This article has been
cited by other articles in ScienceCentral.
Abstract
Odontogenic carcinosarcoma is an extremely rare malignant odontogenic tumor with only a few reported cases. It is characterized by a true mixed tumor showing malignant cytology of both epithelial and mesenchymal components. It has been assumed to arise from pre-existing lesions such as ameloblastoma, ameloblastic fibroma, and ameloblastic fibrosarcoma. To date, the reported cases have exhibited considerably aggressive clinical behavior. The case of an odontogenic carcinosarcoma in the mandible of a 61-year-old male is described herein. The tumor destroyed the cortex of the mandible and invaded the adjacent tissues. Treatment was performed by surgical resection and reconstruction. The purposes of this article are to introduce odontogenic carcinosarcoma through this case study, to distinguish it from related diseases and to discuss features of the tumor in the existing literature.
Go to :

Keywords: Carcinosarcoma, Mixed tumor, Ameloblastoma, Fibrosarcoma, Odontogenic tumor
I. Introduction
Odontogenic carcinosarcoma is an extremely rare malignant tumor that is a mixture of odontogenic carcinoma and sarcoma, such that both epithelial and mesenchymal components show malignant activity
12345. Odontogenic neoplastic potential correlates with odontogenesis. Odontogenesis depends on the close interaction of epithelial and mesenchymal tissues
46. Either purely epithelial or mesenchymal or a mixture of both tissues may form neoplastic lesions. Clinically, the tumor presents with aggressive, recurrent and metastasizing features
12345. Treatment is primarily surgical resection, though an adjuvant therapy may be necessary.
Odontogenic carcinosarcoma is related with some tumors such as ameloblastoma, ameloblastic fibroma, ameloblastic fibrosarcoma, and osteosarcoma. Etiologically, the aforementioned lesions may affect the pathogenesis of odontogenic carcinosarcoma by transformation, but this is unclear. Moreover, owing to the scarcity of reported cases, its clinical significance remains unexplored
13678.
Our case will be the sixth case of odontogenic carcinosarcoma in the literature. The aim of this report is to discuss the pathological and clinical features of odontogenic carcinosarcoma and increase our knowledge on this rare entity.
Go to :

II. Case Report
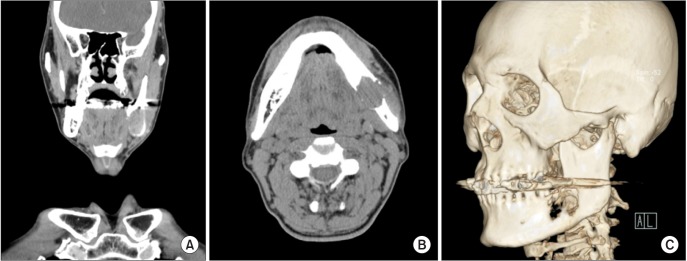
