Abstract
Objectives
The purpose of this study was to clarify which findings in magnetic resonance imaging (MRI) are good predicators of pain and mouth opening limitation in patients with temporomandibular joint (TMJ) internal derangement (ID).
Materials and Methods
Clinical examinations for pain and mouth opening limitation were conducted for suspected TMJ ID. MRI scans were taken within a week of clinical examinations. On the oblique-sagittal plane image, readings were obtained in terms of the functional aspect of disc position, degree of displacement, disc deformity, joint effusion, and osteoarthrosis. Multiple logistic regression analyses were conducted to identify the predictors of pain and mouth opening limitation.
Results
A total of 48 patients (96 TMJs) were studied, including 39 female patients and 9 male patients whose ages ranged from 10 to 65 years. The resultant data showed significant correlations between pain and the MR imaging of the degree of disc displacement (P<0.05). The probability of there being pain in moderate to significant cases was 9.69 times higher than in normal cases. No significant correlation was found between mouth opening limitation and MRI findings.
Temporomandibular joint disorder (TMD) is a clinical condition involving the temporomandibular joint (TMJ), masticatory musculature, and surrounding structures that affects approximately 5% to 12% of the total population12. TMJ internal derangement (ID) refers to an abnormal relationship between the articular disc and the mandibular condyle, and is reportedly the most common type of TMD3. Approximately 80% of symptomatic TMD patients present with TMJ ID4. The common clinical symptoms of TMJ ID include pain, restricted range of motion, and joint sound. Concurrent pain and the restricted range of motion have significant effects on the patient's daily life and quality of life and thus, require appropriate diagnostic techniques and medical intervention.
Magnetic resonance imaging (MRI) is currently the most reliable diagnostic approach for TMJ ID due to its ability to visualize any morphological and positional changes of the articular disc, as well as changes in soft tissues, including synovial fluids. In 1993, Tasaki and Westesson5 assessed the accuracy of MRI using autopsy specimens. They reported that MRI has approximately 95% accuracy for disk position and disc form and about 93% for osseous change.
Several studies have evaluated the correlation of diagnostic MRI with clinical symptoms such as pain and restricted mouth opening. Emshoff et al.6 analyzed the correlation between TMJ pain and MRI findings, and reported that the MRI findings of osteoarthritis, joint effusion, and bone marrow edema were correlated with TMJ pain. Westesson and Brooks7 focused on the correlation between MRI findings and joint pain or disc displacement, and reported that joint effusion found in MRI scans was highly correlated with joint pain.
Most of the preceding studies used univariate analyses to establish correlations between MRI findings and clinical symptoms. However, the symptoms of TMJ ID are often affected simultaneously by various causes and univariate analysis alone is limited in its ability to identify symptom predictors. The purpose of this study was to clarify which of the 5 findings in MRI scans (i.e., functional aspect of disc position, degree of displacement, disc deformity, joint effusion, and osteoarthrosis) are good predicators of pain and mouth opening limitation in patients with TMJ ID, using multivariate analysis. Furthermore, unlike the preceding studies, we looked for effects of the degree of disc displacement on clinical symptoms.
Clinical examinations were conducted on cases of suspected TMD among patients who presented with discomfort in the TMJ region, at the Department of Oral and Maxillofacial Surgery in Ajou University Hospital between January 2013 and October 2013. All patients were asked to complete a questionnaire concerning the clinical symptoms of TMD, and underwent clinical examinations for pain and mouth opening limitation, performed by a clinician. Criteria for including a patient in the study were (a) report of orofacial pain referred to the TMJ, (b) the presence or history of joint sound, or (c) the presence or history of jaw locking. Criteria for excluding a patient were (a) signs and symptoms that characterized a diagnosis of myalgia, (b) a history of trauma, or (c) a history of previous treatment. All potential patients were reviewed retrospectively and 48 patients (96 TMJs) were included in the final screening.
