Abstract
Odontoma is the most common odontogenic benign tumor, and the treatment of choice is generally surgical removal. After excision, bone grafts may be necessary depending on the need for further treatment, or the size and location of the odontoma. Although the osteogenic capacity of a demineralized tooth was verified as early as 1967 by Urist and many other investigators, the cumbersome procedure, including a long demineralization time, may be less than comfortable for clinicians. A modified ultrasonic technology, with periodic negative pressure and temperature control, facilitated rapid and aseptic preparation of demineralized teeth for bone grafts. This approach reduces the demineralization time dramatically (≤80 minutes), so that the graft material can be prepared chairside on the same day as the extraction. The purpose of this article is to describe two cases of large compound odonotomas used as graft material prepared chairside for enucleation-induced bony defects. These two clinical cases showed favorable wound healing without complications, and good bony support for future dental implants or orthodontic treatment. Finally, this report will suggest the possibility of recycling the benign pathologic hard tissue as an alternative treatment option for conventional bone grafts in clinics.
Odontoma is the most common odontogenic benign tumor1,2,3 containing "tooth-like tissues"2,3. It is not considered a true neoplasm, and is thus classified as a hamartoma or a malformation of odontogenic tissues2,3,4.
The etiology of this disease is still unknown, but many factors have been considered as playing important roles in its pathogenesis, including local trauma, infection, and genetics. The diagnosis may be made during routine radiological exams due to the delayed eruption of the primary or permanent teeth4,5. Radiological characteristics include the presence of an irregular mass surrounded by a thin radiolucent capsular space and the presence of radiopaque compact bone4,5.
The treatment of choice has been surgical removal, depending on the size and location of the odontoma, and bone grafts are necessary to reconstruct the alveolar ridge and prepare the region for future dental implants or orthodontic treatment2,3,4,5.
The graft material for the defect is categorized into 4 types; autogenous, allogenic, xenogenic bones, and alloplastic materials. Although autogenous bone is considered the gold standard among graft materials due to its osteoinductivity, osteoconductivity, and osteogenicity, it has some limitations, such as its high morbidity and potential resorption. To compensate for these limitations, extracted human teeth have been spotlighted as a novel graft material due to their physicochemical to bone. The osteogenic capacity of demineralized teeth was verified as early as 19676, and it is generally accepted that autogenous and allogenic demineralized teeth are osteoinductive or osteoconductive graft materials6,7,8. Commercial materials based on demineralized teeth have been recently used in human trials6,9.
The chemical composition of dentin is very similar to that of bone. In dentin, 70%-75% of the content is inorganic, 20% is organic, and up to 10% is water; in alveolar bone, the contents of these components are 65%, 25%, and 10%, respectively10. With respect to organic content, dentin and cementum include type I collagens and various growth factors such as bone morphogenic proteins. In addition, the noncollagenous proteins in dentin are able to trigger the bone resorption and mineralization process11.
Among the inorganic contents, the mineral components providing the biomechanical backbone are still important factors for cell differentiation, for the nidus of calcification, and for maintaining space during new bone formation12. Considering the hierarchical structures of bone, the mineralized collagen matrix with functional proteins and proper fibrillar arrays for biomechanics may be suitable as a natural bioinspired graft material in bone tissue engineering13.
Commercial materials based on demineralized teeth have been recently used in human trials, but have some shortcomings. These include long preparation times, limited productivity for tissue bank preparation and an increase in cost. Based on several efforts to reduce the time for demineralization, a modified ultrasonic technology with periodic negative pressure and temperature control was developed14. This approach dramatically reduced the demineralization time (≤80 minutes), so that graft material can be prepared chairside on the same day as an extraction.
Herein, we report two cases of large compound odontomas which were used as graft material prepared chairside for enucleation-induced bony defects. The goal of these reports was to suggest the possibility of recycling benign pathologic hard tissue as an alternative treatment option for conventional bone grafts in clinics.