A 61-year-old male presented with discomfort, intermittent paresthesia and a slightly painful mass of the left mandible in July 2011. Physical examination revealed nonvital tooth number 37 was painful to percussion. There was no other abnormality. Imaging studies showed a large radiolucent lesion of the left mandible which had a round shape and clear margins. The mass included the root of the left 2nd molar extending to the anterior aspect of the ascending ramus.(
Fig. 1) In addition, it involved the left alveolar canal and destroyed the inner cortex of mandible.(
Fig. 2) Magnetic resonance imaging (MRI) identified invasion of the adjacent bone marrow, outer soft tissue (submandibular area), and masseter muscle with no significant lymphadenopathy.(
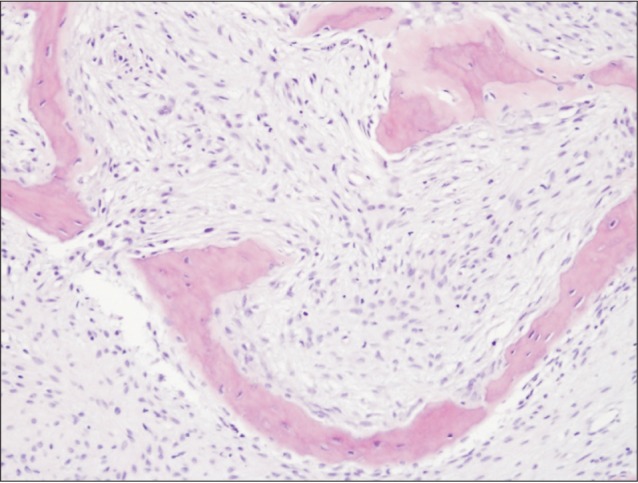
Fig. 3) An incisional biopsy was performed, and the diagnosis was osteosarcoma of the jaw. On bone scan, another active bone lesion was detected in the proximal one third of the right tibia. There was an intramedullary osteolytic lesion in the proximal diaphysis of the tibia with a thin sclerotic rim on MRI images of the right tibia. Subsequently, computed tomography (CT) guided biopsy revealed a linear core of tissue consisting of delicate trabeculae of woven bone in fibrous stroma and no epithelial element.(
Fig. 4) The diagnosis of the tibial lesion was fibrous dysplasia, and seemed to be irrelevant to oral cancer. Nevertheless, the possibility of distant metastasis could not be completely excluded by CT guided biopsy. Therefore, surgery and excisional biopsy for the tibial lesion was recommended, but the patient refused the procedure.
 | Fig. 1Panoramic view shows radiolucent lesion of the left mandible.
|
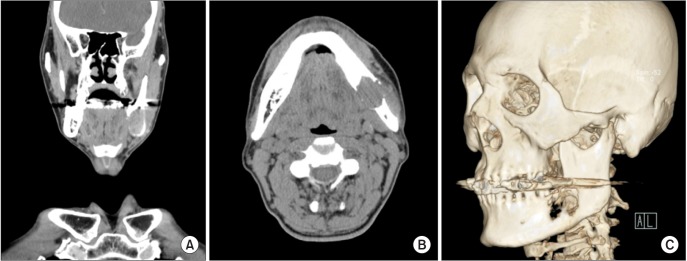 | Fig. 2Computed tomography shows an osteolytic mass with destruction of the inner cortex in the angle of the left mandible, involving the periapical area of the left 2nd molar tooth and left alveolar canal. A. Coronal view. B. Axial view. C. Three-dimensional image view.
|
 | Fig. 3Magnetic resonance imaging shows 2.2×2.8×4.1 cm sized osteolyitc enhancing mass in the angle of the left mandible with invasion of the adjacent mandible bone marrow, surrounding tissue, and masseter muscle. A. Coronal view. B. Axial view.
|
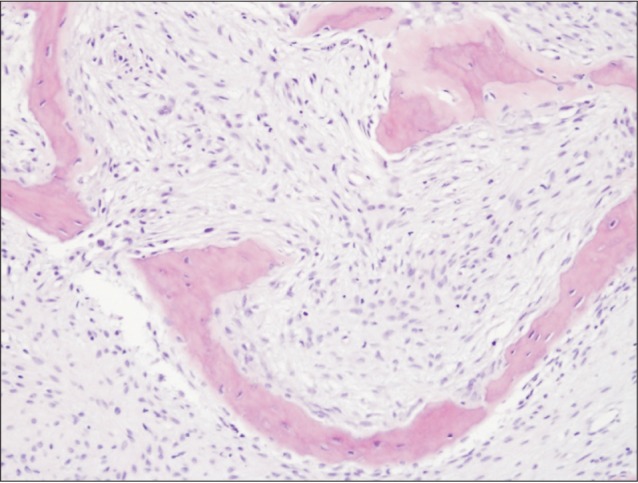 | Fig. 4Histopathologic image of the tibial lesion (H&E staining, ×200).