As a diagnostic criterion, a painful joint was defined as orofacial pain caused by TMD together with pain on TMJ palpation, function, jaw movement, and/or parafunction. Mouth opening limitation was defined as having <35 mm of unassisted movement on clinical examinations and a past history of mouth opening limitation.
MRI scans were taken within a week of clinical examinations. Images were taken with a matrix of 256×256 and cut of 2.50 mm thickness and 3.00 mm space with the GE HDxt 1.5 Tesla MRI Scanner (GE Healthcare, Milwaukee, WI, USA). Three images including coronal fast spin echo proton, oblique-sagittal proton, and oblique-sagittal T2 were taken with the mouth closed and 4 images including coronal fast spin echo proton, oblique-sagittal proton, oblique-sagittal T2, and oblique-sagittal T2 with fat saturation were taken with the mouth open in a routine sequence.
A radiologist blinded to clinical examination results interpreted the acquired images. On the oblique-sagittal plane image passing the center of the condyle, readings were obtained in terms of the functional aspect of the disc position, degree of displacement, disc deformity, joint effusion, and osteoarthrosis. The respective criteria for reading were as follows.
1. The functional aspect of disc position was classified as either normal, anterior disc displacement with reduction (ADDWR), or anterior disc displacement without reduction (ADDWOR) depending upon changes in disc position and the presence of reduction in the closed- and open-mouth positions7.
2. The degree of disc displacement was assessed in the closed-mouth position. A line was drawn between the summits of the posterior glenoid tubercle and the articular eminence, and the point considered as the most central point of the condyle was set as its midpoint. A line from the midpoint to the most superior point of the condyle was set as a vertical line, and a line from the posterior margin of the disc to the midpoint as the posterior line. The angle between the vertical line and the posterior line was defined as the degree of disc displacement. Where the degree of disc displacement was 0°-10°, 11°-50°, and ≥51°, it was regarded as normal disc position, slight to mild anterior disc displacement, and moderate to significant anterior disc displacement, respectively8.
3. Joint effusion was measured in the closed mouth position. The following classification criteria were applied on the basis of the area in which high signals of upper or lower joint space appeared in T2-weighted fat-saturated images. Absent joint effusion was defined as the absence of high signal intensity areas or the lining or spot of high intensity along the articular surface. Present joint effusion was defined as the presence of a band of high intensity or collection with pooling in the compartment7.
4. Presence of disc deformity was defined as the condition in which the disc exhibited morphological changes such as being folded, lengthened, round, biconvex, or having a thick posterior band8.
5. Osteoarthrosis was defined as the condition in which flattening, osteophyte formation, subchondral sclerosis, irregularity, or erosion was found on the articular surface3.
Five types of statistical analyses were performed to compare significant correlations between pain/mouth opening limitation and MRI images. First, in order to determine the correlation between pain and the functional aspect of disc displacement, the degrees of disc displacement, joint effusion, disc deformities, or osteoarthrosis were analyzed and chi-square analyses and linear by linear association analyses were carried out. In addition, multiple logistic regression analyses were conducted to determine whether the degree of disc displacement, joint effusion, disc deformities, or osteoarthrosis are pain predictors. Since the functional aspect of disc displacement and the degree of disc displacement have similar statistical characteristics, it was expected that interactions between the variables would occur; for this reason, the functional aspect of disc displacement was excluded from the multiple logistic regression analysis.
Similarly, chi-square analyses and linear by linear association analyses were performed for the comparative correlation between mouth opening limitation and MRI images. In addition, multiple logistic regression analyses were conducted to identify the predictors of mouth opening limitation.