This study was approved by the Dankook University Jukjeon Dental Hospital institutional review board (D-2011-02-002) and all participants signed an informed consent agreement.
A 41-year-old Korean female was referred to the Department of Oral and Maxillofacial Surgery, Dankook University Jukjeon Dental Hospital (Yongin, Korea). Her chief complaint was a radiopaque mass (on right side of the maxilla), which induced intermittent discomfort and was discovered by her general dentist. A panoramic radiograph showed a radiopaque mass, circumscribed by a radiolucent halo underneath an impacted canine. Computed tomography (CT) scans revealed a hyperdense lesion, with its superior limits invading the floor of the nasal cavity and its posterior limits in the hard palate, and impacting the right maxillary canine above the lesion. It was decided that the odontoma and the impacted canine would be removed and replanted into the induced bony defect in a demineralized form for future dental implant in the canine site.(Fig. 1)
Before the operation, the patient received intravenous administration of clindamycin phosphate (injection 300 mg, Fullgram; Samjin Pharm., Seoul, Korea) and tramadol hydrochlorite (injection 50 mg, Tramadol HCl; Shinpoong Pharm., Seoul, Korea) under sedation (injection 5 mg, Midacum; Myungmoon Pharm., Seoul, Korea). After block and infiltration local anesthesia was performed with 2% lidocaine HCl (Xylestesin-A; 3M ESPE, Seoul, Korea), the odontoma and the impacted canine were surgically extracted. The extracted hard tissue was well-defined with intact adjacent cortical, which is highly suggestive of a benign lesion (odontoma). For an immediate graft, the patient was fully informed and consented that the diagnosis was being confirmed. The hard tissue was confirmed to be an odontoma after a week.
Before processing for graft material, all soft tissue around the root and pulp tissue in the root canals were removed with a surgical blade and a pear-shaped carbide bur. For the final step, many small holes were made on the exterior wall of the tooth to increase the surface contact with reagents.
The procedures, including demineralization, sterilization, and washing, followed the manufacturer's instructions using reagents (DecalSi DM; CosmoBioMedicare, Seoul, Korea) in an ultrasonic chamber (VacuaSonic; CosmoBioMedicare). Each reagent used for processing was kept in a sterile bioreactor tube with a 0.2 µm pore size polytetrafluoroethylene filter. The transfer of tissue between the reagent tubes was performed aseptically in a biological safety cabinet. The whole process took 2 hours.
After 2 hours, the patient was prepared for bone grafting. Additional local anesthesia with 2% lidocaine was administered. The bony defect was 2.7 (height)×1.0 (width)×1.8 (depth; anteroposterior) cm in size. The graft material was implanted in a block form.(Fig. 2. A, 2. B) A titanium sheet and microscrews (E3, CTi; NeoBiotech, Seoul, Korea) were used to maintain the graft in-situ.(Fig. 2. C, 3). Antibiotics and non-steroidal anti-inflammatory drugs were prescribed for 1 week and the patient was educated in postoperative dental hygiene. The operation was uneventful, the surgical site healed favorably, and no complications (infection, wound dehiscence, etc.) were noted after 1 week, or upon removal of the sutures.
Six months after the graft, a tissue core sample was taken from the center of the graft site during removal of the titanium sheet and prepared for decalcified histologic sections.
In this case, follow-up lasted only 6 months due to the patient's personal situation. During this limited period, no recurrence or delayed infection of the lesion were observed, and favorable new bone formation and subsequent resorption of the graft material were partly present in the radiograph. (Fig. 4) Histologically, some of the demineralized dentin matrix integrated strongly with the newly formed bone, and the graft material. Osteoblastic resorption of the graft tooth material and newly formed osteoid mixed with the tooth were observed at 6-months on cross sectional slides.(Fig. 5)
A 16-year-old Korean female was referred to the department by her orthodontist because of a radiopaque mass on the right side of the mandible. A panoramic radiograph showed a radiopaque mass (2.3×2.0×1.9 cm in size) in the left posterior mandible, distal to the second molar, which was circumscribed by a radiolucent halo beside the inferior alveolar nerve. CT scans revealed a hyperdense lesion, contacting above the bony canal of inferior alveolar nerve.(Fig. 6) It was diagnosed as a compound odontoma. Enucleation of the lesion, extraction of the right lower third molar and bone graft of the defect with the recycled hard tissues were planned for orthodontic reasons. The bony defect was 2.0 (height)×2.4 (width; anteroposterior)×1.2 (depth; buccolingual) cm in size. The overall procedures, including surgery, preparation of the tissue and grafting, were almost identical to those in Case 1.(Fig. 7) The wound was stabilized without any complications during the initial healing period, and orthodontic treatment was started one month after the surgery. At the 1-year follow-up, satisfactory bone regeneration of the defect was observed in panoramic radiograph and CT scans. Radiographically, the resorption of the demineralized autogenous odontoma and tooth graft was confirmed in conjunction with a newly formed alveolar bone, which showed higher bone density compared with the radiopacity of the donor site (an impacted 3rd molar on the right side).(Fig. 7) The patient is still under follow-up, and complete bone development and orthodontic treatment are expected.