|
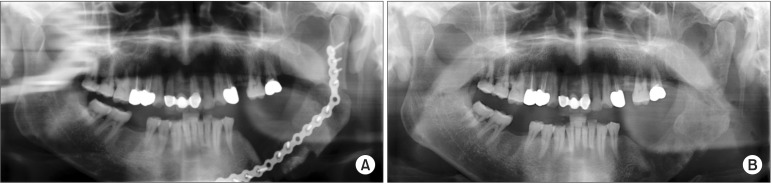
On September, 2011, segmental resection including wide excision of the surrounding soft tissues was performed by a left partial mandibulectomy. After evaluation of the panoramic view, oropharynx CT and oropharynx MRI, a margin of more than 1.5 cm was decided for safety. Simultaneously, a left regional lymph nodes (Level I to partially Level III) was removed in a mass by selective neck dissection.(
Fig. 5) The mandibular condyle was preserved and the position of the mandible was stabilized by a reconstruction plate with a right iliac bone graft.(
Fig. 6. A) On histopathologic examination, all the margins were free of tumor infiltration with no metastatic tumor in the lymph nodes; the final diagnosis was changed to odontogenic carcinosarcoma. After the operation, the patient had a favorable reconstruction result without significant complications. On March 2012, the operation for removal of the reconstruction plate and internal fixation devices was performed.(
Fig. 6. B) Histopathologically, a few soft tissues around the fixation device were identified as inflammatory granulation tissue, but tumor recurrence was not present. Up to now, the patient continues to do well postoperatively.
 | Fig. 5Excised mass with 3.5×3.4×2.5 cm size which included tumor, mandible, and regional lymph node.
|
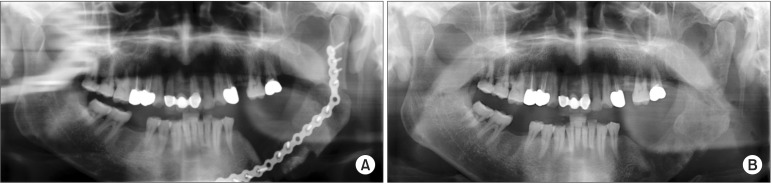 | Fig. 6A. Postoperative (1 month) panoramic view. B. Final postoperative (6 months) panoramic view after plate removal.
|
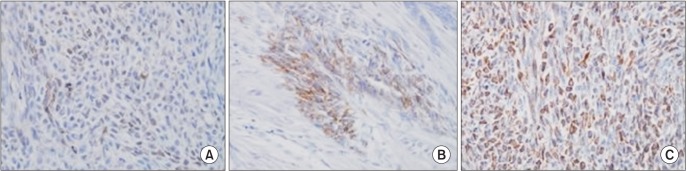
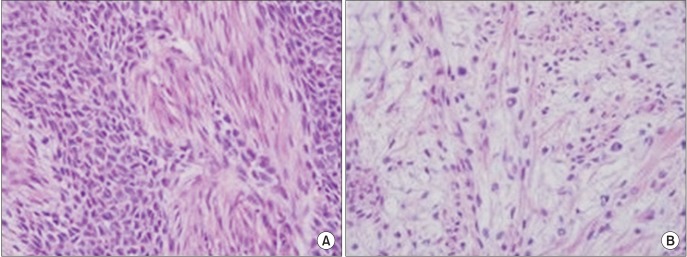
Sections from representative areas of the tumor were stained with H&E. Immunohistochemical studies were also performed using cytokeratin, CAM 5.2, and vimentin. The H&E-stained sections disclosed an invasive tumor consisting of epithelial and mesenchymal neoplastic components. Although the epithelial neoplastic component showed nests and strands similar to ameloblastoma, the tumor cells were obviously malignant cells showing aberrant cytologic atypia, hyperchromasia, and abnormal mitoses.(