Furthermore, to ascertain a correlation between mouth opening limitation and ADDWOR, chi-square analyses were conducted. The patients with ADDWOR in either TMJ or both were placed in the "present" group and the patients without ADDWOR in either TMJ were placed in the "absent" group. A correlation between ADDWOR and mouth opening limitation was subsequently evaluated. The analyses used IBM SPSS Statistics version 22.0 (IBM Co., Armonk, NY, USA). This study was reviewed and approved by the institutional review board of Ajou University Hospital (AJIRBMED-MDB-14-308).
A total of 48 patients (96 TMJs) were studied, including 39 female patients (81%) and 9 male patients (19%), whose ages ranged from 10 to 65 years (mean age, 29 years and 7 months).
Correlations between pain and the functional aspect of disc displacement, the degree of disc displacement, joint effusion, disc deformities, or osteoarthrosis were conducted by chi-square analyses and linear by linear association analyses. Statistically significant results were obtained for the functional aspect of disc displacement (P<0.001). In nonpainful joints, absent ranked first followed by ADDWR and ADDWOR, while in painful joints, ADDWOR ranked first followed by ADDWR and absent. The results concerning the degree of disc displacement were statistically significant (P<0.001). In nonpainful joints, normal was the most common, followed by slight to mild and moderate to significant, whereas in painful joints, moderate to significant was the most common, followed by slight to mild and normal. The results of joint effusion were statistically significant (P<0.05). In both nonpainful and painful joints, absent joint effusion was more frequent; however, in nonpainful joints, the gap between the two groups was greater. The results of disk deformities were statistically significant (P<0.001). In both nonpainful joints and painful joints, the absence of disk deformity was more frequent; however, in painful joints, the gap between the two classifications was greater. The analyses showed that osteoarthrosis had no significant correlation with pain.(Table 1)
Determination of pain predictors was conducted by multiple logistic regression analyses. The entire model was statistically significant (P<0.001). The degrees of disc displacement were statistically significant (P<0.05), and the probability of being painful in moderate to significant cases was 9.69 times higher than in normal cases, which is a statistically significant difference (P<0.05).(Table 2)
Correlations between mouth opening limitation and functional aspect of disc displacement, degree of disc displacement, joint effusion, disc deformities, or osteoarthrosis were determined by chi-square analyses as well as linear by linear association analyses. Statistically significant results were obtained for the functional aspect of disc displacement (P<0.001). In the case of no mouth opening limitation ('no'), ADDWR ranked first, followed by absent and ADDWOR, whereas in the case of measurable mouth opening limitation ('yes'), ADDWOR was the most dominant, followed by absent and ADDWR. The results regarding the degree of disc displacement were statistically significant (P<0.05). In 'no' cases, slight to mild was the most common, followed by moderate to significant and normal, while in 'yes' cases, moderate to significant was the most common, followed by normal and slight to mild. The analyses showed that joint effusion, disc deformities, or osteoarthrosis had no correlation with mouth opening limitation.(Table 3)
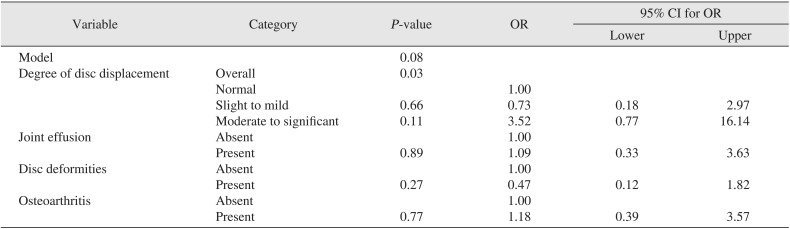
Multiple logistic regression analyses were conducted to find predictors of mouth opening limitation; however, the entire model was not significant.(Table 4)
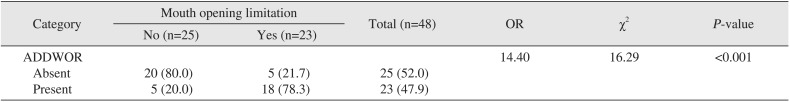
The results of chi-square analyses for any correlation between mouth opening limitation and ADDWOR were statistically significant (P<0.001). In 'no' cases, absent was the most frequent, while in 'yes' cases, present was the most frequent. The probability of having mouth opening limitation was 14.40 times higher in ADDWOR cases than in non-ADDWOR cases.(Table 5)
We conducted two types of analyses to determine correlations between disc displacement and pain in patients with ID. First, a classification was made on the basis of the presence or absence of disc reduction during functional movement. Analysis showed that painful joints were more frequent in the ADDWR group than in the normal group, and in the ADDWOR than in the ADDWR group. These findings were consistent with previously reported results. Emshoff et al.36 reported that there was a correlation between pain and disc displacement in their series. They also reported that the possibility of pain varies with the type of ID and that, in the presence of ADDWOR, the risk of pain was higher, as compared to with ADDWR. They