The most common approach to treatment of an odontoma has been conservative surgical removal. Moreover, the probability of recurrence is very low if the tumor has been completely removed1,2,3. When a bone defect is found in the alveolar ridge, bone grafts are necessary to reconstruct the alveolar ridge and prepare the region for future implant surgery, or for further oral rehabilitation. The patients in the current study received bone grafts of the defects because of the need for further dental implants or for orthodontic reasons. An iliac bone graft is generally chosen for the surgery cavity of a large odontoma, however, it is usually not recommended in growing children because of donor site morbidities5,15. Although some authors report a low morbidity rate in iliac crest bone grafts compared with fibular flap grafts, donor-site dysfunctions and muscle contractures still exist15,16.
Our current report is likely to be the first human trial of recycled benign pathologic hard tissue as bone graft material utilized on the day of removal. The placement of a demineralized autogenous tooth bone graft after odontoma excision has the advantages associated with autogenous bone, such as osteogenesis, osteoinduction, and rapid healing time, without donor site morbidity. Follow-ups on these patients are extremely important to control alveolar ridge resorption and assess the graft site.
Even though use of a non-demineralized form of tooth powder showed good results in a few cases17, demineralization is an essential step for autogenous tooth bond graft materials that allows for an increase in bioavailability of matrix-associated noncollagenous proteins such as phosphophoryn, sialoprotein, glycoprotein, proteoglycan, osteopontin, osteocalcin, and dentin matrix protein-1. These proteins are involved in the bone resorption and mineralization processes6,17,18. Teeth are more highly mineralized and crystalized than bones, therefore, demineralization may be more important in tooth-based graft material. However, tooth demineralization is too time-consuming (usually two to six days) to be applied in clinic17. Another drawback of demineralization is that the long acid exposure negatively affects the noncollagenous proteins which trigger new bone formation19.
A modified ultrasonic technology with periodic negative pressure and temperature control has been introduced, and has dramatically reduced the time required for demineralization11. This technology improves the efficacy of ultrasound, and allows deep penetration of the cavitation energy of ultrasound and the reagents into the dentinal tubules14. The short duration of the whole process makes it possible to perform immediate demineralized autogenous tooth bone grafts chairside on the same day as the mass excision. In addition, this method allows the excised odontoma and tooth graft to be used immediately in a fresh state without the freeze dehydration usually performed for long-term preservation. Because freeze dehydration may affect the structure and physiochemical characteristics of collagen, the freshly demineralized autogenous tooth graft material is able to maintain the original collagen structure. Even though many researchers have reported that the collagen structure is crushed during the freeze dehydration process, the correlation between freeze dehydration and the ability of bone to regenerated needs further investigation20.
In conclusion, use of bone graft material prepared by recycled demineralization on the day of odontoma excision and tooth extraction would be convenient for both patients and clinicians. Within the limited cases in our study, recycled demineralized odontoma and impacted teeth prepared within two hours in an ultrasonic device worked well to restore alveolar bone defects after excision of an odontoma. During surgery, the block form of the graft can be easily changed to chips or powder, depending on the type of defect, thereby increasing clinical availability. We conclude that recycled demineralized odontoma and impacted teeth are favorable alternative treatments for the reconstruction of the alveolar ridge after the surgical removal of an odontoma.
References
1. Budnick SD. Compound and complex odontomas. Oral Surg Oral Med Oral Pathol. 1976; 42:501–506. PMID: 1067549.