Fig. 7. A) The mesenchymal component was morphologically consistent with sarcoma showing marked pleomorphism, enlarged hyperchromatic nuclei, and increased nuclear-to-cytoplasmic ratio. (
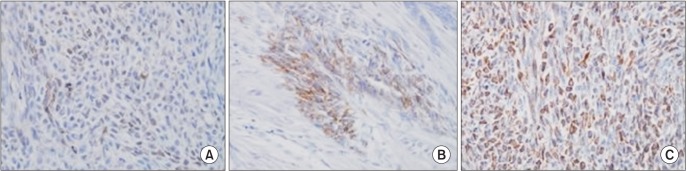
Fig. 7. B) The tumor also invaded into surrounding skeletal muscle and connective tissue. As a whole, these pathologic findings confirmed the diagnosis of odontogenic carcinosarcoma. This diagnosis was supported by positive immunohistochemistry for cytokeratin and CAM 5.2 of carcinomatous element and for vimentin of sarcomatous element.(
Fig. 8)
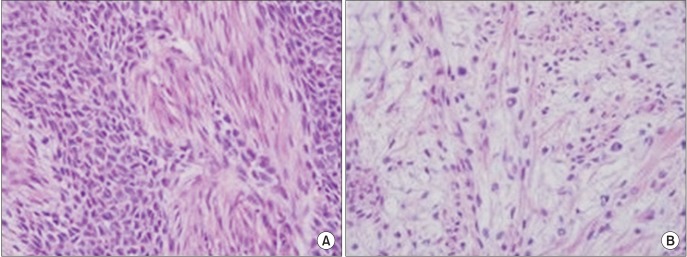 | Fig. 7A. Malignant epithelial component with pleomorphism, enlarged and atypical nuclei (H&E staining, ×400). B. Malignant mesenchymal component with hypercellularity, pleomorphism, enlarged and atypical nuclei (H&E staining, ×400).
|
 | Fig. 8Immunohistochemical stain images (×400). A. Malignant epithelial component. Intense membranous and cytoplasmic staining for cytokeratin. B. Positive staining for CAM 5.2 antigen supporting the diagnosis of malignancy. C. Malignant mesenchymal component showing positivity for vimentin.
|
Go to :

III. Discussion
Odontogenic carcinosarcoma was defined by the 1992 World Health Organization classification of odontogenic tumor as "a very rare neoplasm, similar in pattern to ameloblastic fibrosarcoma, but in which both the epithelial and the ectomesenchymal components show cytological features of malignancy"
9. In other words, the tumor can architecturally resemble an ameloblastic fibroma in which both the epithelial and the mesenchymal components show cytologic evidence of malignancy.
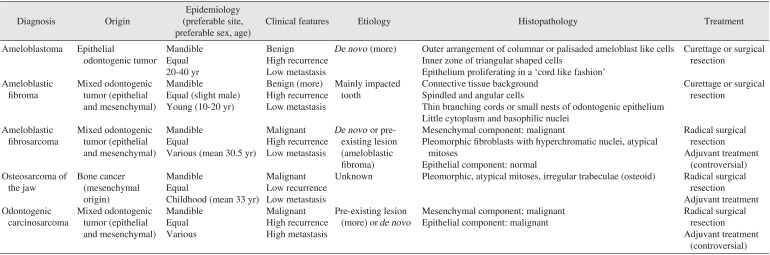
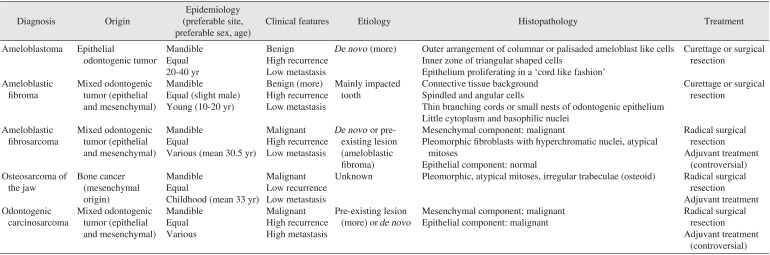
Extremely rare lesion and related neoplasms such as ameloblastoma, ameloblastic fibroma, ameloblastic fibrosarcoma, and osteosarcoma are summarized in
Table 1 to avoid confusion later on. They occur mainly in the mandible, are seen equally in both sexes, and have high recurrence rates except for osteosarcoma. Furthermore, the tumors may arise
de novo or from pre-existing lesions.
