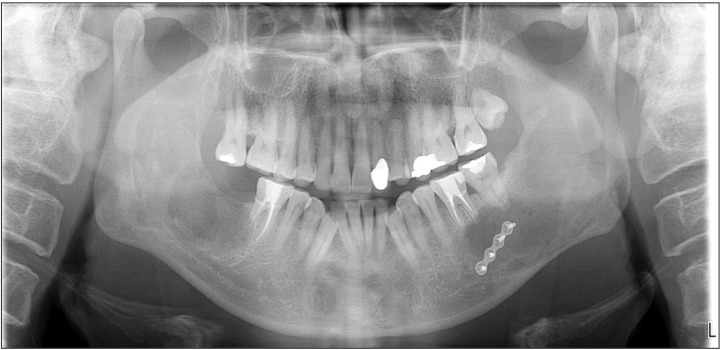
The cystic lesion was removed using SSO under general anesthesia. No unexpected intraoperative events, such as massive bleeding, nerve damage, or condyle fracture, occurred. The right side of the lesion was removed using the conventional enucleation method because the thickness of the buccal cortical bone was not conducive to placing a miniplate. The lesion on the left was removed as anticipated in the preoperative plan, via unilateral SSO. The cystic lining and the third molar were removed completely and the inferior alveolar nerve was preserved.(Fig. 2, 3) Immobilization of both sides of the segment was achieved through a miniplate and intermaxillary fixation (IMF) with a skeletal anchorage miniscrew for two weeks. Histological examination revealed the KCOT diagnosis. Minor postoperative complications, such as temporary hypoesthesia were observed. These symptoms disappeared within six months after surgery, and the clinical and radiographic prognosis were good.(Fig. 4)
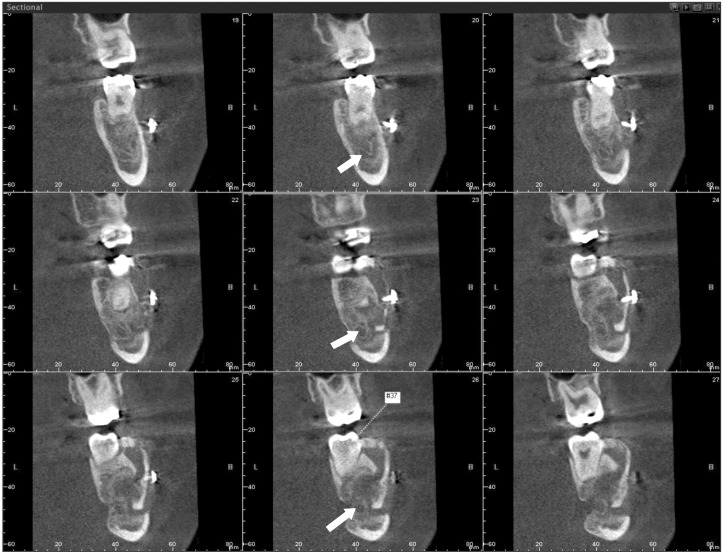
A 21-year-old man visited the clinic complaining of dull pain upon chewing and mouth opening. Radiographic examination revealed a 4×10-cm unicystic lesion on the left side of the mandible ranging from the molar region of the body to the ramus.(Fig. 5) The third molar was embedded in the lesion, which was located just adjacent to the apex of the second molar.
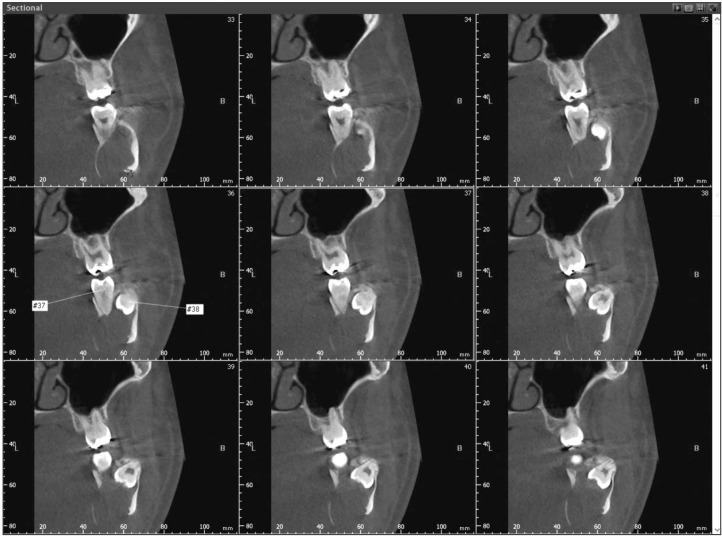
The lesion was enucleated using SSO under general anesthesia. The entire cystic lining and the third molar were removed and the inferior alveolar nerve was preserved. The apex of the second molar adjacent to the lesion was preserved. The stabilization of each segment was accomplished through a 4-hole miniplate and IMF with skeletal anchorage for 2 weeks. After releasing the IMF, an elastic guide was applied one month after surgery. Histological findings revealed KCOT. Postoperatively, there were no severe complications and radiographic evidence confirmed a good prognosis without recurrence.(Fig. 6) The healing process was shown on CBCT.(Fig. 7, 8)
A 19-year-old girl was referred from a local dental clinic for evaluation of a large cystic lesion on panoramic radiography. There were no clinical symptoms or relevant medical history, although the size of cystic lesion identified in CT was large (3.5×7.0 cm).(Fig. 9) The lesion was multilocular with cortical thinning at the right side of the mandible and the third molar was embedded in the lesion.
SSO was used to enucleate the large lesion under general anesthesia. Fixation and postoperative care were performed as described in case 2. Five months after surgery, the radiopacity of the lesion had increased in panoramic radiography. (Fig. 10) Any complication had not been found for follow-up period.
KCOT is typically treated via enucleation with or without cauterization. Marsupialization is another surgical option, but, eventually, enucleation should be performed. However, whenever the size or location of the lesion is unfavorable, such as endangering the inferior alveolar nerve or an adjacent tooth, a different approach must be considered to avoid complications.
There are multiple alternative approaches to removal of large benign tumors or cystic lesions in the posterior part of the mandible6.
- An intraoral approach via removal of the buccal or lingual cortex
- Segmental osteotomy via an extraoral approach
- Unilateral SSO
Several surgeons proposed an intraoral approach and discussed its advantages for removal of large odontomas5. They noted that there are risks associated with a thick buccal cortex, including fracture of the mandible and injury of the inferior alveolar nerve. Segmental resection causes bone defects and reconstruction is essential. Rittersma and van Gool7 initially described the SSO technique for removal of large, multilocular KCOTs. A similar approach has been reported by Rittersma and van Gool7 for excision of a mandibular myxoma. There are several reports in the English language literature of SSO that describe the removal of benign odontogenic tumor or third molars of the posterior mandible89101112.
There are three advantages of using an SSO to approach a large lesion of the mandible. Firstly, it is easy to secure the surgical field. Secondly, more cortical bone can be preserved, therefore hastening bone healing. Thirdly, the possibility of inferior alveolar nerve injury is lower than that of conventional methods. Although patients may complain of discomfort related to 2-week IMF, enucleation of a large cyst via the SSO approach is a viable alternative.
The method used herein does not vary greatly from bilateral SSO, which is most frequently used in orthognathic surgery. First, an osteotomy using an eggbur is performed above the lingula level of mandible, which is followed by splitting osteotomy using a reciprocal saw between the buccal and lingual cortical bone. At the mesial end of the proximal segment, a location with sufficient cortical bone for miniplate fixation is identified. Lastly, an osteotome is used to split the inferior border of the mandible. After splitting the buccal cortical bone of the proximal segment from the lingual cortical bone of the distal segment, we can achieve good access to the lesion.
The benign odontogenic lesion described herein, which was large and unfavorably located, ranging from the ramus to the mandible angle, was an ideal case for treatment with the SSO approach.
References
1. Gambhir A, Rani G. Conservative management of keratocystic odontogenic tumour with enucleation, excision of the overlying mucosa and electrocauterization: a case report. West Indian Med J. 2014; 63:[Epub ahead of print]. DOI: 10.7727/wimj.2014.052.
2. Madras J, Lapointe H. Keratocystic odontogenic tumour: reclassification of the odontogenic keratocyst from cyst to tumour. J Can Dent Assoc. 2008; 74:165–165h. PMID: 18353202.
3. Kulkarni GH, Khaji SI, Metkari S, Kulkarni HS, Kulkarni R. Multiple keratocysts of the mandible in association with Gorlin-Goltz syndrome: a rare case report. Contemp Clin Dent. 2014; 5:419–421. PMID: 25191087.