2. Neville B, Damm DD, Allen CM, Bouquot J. Oral and maxillofacial pathology. Philadelphia: WB Saunders;2007.
3. Owens BM, Schuman NJ, Mincer HH, Turner JE, Oliver FM. Dental odontomas: a retrospective study of 104 cases. J Clin Pediatr Dent. 1997; 21:261–264. PMID: 9484137.
4. Mehra P, Singh H. Complex composite odontoma associated with impacted tooth: a case report. N Y State Dent J. 2007; 73:38–40. PMID: 17472184.
5. Louis PJ, Gutta R, Said-Al-Naief N, Bartolucci AA. Reconstruction of the maxilla and mandible with particulate bone graft and titanium mesh for implant placement. J Oral Maxillofac Surg. 2008; 66:235–245. PMID: 18201602.

6. Yeomans JD, Urist MR. Bone induction by decalcified dentine implanted into oral, osseous and muscle tissues. Arch Oral Biol. 1967; 12:999–1008. PMID: 4226721.

7. Kim YK, Kim SG, Byeon JH, Lee HJ, Um IU, Lim SC, et al. Development of a novel bone grafting material using autogenous teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:496–503. PMID: 20060336.

8. Murata M, Akazawa T, Takahata M, Ito M, Tazaki J, Hino J, et al. Bone induction of human tooth and bone crushed by newly developed automatic mill. J Ceramic Soc Jpn. 2010; 118:434–437.

9. Kim YK, Kim SG, Yun PY, Yeo IS, Jin SC, Oh JS, et al. Autogenous teeth used for bone grafting: a comparison with traditional grafting materials. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014; 117:e39–e45. PMID: 22939321.

10. Nanci A. Ten Cate's oral histology: development, structure and function. 8th ed. Mosby Elsevier;2008. p. 108–192.
11. Butler WT, Mikulski A, Urist MR, Bridges G, Uyeno S. Noncollagenous proteins of a rat dentin matrix possessing bone morphogenetic activity. J Dent Res. 1977; 56:228–232. PMID: 265954.

12. Liu Y, Luo D, Liu S, Fu Y, Kou X, Wang X, et al. Effect of nanostructure of mineralized collagen scaffolds on their physical properties and osteogenic potential. J Biomed Nanotechnol. 2014; 10:1049–1060. PMID: 24749399.

13. Beniash E. Biominerals--hierarchical nanocomposites: the example of bone. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2011; 3:47–69. PMID: 20827739.

14. Behrend O, Schubert H. Influence of hydrostatic pressure and gas content on continuous ultrasound emulsification. Ultrason Sonochem. 2001; 8:271–276. PMID: 11441610.

15. Fang QG, Shi S, Sun CF. Odontogenic lesions in pediatric patients. J Craniofac Surg. 2014; 25:e248–e251. PMID: 24785745.

16. Fasolis M, Boffano P, Ramieri G. Morbidity associated with anterior iliac crest bone graft. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 114:586–591. PMID: 22901642.

17. Atiya BK, Shanmuhasuntharam P, Huat S, Abdulrazzak S, Oon H. Liquid nitrogen-treated autogenous dentin as bone substitute: an experimental study in a rabbit model. Int J Oral Maxillofac Implants. 2014; 29:e165–e170. PMID: 24683581.

18. Rezende ML, Consolaro A, Sant'Ana AC, Damante CA, Greghi SL, Passanezi E. Demineralization of the contacting surfaces in autologous onlay bone grafts improves bone formation and bone consolidation. J Periodontol. 2014; 85:e121–e129. PMID: 24171500.

19. Suzuki S, Haruyama N, Nishimura F, Kulkarni AB. Dentin sialophosphoprotein and dentin matrix protein-1: two highly phosphorylated proteins in mineralized tissues. Arch Oral Biol. 2012; 57:1165–1175. PMID: 22534175.

20. Huang YF, Meek KM, Wang LQ, Wang DJ. Effects of prior freezing or drying on the swelling behaviour of the bovine cornea. Chin Med J (Engl). 2009; 122:212–218. PMID: 19187649.
Fig. 1
Preoperative panoramic radiopraph (A) and computed tomography (CT) scans (B, C) show compound odontoma associated with failure of permanent canine eruption. A. A odontoma is circumscribed by a radiolucent halo underneath an impacted canine (arrows). B. CT scans in axial section show that the alveolar bone was bulged to labial side slightly (arrows). C. CT scans in coronal section show an odontoma with its superior limits invading the floor of the nasal cavity and its posterior limits in the hard palate, and impacted the right maxillary canine above the lesion (arrows).