further described that, specifically, among patients with ADDWOR, those with concurrent osteoarthrosis and bone marrow edema or with concurrent osteoarthrosis and effusion had a significantly increased probability of pain. Similarly, Roh et al.9 reported that the incidence of pain increased significantly in patients with anterior disc displacement, and Farina et al.10 corroborated their results. Taşkaya-Yilmaz and Oğütcen-Toller11 reported that the likelihood of joint pain was increased in patients with ADDWOR, as compared to those with ADDWR. These results suggested that a greater degree of anterior disc displacement is associated with a higher probability of pain. In this context, the current study analyzed the statistically significant correlation between the degree of anterior disc displacement and the presence of pain. Our results indicated that the possibility of pain significantly increases with the greater degree of anterior disc displacement. Although there are few studies that have directly compared the degree of disc displacement and presence of pain, the presumption is that that severity in degree of anterior disc displacement is associated with a higher probability of ADDWOR, leading to a higher risk of pain.
Joint effusion is detected in T2-weighted MRI scans, and is observed in about 30 to 80% of patients with TMD12. Segami et al.121314 asserted that joint effusion represents the synovitis of the TMJ. Several studies have reported that there is a correlation between joint effusion and pain, and that joint effusion occurs in about 46 to 80% of painful joints3715. Similarly, in this study, a strong correlation between the presence of pain and joint effusion was seen, and joint effusion was found in approximately 24% of painful joints. However, it has been previously reported that joint effusion had no significant correlation with the severity of pain1216, and that the greater degree of anterior disc displacement was associated with a higher probability of joint effusion717. Because the linings or spots of intensity are occasionally seen in about 7% of normal TMJs7, the cases with linings or spots of high intensity were classified as having no joint effusion in this study.
Of the 96 TMJ discs included in the current study, the cases with no deformity accounted for about 26.04% (25 discs); the cases with a folded disc for 28.13% (27 discs); the cases with a lengthened disc were 12.50% (12 discs); the cases with a rounded disc were 3.13% (3 discs); the cases with a biconvex disc were 2.08% (2 discs); and the cases with a disc with a thick posterior band were 28.13% (27 discs). We found that the possibility of pain increased significantly in the presence of disc deformity. Although there have been few studies that directly addressed this issue, some studies suggested that disc deformity reflects the severity of ID111718. Santos et al.17 reported that the morphological changes of the disc were correlated with disc position. In their study, in the case of ADDWOR, the rate of folded disc was remarkably high as compared to that of normal position disc. In addition, they reported that there was a correlation between disc form and the sideways position of the disc, and specifically, when the disc was in the medial position, the incidence of folded disc was significantly increased. Taşkaya-Yilmaz and Oğütcen-Toller11 reported that the frequency of disc deformity increased in TMJs corresponding to ADDWOR, as compared to ADDWR. They reported that different types of disc deformities were seen depending on the aspect of ID and specifically, lengthened discs were found in 56.75% of ADDWR cases while folded or round disc forms were dominant among ADDWOR cases. It is thought that the greater degree of anterior disc displacement is associated with a higher probability of severe morphological changes to the disc and thus, pain.
It was reported that osteoarthrosis was not observed in patients without ID, indicating a strong correlation between osteoarthrosis and ID19. Many studies suggested that there is a strong correlation between ADDWOR and osteoarthrosis, and specifically reported that pain increased significantly in patients with ADDWOR in concurrence with osteoarthrosis320212223. Nevertheless, such a correlation between osteoarthrosis and the possibility of pain remains uncertain. Campos et al.23 claimed that osteoarthrosis was not always a fundamental factor of TMJ pain because degenerative bony changes were seen even in asymptomatic joints. A multivariate analysis performed by Emshoff et al.3 also showed that the effects of osteoarthrosis on pain were insignificant. Farina et al.10 interpreted the paradoxical phenomenon as being caused by the fact that, while osteoarthrosis mostly appears in the advanced stage, TMJ pain tends to decrease in the advanced stage.
