Abstract
In surgery for facial asymmetry, mandibles can be classified into two types, rotational and translational, according to the required mandibular movements for surgery. During surgery for rotational mandibular asymmetry, a bilateral sagittal split ramus osteotomy (BSSRO) may cause a large bone gap between the proximal and distal segments as well as condylar displacement, resulting in a relapse of the temporomandibular joint disorder, especially in severe cases. The intraoral vertical ramus osteotomy has an advantage, in this respect, because it causes less rotational displacement of the proximal segment on the deviated side and even displaced or rotated condylar segments may return to their original physiologic position. Unilateral intraoral vertical ramus osteotomy (UIVRO) on the short side combined with contralateral SSRO was devised as an alternative technique to resolve the spatial problems caused by conventional SSRO in cases of severe rotational asymmetry. A series of three cases were treated with the previously suggested protocol and the follow-up period was analyzed. In serial cases, UIVRO combined with contralateral SSRO may avoid mediolateral flaring of the bone segments and condylar dislocation, and result in improved condition of the temporomandibular joint. UIVRO combined with contralateral SSRO is expected to be a useful technique for the treatment of rotational mandibular asymmetry.
Bilateral sagittal split ramus osteotomy (BSSRO) has most frequently been used to treat various dentofacial deformities. It has the advantage of early jaw movement by utilizing a rigid fixation method. However, in cases of moderate to severe asymmetry, when the mandibular midline is rotated laterally, flaring of the proximal segment on the short side can occur and results in a gap between the fragments. Displacement of the condyles within the mandibular fossa can occur when the proximal and distal segments are not passively positioned during the application of internal fixation devices. This condylar displacement may cause skeletal or occlusal instability and temporomandibular joint (TMJ) dysfunction1,2,3,4.
Careful bone removal can be performed to minimize or eliminate bony interference between the proximal and distal segments, but it is not always possible to eliminate enough bone for sufficient bony contact due to structural limitations1.
Recently, additional vertical osteotomy of the distal segment, just behind the terminal molar, was proposed to passively align the proximal segment and distal segment and eliminate all bony interference, even in cases of severe asymmetry2,3. No medial force has to be applied to the proximal fragment to align the segments after interference between the fragments has been eliminated with the secondary osteotomy3.
Another modification of sagittal split ramus osteotomy (SSRO) is described as follows. On the long side, a conventional osteotomy is performed. On the short side, unlike a usual lingual osteotomy made horizontally above the lingual osteotomy, the osteotomy was angled downward and the buccal osteotomy was made horizontally below the lingual osteotomy. The angulation of the lingual osteotomy made the posterior aspect of the distal segment shorter, thereby preventing bony interference of the two segments during fixation4.
The authors used a unilateral intraoral vertical ramus osteotomy (UIVRO) on the short side combined with a contralateral SSRO to overcome the condylar displacement and its sequelae in asymmetric cases, especially in cases of rotational mandibular asymmetry.
All patients were explained for the use of clinical images on this article and informed consent was gained.
An 18-year-old male visited our hospital with a chief complaint of right chin deviation. The patient received presurgical orthodontic treatment for one year. He suffered from atopic dermatitis and allergic rhinitis. Through clinical evaluation, concordant canting of the maxillary, mandibular occlusal plane, and chin were observed. Yawing of the maxillary arch was also present. Dental midline discrepancy between the upper and lower incisors was present. TMJ dysfunctions including pain and noise on both TMJs were present. Cephalometric analysis of the patient revealed that the menton (Me) of the mandible was deviated 6.5 mm to the right and the left maxilla was positioned 3.5 mm downward at the upper canine position compared to the right.(Fig. 1)
Through cephalometric tracing and model surgery, we determined the amount and direction of maxillary and mandibular movements. In the mandible, the chin midline should be rotated to the left and the amount of setback was estimated to be 1 mm on the short side (the right side) and 6.5 mm on the long side (the left side). Bony interference between the fragments and flaring of the proximal segment on the right side would be anticipated if a BSSRO was performed. Therefore, we planned to use UIVRO on the short side and SSRO on the contralateral side of the mandible.