Fig. 2
Intraoral photos during operation. After opening the alveolar bony window (A), demineralized odontoma and tooth block were grafted followed by surgical removal (B), and titanium mesh filled with bone graft and secured into position with screws in the area of the bony defect (C). (a1: an impacted maxillary canine, a2: an odontoma, b1: demineralized odontoma and tooth block, asterisk: titanium mesh)
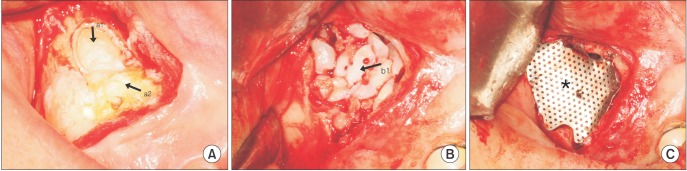
Fig. 3
Postoperative panoramic radiograph showing the titanium mesh in position with demineralized tooth graft materials.
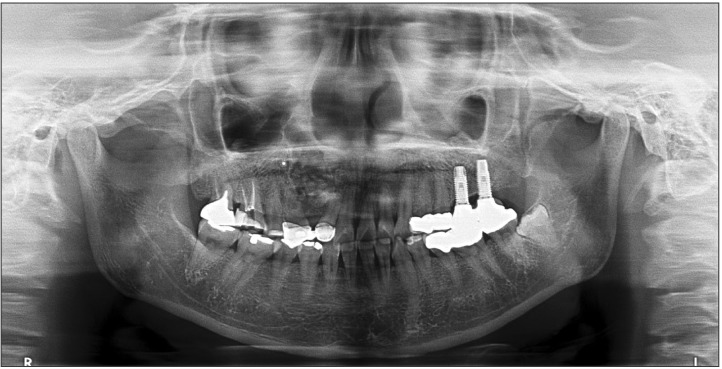
Fig. 4
Postoperative panoramic radiograph (A) and computed tomography scans in coronal (B), axial (C) section at 6-months follow-up shows favorable new bone formation and subsequent resorption of graft materials (arrows).
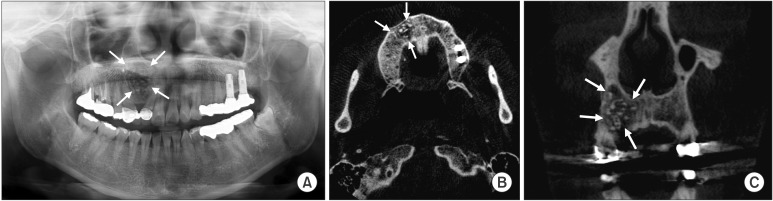
Fig. 5
The section in 6-months was stained with H&E staining (A: ×200, B: ×400) and Masson's trichorme staining (C: ×200, D: 400). Osteocytic embedding in graft tooth material (A, arrows), intimate fusion between new bone and graft tooth material (B, a-f) is observed. Osteocytic embedding in graft material with new bone were shown. Embedded osteocyte (C, c; D, a), newly formed bone (C, a,b,d; D, b) were also confirmed in the specimens.
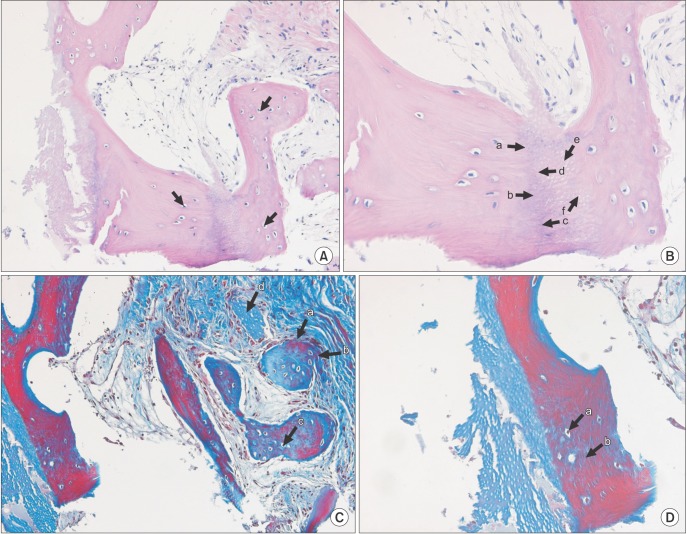
Fig. 6
Preoperative panoramic radiopgraph (A) and computed tomography scans (B, C) show a compound odontoma with impacted 3rd molar, contacting above the bony canal of inferior alveolar nerve (left, 4 arrows). Right impacted 3rd molar (right, 3 arrows) was also extracted for the orthodontic treatment.
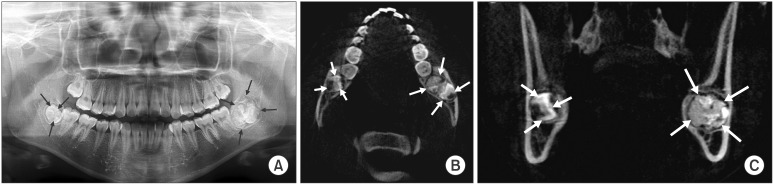
Fig. 7
Postoperative panoramic radiograph at postoperative 1-day (A), and 1-year (B), computed tomography scans (C, D) at 1-year follow-up. Radiographs at 6-months (B-D) showed favorable new bone formation, regularity of alveolar ridge, and higher bony density of graft site. Patient could start orthodontic treatment after 1 month of mass excision. Left: 4 arrows, right: 3 arrows.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download