Multiple logistic regression analyses showed that the degree of disc displacement alone had a statistically significant correlation with pain. When the degree of anterior disc displacement was ≥51°, the likelihood of pain increased sharply (odds ratio=9.69:1). This result is supported by some other studies. Oğütcen-Toller et al.24 compared the degree of anterior disc displacement and MRI images and showed that degenerative condylar change increased with the degree of anterior disc displacement and that ADDWOR existed in all the cases where the degree of anterior disc displacement was at least 80°. The degree of anterior disc displacement is proportional to increasing ADDWOR and degenerative changes, and thus, the probability of pain. Emshoff et al.25 performed a multivariate analysis to evaluate pain predictors and found that pain had a highly significant correlation with ADDWOR (odds ratio=10.2:1; P=0.007) and bone marrow edema (odds ratio=15.6:1; P=0.003).
Taken together, it appears that pain had a highly significant correlation with the degree of anterior disc displacement, joint effusion, and disc deformity. Most of all, it appears that a high degree of anterior disc displacement (≥51°) is most valuable as a pain predictor. Anterior disc displacement could be a normal variant in the balanced environment between adaptive capacity and functional demand. Once such a balance is tipped, TMJ can switch from adaptation to destruction. Severe anterior disc displacement may increase micro and macro damage to the TMJ and surrounding structures (i.e., retrodiscal tissue), and results in synovitis. Pain is the typical result of inflammation and the likelihood of pain may be increased with inflammatory changes of the TMJ and surrounding structures.
The results of this study suggest that there is a correlation between mouth opening limitation and the functional aspect of disc displacement or the degree of displacement. Specifically, it was found that the possibility of mouth opening limitation increased significantly if ADDWOR existed in either or both of the TMJs. Campos et al.23 also showed a strong correlation between TMJ hypomobility and ADDWOR. Both of these results suggest that severe anterior disc displacement may have effects on mouth opening limitation. However, the correlation between anterior disc displacement and mouth opening limitation is still unclear. Roh et al.9 reported that there was no statistically significant difference in the maximum and comfortable mouth opening range among normal, ADDWR, and ADDWOR groups. Multiple logistic regression analysis in our study showed no significant results for anterior disc displacement and mouth opening limitation. The inconsistency of results between studies can be attributed to confounding factors such as muscular dysfunction or TMJ tissue remodeling. Further studies on various confounding factors that may affect mouth opening limitation are required.
As a retrospective study, this study had the limitations of having only a small sample size of the Korean population. Moreover, possible errors in clinical examinations and image reading were not taken into account.
We identified a significant correlation between clinical symptoms and MRI findings of ID. The degree of anterior disc displacement may be useful for predicting pain in patients with TMJ ID. Nevertheless, MRI findings are not the only predictor of clinical symptoms, and MRI cannot explain all the manifestations of ID. Therefore, MRI should be used cautiously for correct diagnosis.
References
1. Barclay P, Hollender LG, Maravilla KR, Truelove EL. Comparison of clinical and magnetic resonance imaging diagnosis in patients with disk displacement in the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 88:37–43. PMID: 10442943.
2. Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. International RDC/TMD Consortium Network, International Association for Dental Research. Orofacial Pain Special Interest Group, International Association for the Study of Pain. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache. 2014; 28:6–27. PMID: 24482784.
3. Emshoff R, Brandlmaier I, Bertram S, Rudisch A. Relative odds of temporomandibular joint pain as a function of magnetic resonance imaging findings of internal derangement, osteoarthrosis, effusion, and bone marrow edema. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 95:437–445. PMID: 12686927.

