Abstract
Introduction
Quality of life (QoL) studies provide information about the impact of disease, the treatment of symptoms, and outcomes following treatment. The present study aims to evaluate the postoperative QoL of patients treated for oral cancer in a Nigerian government tertiary hospital.
Materials and Methods
A prospective study on consenting patients with oral cancer was undertaken at Aminu Kano Teaching Hospital, Kano, Nigeria. The subjects completed the University of Washington QoL (UW-QoL) questionnaire one day prior to surgery and postoperatively after 7 days, 1 month, 3 months, and 6 months.
Results
Sixty-eight patients with oral cancer were recruited. Of these, 38 were males, and 30 were females (male : female, 1.3 : 1). Twenty-four patients (12 males and 12 females) underwent surgery and completed postoperative QoL assessment using the UW-QoL questionnaire. Preoperative QoL mean score was 2.21, while postoperative mean scores after 1 week, 1 month, 3 months, and 6 months were 3.67, 3.46, 2.82, and 2.61, respectively.
Quality of Life (QoL) revolves around four core domains: physical functioning, psychological functioning, social interaction and disease, and treatment-related symptoms1. The acceptability of surgical treatment to the patient as well as a return to preoperative physical, psychological, and social functioning are areas that still require study2. There are numerous QoL studies in the literature; however, a search of the literature revealed only a few postoperative QoL studies that investigated the acceptability of surgical treatment for patients in Nigeria3,4,5. To the authors' knowledge, there is no study investigating postoperative QoL of surgically treated oral cancer patients in Nigeria. Information gained from these studies is vital for improving treatment outcomes and bridging the gap between patients' expectations and surgical outcomes.
The aim of this study was to evaluate the postoperative QoL of patients treated for oral cancer in a government tertiary hospital in Northern Nigeria using the University of Washington QoL (UW-QoL) questionnaire version 4.(Supplement) This instrument is considered a suitable routine outcome measure in head and neck cancer treatment6. It is a popular Health Related QoL (HRQoL) questionnaire used worldwide 7,8,9,10.
The UW-QoL is a 15-item questionnaire with 12 items assessing issues related to oral function, orofacial appearance, and social interaction11. These items refer to problems or symptoms experienced during the previous week and are rated on a Likert scale. The questionnaire also has 3 general questions and an invitation for free text expression by the respondent on his/her QoL11.
This prospective study was conducted from January 2011 to December 2012 at Aminu Kano Teaching Hospital (Kano, Nigeria).
Approval for the study was obtained from the ethics committee of the hospital (AKTH/MAC/SUB/12/II/P.3/164). Consented patients with histologically confirmed oral cancer were recruited for the study. The UW-QoL Questionnaire6 was completed 1 day prior to surgery and postoperatively after 7 days, 1 month, 3 months, and 6 months. Patients who could not communicate in English had their forms completed by the researcher with the help of an interpreter.
Scoring of the first 12 items of the UW-QoL is scaled so that a score of 0 represents the worst subjective function, and a score of 100 represents no subjective deficit11. Each domain (pain, appearance, activity, etc.) is scored separately. Possible domain scores are 0, 25, 30, 50, 70, 75, and 100. These scores are assigned to each number according to a published guideline 11. Items in the questionnaire have 3, 4, or 5 responses. Questions with 3 responses are scored as 30, 70, or 100; those with 4 responses are scored as 25, 50, 75, or 100; and those with 5 responses are scored as 0, 25, 50, 75, or 100. For the 3 general questions, each response is assigned a score progressively from 1 to 6. To calculate the QoL for each item, the number of respondents that choose a particular response is multiplied by the score of that response. This calculation was performed for all responses and summed to yield the total score for that item. The QoL for that item is calculated by dividing the total score by the number of respondents.
Computer analysis was performed using the SPSS software version 14.0 (SPSS Inc., Chicago, IL, USA). Comparative statistics were calculated, and tests of significance were determined using the chi square test and other relevant statistical tools as appropriate. Significance was set at a P-value of <0.05.