4. de Molon RS, Verzola MH, Pires LC, Mascarenhas VI, da Silva RB, Cirelli JA, et al. Five years follow-up of a keratocyst odontogenic tumor treated by marsupialization and enucleation: a case report and literature review. Contemp Clin Dent. 2015; 6(Suppl 1):S106–S110. PMID: 25821360.

5. Singh V, Bhagol A, Sharma B, Narwal A, Arya S. Surgical access to large unilocular cystic lesion through a sagittal split ramus osteotomy. J Oral Maxillofac Surg Med Pathol. 2012; 24:195–197.

6. Mahmood L, Demian N, Weinstock YE, Weissferdt A. Mandibular nerve schwannoma resection using sagittal split ramus osteotomy. J Oral Maxillofac Surg. 2013; 71:1861–1872. PMID: 23891013.

7. Rittersma J, van Gool AV. Surgical access to multicystic lesions, by sagittal splitting of the lower jaw. J Maxillofac Surg. 1979; 7:246–250. PMID: 291684.

8. Casap N, Zeltser R, Abu-Tair J, Shteyer A. Removal of a large odontoma by sagittal split osteotomy. J Oral Maxillofac Surg. 2006; 64:1833–1836. PMID: 17113456.

9. Wong GB. Surgical management of a large, complex mandibular odontoma by unilateral sagittal split osteotomy. J Oral Maxillofac Surg. 1989; 47:179–184. PMID: 2913254.

10. Wyatt WM. Sagittal ramus split osteotomy: literature review and suggested modification of technique. Br J Oral Maxillofac Surg. 1997; 35:137–141. PMID: 9146874.

11. Waldron CA. Oral epithelial tumors. In : Thoma KH, Gorlin RJ, Goldman HM, editors. Thoma's oral pathology. 6th ed. St. Louis: Mosby Co;1970. p. 846–847.
12. Shear M. Primary intra-alveolar epidermoid carcinoma of the jaw. J Pathol. 1969; 97:645–651. PMID: 5354042.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download