During the maxillary surgery, a Le Fort I osteotomy was performed to correct the canting and yawing of the maxilla in a standard fashion based on the intermediate surgical wafer. In the mandible, conventional SSRO was begun on the long side of the mandible (the left side) and then IVRO was performed on the short side (the right side).
On the left side a SSRO was performed, when the osteotomized distal segment was positioned using the final surgical wafer and the condyle was repositioned within the glenoid fossa without compression, initial bone contact occurred anteriorly and a large gap was noted posteriorly between the segments. A 2.0 mm monocortical miniplate was placed first and then two bicortical position screws were placed to prevent condylar torque. In the IVRO, an oblique osteotomy from the sigmoid notch to the inferior border of the mandibular angle and coronoidotomy were performed. During the IVRO procedure, no bony interference between the segments was seen. We did not perform repositioning or fixation of the condylar and proximal segments on the short side of the IVRO side. Additionally we did genioplasty for vertical reduction and advancement of the chin.(Fig. 2)
Intermaxillary wire fixations were maintained postoperatively for two weeks with the final surgical wafer to stabilize the occlusion and mandibular segments. After release of intermaxillary fixation at two weeks, two elastic bands were used for mouth opening exercises. The wafer was maintained for 6 weeks postoperatively for training and adaptation to the new anatomical circumstances. Postoperative orthodontic treatment was completed 6 months after surgery. The dental midline discrepancy, canting of the occlusal plane, and chin deviation were significantly improved and the temporomandibular symptoms including pain or tenderness over the TMJ and joint noise were significantly decreased.(Fig. 3)
A 24-year-old male visited our clinic with a chief complaint of chin deviation. The patient previously received presurgical orthodontic treatment at a private clinic for a total of 10 months. He had a medical history of a prior pneumothorax and hepatitis. Clinically, the chin of the patient was deviated to the left side and canting of the rima oris was observed. The right maxilla was down 3.5 mm at the upper canine position compared to the left and the maxillary arch and upper dental midline were rotated to the left. The lower dental midline of the incisors was deviated 4.0 mm to the left side. The overjet and overbite was -3.0 mm and 3.5 mm, respectively. No specific symptoms and findings on the TMJ were noted.(Fig. 4)
Through presurgical planning, we determined the amount and direction of maxillary and mandibular movements. Maxillary canting and yawing deformities was corrected only with a Le Fort I osteotomy. A sagittal ramus osteotomy with a 11.5 mm setback was begun on the right side of the mandible. One 2.0 mm monocortical miniplate and two bicortical positional screws were used for internal fixation of the SSRO. On the short-left side (deviated side), a IVRO of 6.0 mm setback and coronoidotomy were performed. During the IVRO procedure, we determined that the distal segment was excessively rotated and positioned laterally to the condylar segment. No fixation device for the IVRO was used. Next, postoperative procedures proceeded in the same way as in the previous case.(Fig. 5)
On postoperative radiographs and cone-beam computed tomography, we found that the most posterior aspect of the distal segment on the left side (deviated side; IVRO performed) was rotated laterally on a large scale and positioned lateral to the proximal segment.(Fig. 6) During the follow-up period, temporary paresthesia over the left side of the lower lip and chin was observed; however, the sensory disturbances improved 3 months after surgery and completely disappeared at the sixth postoperative month. Additionally, the patient showed a normal range of mouth opening and did not complain of any other TMJ symptoms.(Fig. 7)