A total of 68 patients diagnosed with oral cancer were recruited over the study period. Of these, 38 patients (55.9%) were males, and 30 patients (44.1%) were females, resulting in a male-to-female ratio of 1.3 : 1.(Table 1) There was no statistically significant gender difference (P=0.064). Subject ages ranged from 7 to 80 years with a mean±standard deviation of 43.10±19.86 years. The ages of the male patients ranged from 7 to 70 years with a mean of 40.15±20.04 years, while those of the female patients ranged from 12 to 80 years with a mean of 48.37±18.23 years. The difference in mean age of males and females was not statistically significant (P=0.052). The majority of patients were aged 51 to 60 years (22.1%), followed by those aged 31 to 40 years (19.1%), and then those aged >70 years (1.5%).
Twenty-four patients (35.3%) received surgical treatment alone, while 14 patients (20.6%) received radiotherapy alone. Eight patients were treated with surgery and adjuvant radiotherapy, while 12 patients (17.6%) were given chemotherapy. A total of 10 patients (14.7%) received no treatment because they could not afford treatment or declined treatment (3 cases, 4.4%), or were deemed inoperable (7 cases, 10.3%). Inoperable cases were referred for hospice care.
Twenty-four subjects (12 males and 12 females) underwent surgery alone for oral malignancy during the study period (male : female, 1 : 1), and these patients constituted the study group. The difference in gender was not statistically significant (χ2=2.333, degree of freedom=3, P=0.506). Subject age ranged from 12 to 70 years with a mean of 45.96±19.38 years. The majority of patients were aged 61 to 70 years (29.2%), followed by patients aged 31 to 40 and 51 to 60 years (20.8% each), then those patients aged 41 to 50 years (4.2%).
Histologic diagnosis and sex distribution of these subjects are presented in Table 2. The most frequently involved site was the maxilla (7 cases, 29.2%), followed by the lower lip and buccal mucosa (3 cases each, 12.5%). Other sites included the mandible, palate, and salivary glands (2 cases each, 8.3%), and the upper lip, gingiva, retromolar region, floor of mouth, and pharynx (1 case each, 4.2%). Patients identified 'appearance' (83.3%), 'recreation' (66.7%), and 'chewing' (58.3%) as the three most important factors determining their well-being following surgery for oral malignancy. The 'shoulder' and 'saliva' domains of the UW-QoL recorded the highest mean score of 100.0 with 100% of patients assigning the best possible score. The 'pain' domain had the lowest mean score of 30.21 with only 4.2% of patients submitting the best possible score.(Table 3)
Responses to the UW-QoL 'general health' item of the 24 patients who underwent surgery for oral malignancy (as measured by the patients' own perceptions) were found to markedly rise immediately following surgery (3.67) and then have a steady decline from 1 month (3.46) to 3 months (2.82) and then 6 months (2.61). This decline did not descend to the original baseline (2.21) measured prior to surgery.(Table 4)
A comparative assessment of patients' QoL postoperatively and one month before diagnosis showed that there was an increase in patients' perceptions of their health after surgery, which was sustained throughout the study period (baseline 2.33, 1 week 2.75, 1 month 2.88, 3 months 2.64, 6 months 3.11). The overall QoL of these patients improved from 2.42 preoperatively to 4.78 by 6 months postoperatively.(Table 4)
QoL assessment has long been recognized by many Nigerian 12,13,14,15,16 and international authors17,18 to be an integral part of oral cancer management. Even so, the use of HRQoL questionnaires is not universal. Kanatas and Rogers19 did a national study on the use of HRQoL among practicing consultants in the United Kingdom and found that only 29% of the consultants used HRQoL questionnaires. Their study also showed that UW-QoL was the most popular questionnaire used for HRQoL studies.
Kanatas and Rogers19 also found that questionnaires were mostly used before and after treatment (67%) and were administered by either nursing staff or consultants. The main reasons HRQoL questionnaires were not being used included lack of resources and lack of proven value. In a review of papers published on QoL in head and neck cancer from 2000 to 2005, Rogers et al.20 found that despite the many advantages of such questionnaires, there were still areas requiring further research.
Patients treated with surgery in this study were found to have increased QoL scores despite the fact that not all of these patients had received full reconstruction at the time of their evaluation. The mean score for 'appearance' following surgery was one of the lowest domain scores with a value of 46.88, but it was given the highest rating in domain importance. Considering that the overall QoL measured after surgical treatment, it can be theorized that improvement in appearance is an important aspect of surgical outcome for patients.