4. Paesani D, Westesson PL, Hatala M, Tallents RH, Kurita K. Prevalence of temporomandibular joint internal derangement in patients with craniomandibular disorders. Am J Orthod Dentofacial Orthop. 1992; 101:41–47. PMID: 1731487.

5. Tasaki MM, Westesson PL. Temporomandibular joint: diagnostic accuracy with sagittal and coronal MR imaging. Radiology. 1993; 186:723–729. PMID: 8430181.

6. Emshoff R, Innerhofer K, Rudisch A, Bertram S. Relationship between temporomandibular joint pain and magnetic resonance imaging findings of internal derangement. Int J Oral Maxillofac Surg. 2001; 30:118–122. PMID: 11405446.

7. Westesson PL, Brooks SL. Temporomandibular joint: relationship between MR evidence of effusion and the presence of pain and disk displacement. AJR Am J Roentgenol. 1992; 159:559–563. PMID: 1503025.

8. Incesu L, Taşkaya-Yilmaz N, Oğütcen-Toller M, Uzun E. Relationship of condylar position to disc position and morphology. Eur J Radiol. 2004; 51:269–273. PMID: 15294336.

9. Roh HS, Kim W, Kim YK, Lee JY. Relationships between disk displacement, joint effusion, and degenerative changes of the TMJ in TMD patients based on MRI findings. J Craniomaxillofac Surg. 2012; 40:283–286. PMID: 21745748.

10. Farina D, Bodin C, Gandolfi S, De Gasperi W, Borghesi A, Maroldi R. TMJ disorders and pain: assessment by contrast-enhanced MRI. Eur J Radiol. 2009; 70:25–30. PMID: 18329212.

11. Taşkaya-Yilmaz N, Oğütcen-Toller M. Magnetic resonance imaging evaluation of temporomandibular joint disc deformities in relation to type of disc displacement. J Oral Maxillofac Surg. 2001; 59:860–865. PMID: 11474436.
12. Segami N, Nishimura M, Kaneyama K, Miyamaru M, Sato J, Murakami KI. Does joint effusion on T2 magnetic resonance images reflect synovitis? Comparison of arthroscopic findings in internal derangements of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 92:341–345. PMID: 11552156.

13. Segami N, Miyamaru M, Nishimura M, Suzuki T, Kaneyama K, Murakami K. Does joint effusion on T2 magnetic resonance images reflect synovitis? Part 2. Comparison of concentration levels of proinflammatory cytokines and total protein in synovial fluid of the temporomandibular joint with internal derangements and osteoarthrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 94:515–521. PMID: 12374930.

14. Segami N, Suzuki T, Sato J, Miyamaru M, Nishimura M, Yoshimura H. Does joint effusion on T2 magnetic resonance images reflect synovitis? Part 3. Comparison of histologic findings of arthroscopically obtained synovium in internal derangements of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 95:761–766. PMID: 12789161.

15. Takahashi T, Nagai H, Seki H, Fukuda M. Relationship between joint effusion, joint pain, and protein levels in joint lavage fluid of patients with internal derangement and osteoarthritis of the temporomandibular joint. J Oral Maxillofac Surg. 1999; 57:1187–1193. PMID: 10513864.

16. Güler N, Uçkan S, Imirzalioğlu P, Açikgözoğlu S. Temporomandibular joint internal derangement: relationship between joint pain and MR grading of effusion and total protein concentration in the joint fluid. Dentomaxillofac Radiol. 2005; 34:175–181. PMID: 15897289.

17. Santos KC, Dutra ME, Warmling LV, Oliveira JX. Correlation among the changes observed in temporomandibular joint internal derangements assessed by magnetic resonance in symptomatic patients. J Oral Maxillofac Surg. 2013; 71:1504–1512. PMID: 23948363.

18. Murakami S, Takahashi A, Nishiyama H, Fujishita M, Fuchihata H. Magnetic resonance evaluation of the temporomandibular joint disc position and configuration. Dentomaxillofac Radiol. 1993; 22:205–207. PMID: 8181648.

19. Brooks SL, Westesson PL, Eriksson L, Hansson LG, Barsotti JB. Prevalence of osseous changes in the temporomandibular joint of asymptomatic persons without internal derangement. Oral Surg Oral Med Oral Pathol. 1992; 73:118–122. PMID: 1603550.

20. Taşkaya-Yýlmaz N, Oğütcen-Toller M. Clinical correlation of MRI findings of internal derangements of the temporomandibular joints. Br J Oral Maxillofac Surg. 2002; 40:317–321. PMID: 12175833.