A 19-year-old female was referred from the department of orthodontics for orthognathic surgery. She wanted to improve her facial appearance of chin protrusion and also complained of pain and noise from the left TMJ. Vertical and anteroposterior position of the maxilla was acceptable and occlusal canting or yawing of maxilla was not identified. The lower dental midline of the incisors was deviated 3 mm to the left side compared with the upper dental midline and the overjet was -2.0 mm.(Fig. 8)
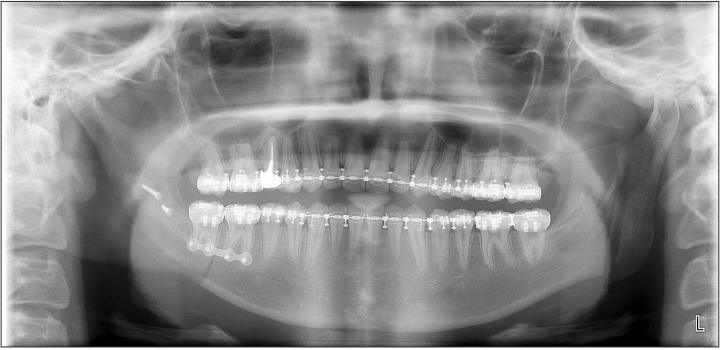
We decided to perform only mandibular surgery and the estimated amount of setback was 7.0 mm on the long side (right side) and 3.0 mm on the short (left side). We did not anticipate considerable bony interference or a gap between the fragments during the BSSRO. However, she consistently complained of TMJ symptoms, so we chose to perform a UIVRO on the deviated side rather than BSSRO. The SSRO was started on the right and left sides and a IVRO setback was performed with a coronoidotomy. During the IVRO procedure, we found lateral flaring of the proximal segment so minimal bony removal at the inner surface of the proximal condylar segment was performed to minimize bony interference between the segments.(Fig. 9) Operative and postoperative procedures were similar to the cases presented previously. Postsurgical orthodontic treatment was completed at 6 months. At postoperative 6 months, the occlusion was stable and an excellent facial appearance was achieved. Joint noise was detected on her left TMJ with wide mouth opening, but she has not reported any painful episodes with mouth opening or mastication.(Fig. 10)
BSSRO is a versatile and reliable surgical technique for the correction of prognathic or retrognathic patients. Rigid internal fixation is routinely used to stabilize the proximal and distal segments following SSRO, for fast bone healing, initiating early postoperative jaw function, and decreasing the amount of relapse. Without intermaxillary fixation, postoperative airway management is much easier and the convenience of oral hygiene maintenance is an additional advantage of SSRO.
The author suggests that in orthognathic surgery for asymmetric mandibles, mandibular movements required to achieve an appropriate occlusal relationship to the maxilla can be classified into two types according to the subtype of mandibular asymmetry; rotational or translational5.
In surgical treatment for rotational mandibular asymmetry, when the mandibular midline is shifted laterally, the most posterior aspect of the distal segment is rotated medially and the other side is rotated laterally. This causes gaps between the fragments when performing a BSSRO. Displacement of the condyles medially or laterally within the mandibular fossa can occur when the proximal and distal segments are not passively positioned during the application of internal fixation devices3. This condylar displacement can cause malocclusion associated with the risk of early relapse and favor the development of temporomandibular disorders1,2,3,4,6,7,8,9.
To avoid flaring of the mandibular segments, several modifications or additional procedures for SSRO were advocated. The simplest method among the procedures was removal of the bony interferences between the segments to minimize flaring of the proximal segment. Careful bone removal prevents displacement of the proximal segment and possible condylar torque after distal segment repositioning. Furthermore, it maximizes the area of bone contact along the sagittal osteotomy. However, because of the neuromuscular bundle and other anatomical limitations, removing sufficient bone to remove all bony interferences between the segments is not possible in many cases1.
