This article has been
cited by other articles in ScienceCentral.
Abstract
In 1942 Stafne reported 35 asymptomatic, radiolucent cavities that were unilaterally located in the posterior region of the mandible between the mandibular angle and the third molar, and below the mandibular canal. The term Stafne bone cavity (SBC) is now used for such asymptomatic lingual bone depressions of the lower jaw. Since then there have been many reports of SBCs but very fews tudies have used cone-beam computed tomography (CBCT) for their diagnosis. The aim of this paper is to describe the clinical and radiological characteristics of two cases of SBCs and the importance of limited CBCT in confirming the diagnosis.
Go to :

Keywords: Stafne bone cavities, Cone-beam computed tomography, Panoramic radiography, Salivary glands
I. Introduction
Stafne
1 first described 35 asymptomatic radiolucent lesions located unilaterally in the posterior region of the mandible, between the mandibular angle and the third molar, inferior to the mandibular canal, and slightly above the mandibular base.
This entity has been given numerous names based on different theories of etiopathogenesis, including static bone cyst, lingual mandibular bone defect, Stafne bone cavity (SBC), idiopathic bone cavity, and lingual mandibular bone depression
2. However, the accepted theory is that they develop as a result of localized pressure atrophy of the lingual surface of the mandible from the adjacent salivary gland
3.
SBCs are most commonly observed in men in their fifth or sixth decade of life and have a prevalence between 0.10% and 0.48%
456. They may present as round or oval, and range in size from 1 to 3 cm in diameter
7.
SBC is more commonly seen in the posterior region of the mandible (posterior variant), but can also appear in the anterior region (anterior variant) and in the ascending ramus of the mandible (mandibular ramus variant)
8. It is generally unilateral, with some reports of bilateral occurrence
9101112. Double unilateral occurrence is rare, and bilocular occurrence is even rarer
9. There are many reports of SBC but the use of conebeam computed tomography (CBCT) for diagnosis is rare. The aim of this paper is to describe the clinical and radiological characteristics of 2 cases of Stafne bone cyst and the importance of limited CBCT in confirming the diagnosis.
Go to :

II. Cases Report
1. Case 1
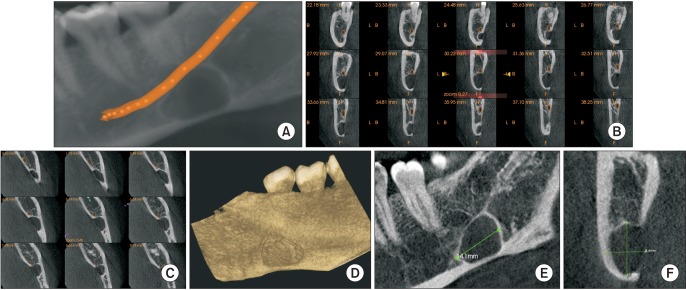
A 31-year-old asymptomatic male patient was referred to Secunderabad Dental Imaging Centre (Hyderabad, India) to undergo routine panoramic radiography. The panorama revealed a cystic lesion in the left posterior mandible just anterior to the mandibular angle and below the third molar and mandibular canal.(
Fig. 1) There was no significant medical or dental history. There was no tenderness on bidigital palpation at the site of the lesion. For further analysis, CBCT restricted to the area of lesion was performed. The results revealed a complete radiolucent lesion that was regular, oval in shape, and well corticated.(
Fig. 2. A-D) The lesion was located below the mandibular canal and measured 11.8×8.4×14.1 mm (height×breadth×length).(
Fig. 2. E, 2. F) The long axis of the lesion was placed horizontally on the left side. The cross-sections revealed a close relationship with the mandibular nerve without any pressure effect.(
Fig. 2. B) The patient was asymptomatic and there was no parasthesia or anaesthesia. The buccal wall was intact and there was no expansion (
Fig. 2. B); however, the lingual wall was involved. The inferior border was also intact with little pressure atrophy.
 | Fig. 1Panoramic view shows the lesion.
|
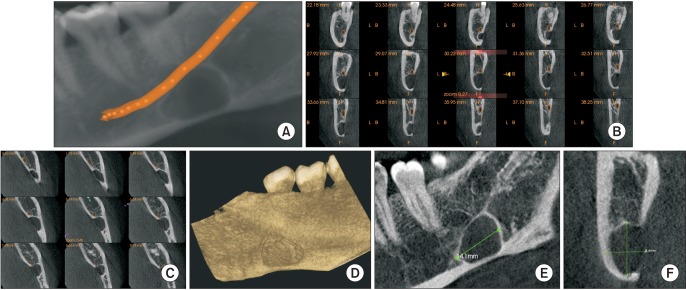 | Fig. 2Cone-beam computed tomography images. A. Panoramic view with mandibular nerve canal traced. B. Cross-section revealing the relationship of the lesion with the mandibular canal. C. Axial view revealing the relationship of the lesion with the mandibular canal. D. Three-dimensional reconstructed view from lingual aspect. E, F. Dimensions of the lesion.
|
A radiographic diagnosis of SBC was considered and the patient was advised to undergo regular follow-up examinations.
2. Case 2
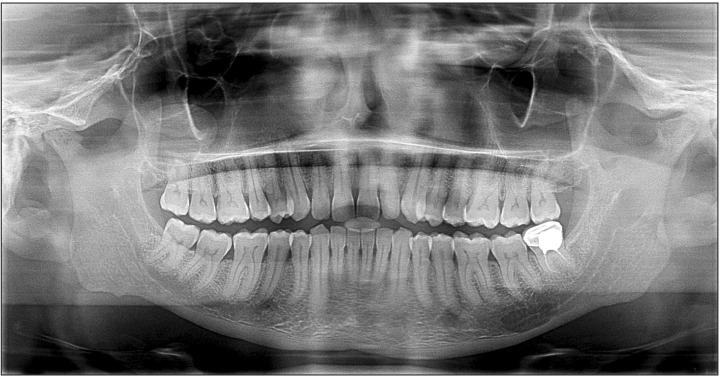
A 35-year-old male patient was similarly referred to Secunderabad Dental Imaging Centre (Hyderabad, India) to undergo routine panoramic radiography. The panorama revealed a cystic cavity on the left side below the second molar and mandibular canal, anterior to the angle of the mandible. (
Fig. 3) Medical and dental history was not contributory. There was no tenderness on bidigital palpation at the site of the lesion. For further analysis, CBCT restricted to the area of lesion was performed. The results revealed a complete radiolucent lesion that was regular, oval in shape, and well corticated.(
Fig. 4. A-D) The lesion was situated below the mandibular canal and measured 4.7×12.7×16.6 mm (height ×breadth×length).(
Fig. 4. E, 4. F) The long axis of the lesion was situated horizontally in the left side. Cross-sections revealed a mandibular canal within the lesion without any pressure effect.(
Fig. 4. B) The patient was asymptomatic and there was no parasthesia or anaesthesia. The buccal wall and the inferior border were intact and there was no expansion (
Fig. 4. B); however, the lingual wall was involved and the inferior border showed some pressure atrophy.
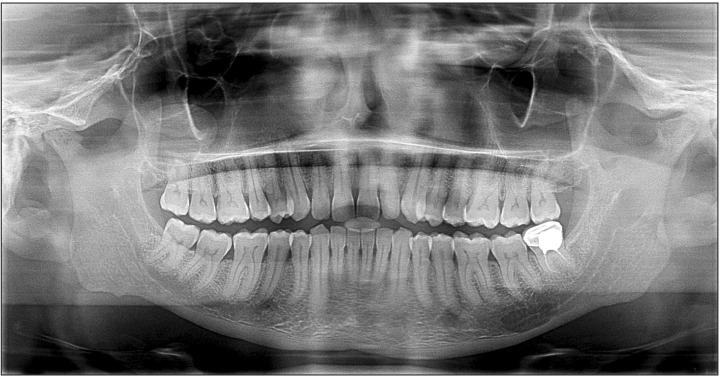 | Fig. 3Panoramic view shows the lesion.
|
 | Fig. 4Cone-beam computed tomography images. A. Panoramic view with mandibular nerve canal traced. B. Cross-sections revealing the relationship of the lesion with the mandibular canal. C. Axial view revealing the relationship of the lesion with the mandibular canal. D. Three-dimensional reconstructed view from lingual aspect. E, F. Dimensions of the lesion.
|
A radiographic diagnosis of SBC was considered and the patient was recommended for regular follow-up.
Go to :