The shoulder domain recorded the highest possible score because none of our patients had either radical neck dissection or surgery at the shoulder for reconstruction. The saliva domain similarly recorded the same score because this domain is used to assess xerostomia following radiotherapy. All patients who completed this form received surgical treatment alone. 'Chewing' had the worst domain mean score rating. This is possibly due to the lack of bony reconstruction and prosthetic rehabilitation in most of the patients. Patients' overall assessments of their QoL were good despite this obvious drawback.
Rogers et al.20 assessed the domain importance ratings of the UW-QoL Questionnaire using 48 patients with previously untreated oropharyngeal cancer treated by primary surgery alone. The questionnaires were completed preoperatively and postoperatively after 6 months and 1 year. They found that at all time points, patients rated speech, chewing, and swallowing as more important than the other UW-QoL domains. This is comparable with our results, in which patients identified 'appearance,' 'recreation,' and 'chewing' as the most important outcomes of treatment. Bearing in mind the difficulties of comparing these studies, the observed differences may be a reflection of differences in the psychological makeup of the two study groups. The difficulties with swallowing seen in their study may be a reflection of oropharyngeal cancer surgery performed on those patients. Obviously, much more investigation is needed before establishing definite conclusions.
Cancer treatment in Nigeria is often limited by lack of infrastructural development, late patient presentation, and lack of finances. Absence of computerized tomographic scans, magnetic resonance imaging, and frozen sections for appropriate diagnosis and staging of oral cancer could misguide the surgeons and limit the scope of treatment. Atchison et al.21 investigated the relationships between the objective clinician assessment of the postoperative outcome of mandibular fracture treatment and the subjective assessment of patients and found that the two groups may have differing perceptions. Patients' assessments of outcomes are often superficial and limited to aspects of outcomes related to aesthetics and/or functional impairment. This study on mandibular fractures reveals that patient and clinician expectations may differ. This may also be seen in cancer surgery, as most uneducated patients are initially only concerned with eliminating the tumor burden.
Our study showed improved QoL following surgical treatment despite absence of functional rehabilitation. This was an unexpected finding and may be related to the fact that functional rehabilitation after cancer treatment is uncommon in our region. Many patients set their expectations mainly on surgically treatment and do not look beyond these initial benefits. Also, there could be the cancer 'fear factor' which would increase their acceptance of surgical excision alone if they consider themselves to be free of the tumor burden. Another consideration is the late presentation of our patients often with disfiguring, fungating masses with an offensive odor. Surgical excision at this stage rids the patients of these problems thereby improving their acceptance of the treatment.
QoL assessment tools provide much needed insight into patients' self-perceptions and impressions about the treatments they have received. Further understanding of patients' needs and perceptions will result in better patient management and eventually better QoL scores. Though the present study is a subjective assessment of patients after a 6-month postoperative review, it highlights the importance of QoL studies in patients treated for oral cancer. Future studies could aim to compare QoL among patients with different treatment modalities.
'Appearance,' 'recreation,' and 'chewing' were identified as the most important determinants of postoperative QoL in patients with oral cancer in our study. Also, improvement in postoperative QoL scores suggests that intervention is indicated for operable cases. QoL studies may be a guide for the caregiver to plan treatment based on a patient's expectations, thereby making management more holistic.
References
1. Marx RE, Stern D. Oral and maxillofacial pathology: a rationale for diagnosis and treatment. Chicago: Quintessence Publishing;2003. p. 283–293.
2. Tang XH, Knudsen B, Bemis D, Tickoo S, Gudas LJ. Oral cavity and esophageal carcinogenesis modeled in carcinogen-treated mice. Clin Cancer Res. 2004; 10:301–313. PMID: 14734483.