21. Cortés D, Exss E, Marholz C, Millas R, Moncada G. Association between disk position and degenerative bone changes of the temporomandibular joints: an imaging study in subjects with TMD. Cranio. 2011; 29:117–126. PMID: 21661586.

22. Moncada G, Cortés D, Millas R, Marholz C. Relationship between disk position and degenerative bone changes in temporomandibular joints of young subjects with TMD. An MRI study. J Clin Pediatr Dent. 2014; 38:269–276. PMID: 25095324.

23. Campos MI, Campos PS, Cangussu MC, Guimarães RC, Line SR. Analysis of magnetic resonance imaging characteristics and pain in temporomandibular joints with and without degenerative changes of the condyle. Int J Oral Maxillofac Surg. 2008; 37:529–534. PMID: 18440778.

24. Oğütcen-Toller M, Taşkaya-Yilmaz N, Yilmaz F. The evaluation of temporomandibular joint disc position in TMJ disorders using MRI. Int J Oral Maxillofac Surg. 2002; 31:603–607. PMID: 12521315.
25. Emshoff R, Brandlmaier I, Gerhard S, Strobl H, Bertram S, Rudisch A. Magnetic resonance imaging predictors of temporomandibular joint pain. J Am Dent Assoc. 2003; 134:705–714. PMID: 12839406.

Table 1
Correlation between pain and each of the magnetic resonance imaging findings (univariate analysis)
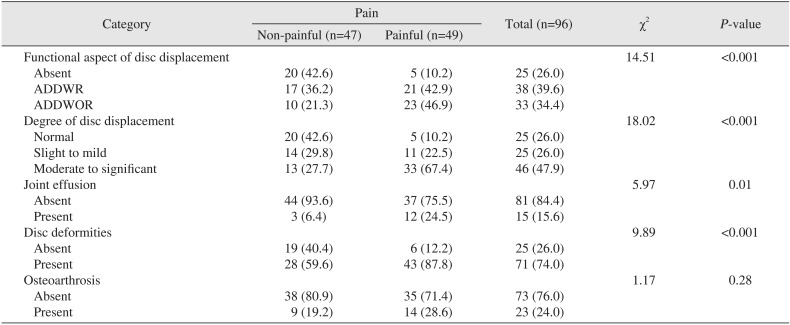
Table 2
Correlation between pain and each of the magnetic resonance imaging findings (multivariate analysis)
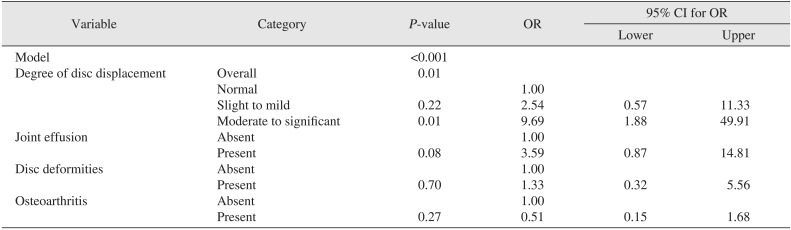
Table 3
Correlation between mouth opening limitation and each of the magnetic resonance imaging findings (univariate analysis)
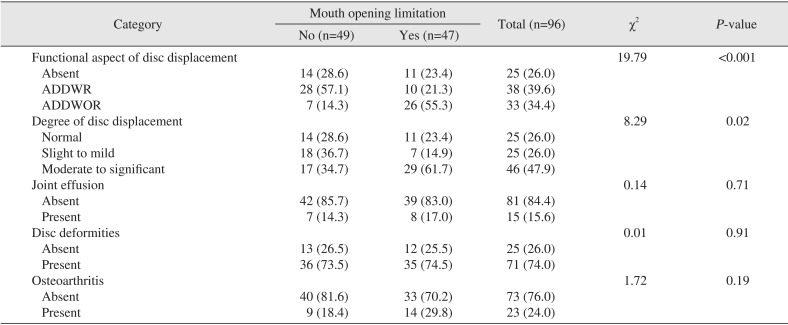
Table 4
Correlation between mouth opening limitation and each of the magnetic resonance imaging findings (multivariate analysis)




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download