De novo odontogenic tumors arise from remnants that originated in the embryologic process of odontogenesis. The process of odontogenesis involves reciprocal inductive interaction and is thought to play a role in the development of odontogenic neoplasms. In pre-existing lesions, malignant transformation usually becomes clinically manifest as a recurrent tumor. In terms of origin and histopathology, ameloblastoma demonstrates epithelial cytologic features of a benign tumor which grows locally invasive, while ameloblastic fibroma exhibits features of a benign mixed odontogenic tumor which consists of odontogenic epithelial and mesenchymal cells. Ameloblastic fibrosarcoma, a rare malignant odontogenic neoplasm consisting of epithelial and mesenchymal components, is characterized by malignant activity in the mesenchyme only. Osteosarcoma of the jaw is the most common malignant bone tumor arising from primitive transformed cells of the mesenchyme that exhibit osteoblastic differentiation and produce malignant osteoid. Finally, odontogenic carcinosarcoma has distinctively malignant activity in both components and high potential of metastasis.
Table 1
Summary of the differential diagnosis for odontogenic carcinosarcoma
|
Diagnosis |
Origin |
Epidemiology (preferable site, preferable sex, age) |
Clinical features |
Etiology |
Histopathology |
Treatment |
|
Ameloblastoma |
Epithelial odontogenic tumor |
Mandible |
Benign |
De novo (more) |
Outer arrangement of columnar or palisaded ameloblast like cells |
Curettage or surgical resection |
|
Equal |
High recurrence |
Inner zone of triangular shaped cells |
|
20-40 yr |
Low metastasis |
Epithelium proliferating in a 'cord like fashion' |
|
Ameloblastic fibroma |
Mixed odontogenic tumor (epithelial and mesenchymal) |
Mandible |
Benign (more) |
Mainly impacted tooth |
Connective tissue background |
Curettage or surgical resection |
|
Equal (slight male) |
High recurrence |
Spindled and angular cells |
|
Young (10-20 yr) |
Low metastasis |
Thin branching cords or small nests of odontogenic epithelium |
|
Little cytoplasm and basophilic nuclei |
|
Ameloblastic fibrosarcoma |
Mixed odontogenic tumor (epithelial and mesenchymal) |
Mandible |
Malignant |
De novo or pre-existing lesion (ameloblastic fibroma) |
Mesenchymal component: malignant |
Radical surgical resection |
|
Equal |
High recurrence |
Pleomorphic fibroblasts with hyperchromatic nuclei, atypical mitoses |
Adjuvant treatment (controversial) |
|
Various (mean 30.5 yr) |
Low metastasis |
Epithelial component: normal |
|
Osteosarcoma of the jaw |
Bone cancer (mesenchymal origin) |
Mandible |
Malignant |
Unknown |
Pleomorphic, atypical mitoses, irregular trabeculae (osteoid) |
Radical surgical resection |
|
Equal |
Low recurrence |
Adjuvant treatment |
|
Childhood (mean 33 yr) |
Low metastasis |
|
Odontogenic carcinosarcoma |
Mixed odontogenic tumor (epithelial and mesenchymal) |
Mandible |
Malignant |
Pre-existing lesion (more) or de novo
|
Mesenchymal component: malignant |
Radical surgical resection |
|
Equal |
High recurrence |
Epithelial component: malignant |
Adjuvant treatment (controversial) |
|
Various |
High metastasis |

In general, these tumors are primarily treated by surgical resection. The effectiveness of adjuvant therapy remains controversial. In particular, radiation therapy carries the possibility of inducing oncogenesis, and ameloblastic series have potential capacity for the radiation resistance