3. Hotary K, Allen E, Punturieri A, Yana I, Weiss SJ. Regulation of cell invasion and morphogenesis in a three-dimensional type I collagen matrix by membrane-type matrix metalloproteinases 1, 2, and 3. J Cell Biol. 2000; 149:1309–1323. PMID: 10851027.

4. Kaplan RN, Rafii S, Lyden D. Preparing the "soil": the premetastatic niche. Cancer Res. 2006; 66:11089–11093. PMID: 17145848.
5. Carnelio S, Rodrigues G. Oral cancer at a glance. Internet J Dent Sci [Internet]. 2003; 1(2):cited 2013 Mar 21. Available from: https://ispub.com/IJDS/1/2/5720.
6. SEER cancer statistics review, 1975-2005 [Internet]. Bethesda(MD): National Cancer Institute;cited 2009 Jan 26. Available from: http://seer.cancer.gov/archive/csr/1975_2005.
7. World Health Organization (WHO). International statistical classification of diseases and related health problems. 10th revision. Geneva: WHO;1992. p. 42–57.
8. Parkin DM, Pisani P, Ferlay J. Estimates of the worldwide incidence of eighteen major cancers in 1985. Int J Cancer. 1993; 54:594–606. PMID: 8514451.

9. The Oral Cancer Foundation [Internet]. Newport Beach (CA): The Oral Cancer Foundation;cited 2006 May 28. Available from: http://www.oralcancerfoundation.org.
10. Levi F, Lucchini F, La Vecchia C. Worldwide patterns of cancer mortality, 1985-89. Eur J Cancer Prev. 1994; 3:109–143. PMID: 7517250.

11. Rogers SN, Laher SH, Overend L, Lowe D. Importance-rating using the University of Washington quality of life questionnaire in patients treated by primary surgery for oral and oro-pharyngeal cancer. J Craniomaxillofac Surg. 2002; 30:125–132. PMID: 12069517.

12. Goldspiel BR, Green L, Calis KA. Human gene therapy. Clin Pharm. 1993; 12:488–505. PMID: 8354036.
13. Arotiba GT, Ladeinde AL, Oyeneyin JO, Nwawolo CC, Banjo AA, Ajayi OF. Malignant orofacial neoplasms in Lagos, Nigeria. East Afr Med J. 2006; 83:62–68. PMID: 16771101.

14. Ajayi OF, Adeyemo WL, Ladeinde AL, Ogunlewe MO, Effiom OA, Omitola OG, et al. Primary malignant neoplasms of orofacial origin: a retrospective review of 256 cases in a Nigerian tertiary hospital. Int J Oral Maxillofac Surg. 2007; 36:403–408. PMID: 17391919.

15. Adekeye EO, Asamoa E, Cohen B. Intraoral carcinoma in Nigeria: a review of 137 cases. Ann R Coll Surg Engl. 1985; 67:180–182. PMID: 4004050.
16. Ugboko V, Ajike S, Olasoji H, Pindiga H, Adebiyi E, Omoniyi-Esan G, et al. Primary orofacial squamous cell carcinoma: a multicenter Nigerian study. Internet J Dent Sci [Internet]. 2003; 1(2):cited 2013 May 5. Available from: https://ispub.com/IJDS/1/2/10778.
17. Arotiba JT, Obiechina AE, Fasola OA, Fawole OI, Ajagbe HA. Oral squamous cell carcinoma: a review of 246 Nigerian cases. Afr J Med Med Sci. 1999; 28:141–144. PMID: 11205818.
18. Lippman SM, Sudbø J, Hong WK. Oral cancer prevention and the evolution of molecular-targeted drug development. J Clin Oncol. 2005; 23:346–356. PMID: 15637397.

19. Kanatas AN, Rogers SN. A national survey of health-related quality of life questionnaires in head and neck oncology. Ann R Coll Surg Engl. 2004; 86:6–10. PMID: 15005937.

20. Rogers SN, Ahad SA, Murphy AP. A structured review and theme analysis of papers published on 'quality of life' in head and neck cancer: 2000-2005. Oral Oncol. 2007; 43:843–868. PMID: 17600755.