III. Discussion
Since Stafne first described the SBC in 1942, many cases have been reported. The most widely accepted etiopathogenesis is that the lesions develop as a result of localized pressure atrophy of the lingual surface of the mandible from the adjacent salivary gland
17910.
There are anterior and posterior variants of SBC, although most cases are posterior variants located between the mandibular angle and first mandibular molar tooth below the inferior dental canal
124789101112131415161718. In both of our cases the lesions were situated in the posterior region below the mandibular canal, anterior to the angle of the mandible, and on the left side.
According to their relationship to the buccal cortical wall, SBCs can be divided into three types: in type I, the cavity does not reach the buccal cortex; in type II, it reaches the buccal cortex without expanding it; and in type III, the buccal osseous cortex is expanded
19. Both of the cases described here belonged to type II.
SBCs are incidental findings because patients are asymptomatic
4. Radiographically, they present as a cystic cavity with a well-defined sclerotic border, situated in the posterior region of the mandible, below the inferior dental canal
1718. Similar findings were obtained in our cases.
The reported predilection of SBC in men is aged between 50 and 70 years
271113. Both of our patients were male, but they were relatively young at 37 and 35 years old, respectively. Both were asymptomatic.
SBCs are an anatomical rather than a pathological condition and do not require any surgical treatment. Patients are usually only followed up radiographically, although surgical exploration or biopsy should be performed in atypical cases or other suspected lesions. As there were no signs of inflammatory or tumoral changes in our patients no surgical intervention was performed and the patients were recommended for regular follow-up.
CBCT is a major innovation in the field of dentistry and has gained popularity because of its low radiation, limited area exposure, high resolution, and ease of availability compared to medical CT
20.
CBCT facilitates both diagnosis and follow-up, especially through the reconstructed images that show radiographic features in fine detail. In both of our cases CBCT was very helpful in analyzing the cases and establishing a negative relationship with dentition and the mandibular canal. Another important aspect of our paper is the use of limited area exposure with CBCT, which is an added advantage of this technique.
SBCs are incidental findings, especially on panorama, and are considered anatomical rather than pathological. They do not have any alarming effects on the surrounding structure and do not require surgical attention, but only regular radiographic follow-up. However, they should be analyzed using three-dimensional imaging to rule out other similar appearing lesions. As demonstrated in our cases, the use of CBCT is highlighted because of the low radiation dose, limited area exposure, and the fine detail of imaging, which is beneficial for the diagnosis of SBC.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download