8. In other words, adjuvant therapy may contribute to recurrence and malignant transformation.
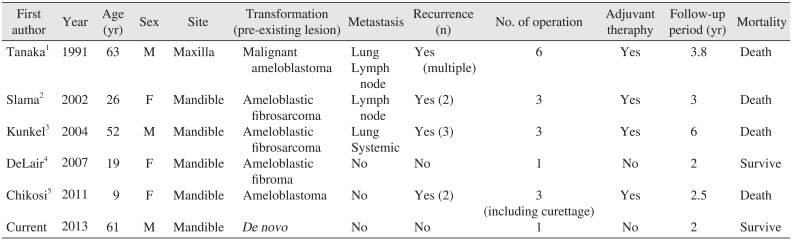
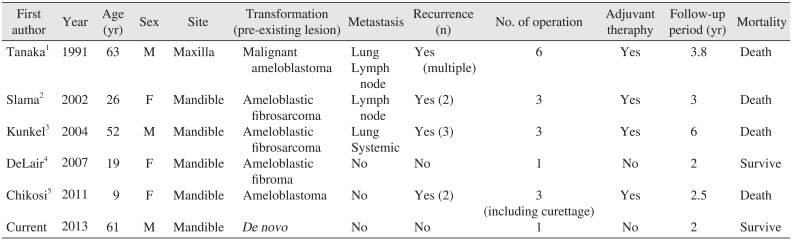
Given the scarcity of reported cases, odontogenic carcinosarcoma is difficult to characterize. In a retrospective study of a few cases (
Table 2)
12345, the patients' ages ranged from 9 to 63 years, and there was no gender preference. It was more common in the mandible, and mainly believed to progress from related neoplasms. The pathogenesis of malignant transformation is not completely understood, but it is considered to occur after multiple recurrences and surgical treatments. Nevertheless, the tumor may arise
de novo such as in the present case without previous disease and surgical intervention.
Table 2
Summary of clinical features of reported cases of odontogenic carcinosarcoma
|
First author |
Year |
Age (yr) |
Sex |
Site |
Transformation (pre-existing lesion) |
Metastasis |
Recurrence (n) |
No. of operation |
Adjuvant theraphy |
Follow-up period (yr) |
Mortality |
|
Tanaka1
|
1991 |
63 |
M |
Maxilla |
Malignant ameloblastoma |
Lung |
Yes (multiple) |
6 |
Yes |
3.8 |
Death |
|
Lymph node |
|
Slama2
|
2002 |
26 |
F |
Mandible |
Ameloblastic fibrosarcoma |
Lymph node |
Yes (2) |
3 |
Yes |
3 |
Death |
|
Kunkel3
|
2004 |
52 |
M |
Mandible |
Ameloblastic fibrosarcoma |
Lung |
Yes (3) |
3 |
Yes |
6 |
Death |
|
Systemic |
|
DeLair4
|
2007 |
19 |
F |
Mandible |
Ameloblastic fibroma |
No |
No |
1 |
No |
2 |
Survive |
|
Chikosi5
|
2011 |
9 |
F |
Mandible |
Ameloblastoma |
No |
Yes (2) |
3 (including curettage) |
Yes |
2.5 |
Death |
|
Current |
2013 |
61 |
M |
Mandible |
De novo
|
No |
No |
1 |
No |
2 |
Survive |

In previously published cases, the tumor has a fatality rate of more than 50% with high rates of recurrence and metastasis. Aside from two cases, all the other patients died. However, DeLair et al.
4 and present cases without evidence of recurrence or metastasis after the first operation without use of adjuvant therapy. Moreover, the clinical behavior of the tumors was favorable. Due to the short follow-up period in these 2 cases, these results were not able to be confirmed.
In summary, this is a case report of a rare occurrence of odontogenic carcinosarcoma. This malignant tumor shows mixed features of both carcinomatous and sarcomatous elements on histopathological study, and is clinically very aggressive features with high rates of recurrence and metastasis. However, the current case resulted in a favorable clinical prognosis. If the tumor is detected at an early stage and has mild features, then adequate surgical treatment alone may lead to good outcomes. A larger number of cases and prolonged follow-up are need to further clarify the nature of odontogenic carcinosarcoma.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download