21. Atchison KA, Shetty V, Belin TR, Der-Martirosian C, Leathers R, Black E, et al. Using patient self-report data to evaluate orofacial surgical outcomes. Community Dent Oral Epidemiol. 2006; 34:93–102. PMID: 16515673.

Table 2
The histologic diagnosis and sex distribution of 24 subjects surgically treated for oral cancer
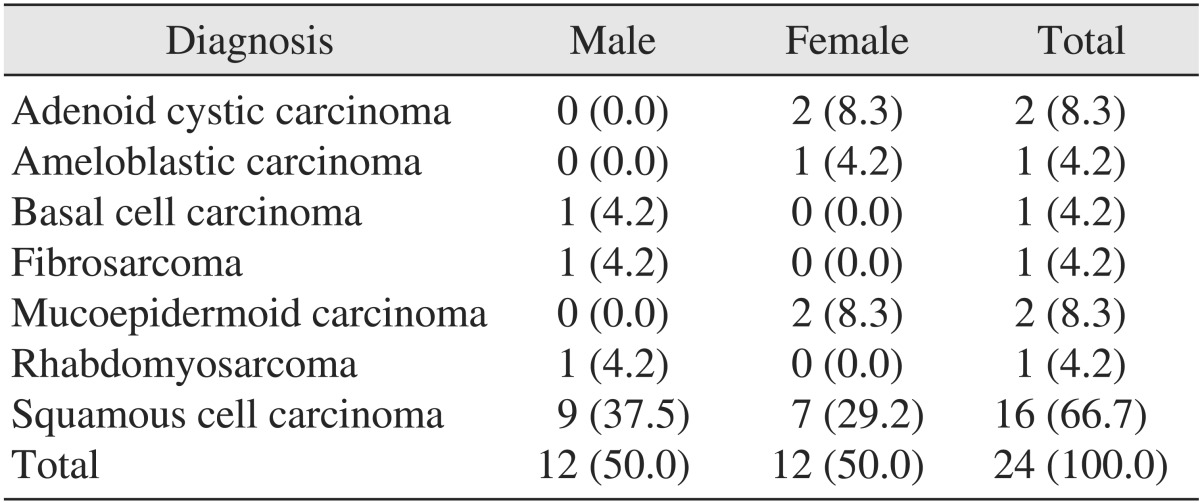
Table 3
University of Washington quality of life domain scores and importance rating of 24 subjects with oral malignancy at 6-month review
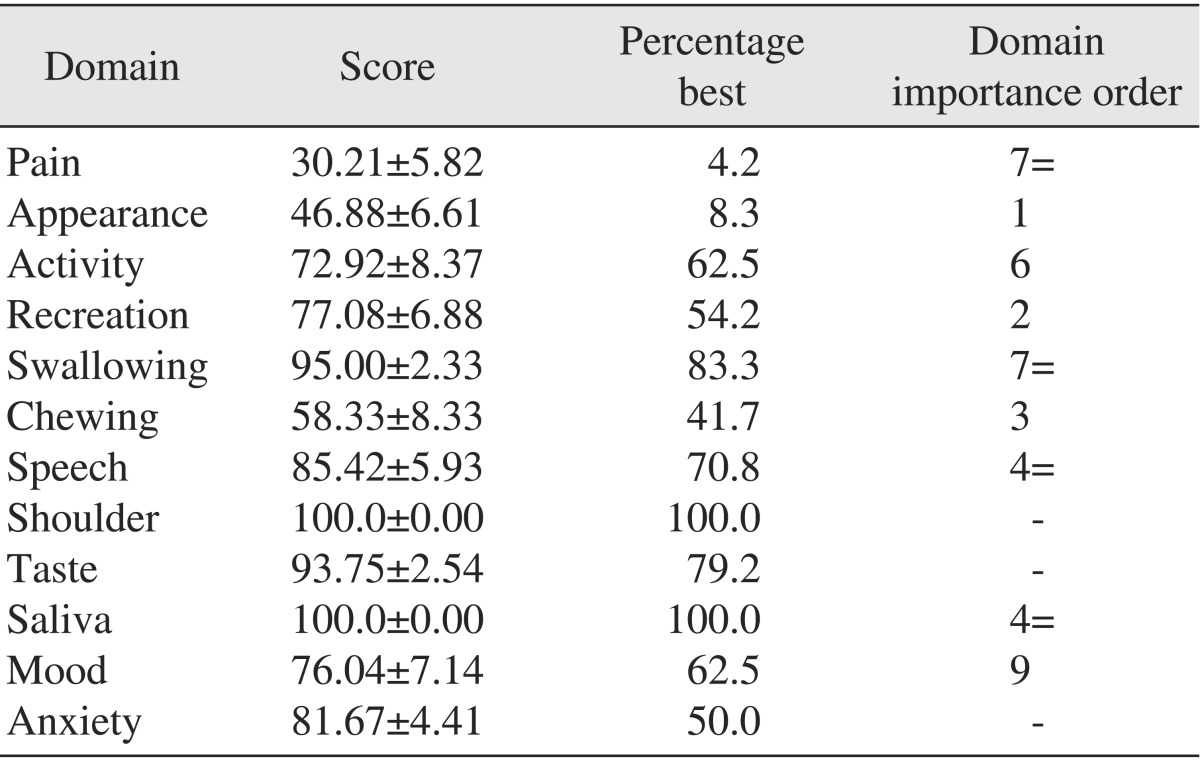
Table 4
Quality of life general health values of 24 oral malignancy patients taken before and after surgery
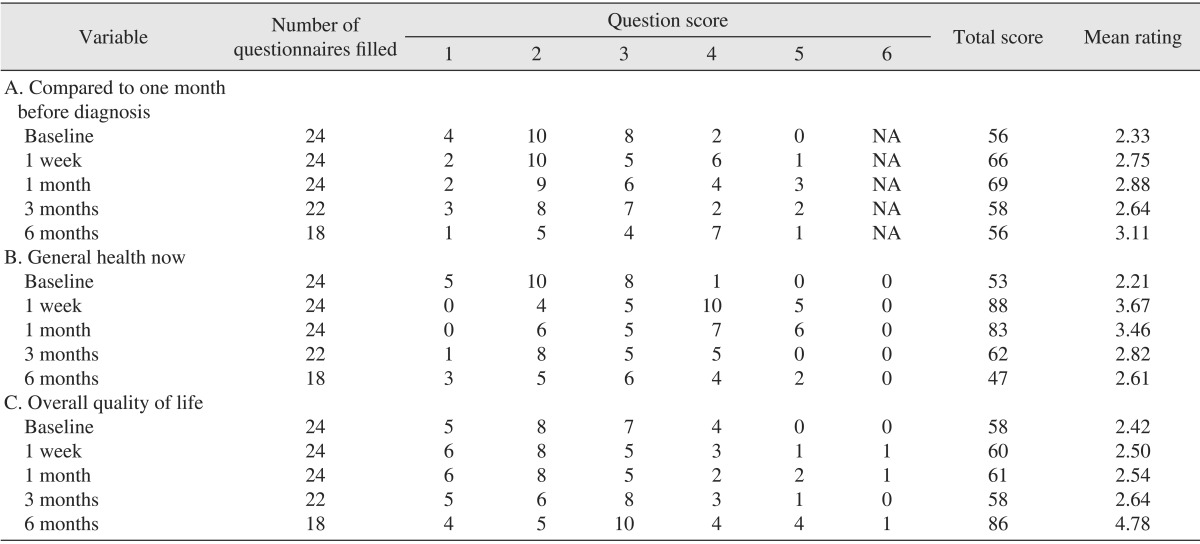
(NA: question not available)
Key to ratings: A, '1' very poor, '2' poor, '3' fair, '4' good, '5' very good, and '6' outstanding; B, '1' much worse, '2' somewhat worse, '3' about the same, '4' somewhat better, and '5' much better; C, '1' very poor, '2' poor, '3' fair, '4' good, '5' very good, and '6' outstanding.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download