Modifications of SSRO have been implemented to improve the efficiency and predictability of the split, increase bony overlap to improve union, and maintain condylar position. Ellis3 proposed that the additional osteotomy of the distal segment behind the last molar had several benefits including elimination of all premature contact areas and bony interferences. This secondary osteotomy might cause less displacement of the mandibular condyle; however, the main disadvantage of the secondary osteotomy is that the nerve may undergo a second surgical insult when the greenstick fracture occurs or potentially during instrumentation. Yoshida et al.4 suggested a modified SSRO designed to minimize displacement of the proximal segment in asymmetric cases. Usually, a lingual osteotomy is made horizontally above the lingula, but in their cases, because the distal segment on the short side needed to be shifted more than 5 mm, the osteotomy was angled downward and the buccal osteotomy was made horizontally below the lingual osteotomy rather than in the region of the mandibular body. This procedure prevented overlap of the two segments during fixation. Through this procedure, they avoided displacement of the proximal segment. However, because the area of bone contact produced by this procedure is narrow, it may result in nonunion between the proximal and distal segments.
In comparison with SSRO, there are fewer bony contact areas between the segments during the IVRO procedure. Furthermore, it does not require rigid fixation and allows for postoperative positional changes of rotated or displaced condylar segments. Bell and colleagues10,11 reported that the condyle was positioned anteriorly and inferiorly after IVRO but the condyles tended to return to their preoperative position after systemic neuromuscular rehabilitation12. Jung et al.13 also reported that lateral rotation of the condyles occurred after IVRO setback and the laterally rotated condylar angles progressively reversed towards the original angulations. Therefore, IVRO causes less rotational displacement of the proximal segment on the deviated side during the surgical procedure and displaced or rotated condylar segments returned to a physiologic position. Therefore, this technique may bring stable postoperative results without condylar displacement and adverse sequelae when surgically correcting mandibular asymmetry.
After IVRO, postoperative disappearance of signs and symptoms of TMJ disorders has been reported13,14,15. The improvements of symptoms associated with TMJ disorders after IVRO was contingent on producing a more functional articular disc-condylar relationship and decreased pressure between the mandibular condyle and mandibular fossa11,16. Lai et al.17 reported a high incidence of TMJ disorders in patients with mandibular asymmetries. He also endorsed that UIVRO and SSRO can be useful in improving signs and symptoms of TMJ disorders as well as correcting mandibular deviation. This was also shown in our cases.
In our patients with rotational mandibular asymmetry, UIVRO combined with contralateral SSRO was effective in correcting mandibular asymmetry, because it helped avoid mediolateral flaring of the bone segments and condylar dislocation of the deviated side. Additionally, the signs and symptoms of TMJ disorders on the deviated side were improved. Through this experience, we recommend UIVRO combined with contralateral SSRO as a useful technique for the treatment of rotational mandibular asymmetry.
References
1. Schwartz HC. Efficient surgical management of mandibular asymmetry. J Oral Maxillofac Surg. 2011; 69:645–654. PMID: 20934795.

2. Epker BN, Stella JP, Fish LC. Dentofacial deformities, integrated orthodontic and surgical correction. 2nd ed. St. Louis: Mosby;1999.
3. Ellis E 3rd. A method to passively align the sagittal ramus osteotomy segments. J Oral Maxillofac Surg. 2007; 65:2125–2130. PMID: 17884553.

4. Yoshida K, Rivera RS, Kaneko M, Kurita K. Minimizing displacement of the proximal segment after bilateral sagittal split ramus osteotomy in asymmetric cases. J Oral Maxillofac Surg. 2001; 59:15–18. PMID: 11152184.

5. Jeon JH. Surgical treatment planning for the two subtypes of mandibular asymmetry. J Korean Assoc Oral Maxillofac Surg. 2014; 40:205. PMID: 25368831.

6. Ellis E 3rd, Hinton RJ. Histologic examination of the temporomandibular joint after mandibular advancement with and without rigid fixation: an experimental investigation in adult Macaca mulatta. J Oral Maxillofac Surg. 1991; 49:1316–1327. PMID: 1955923.

7. Ueki K, Degerliyurt K, Hashiba Y, Marukawa K, Nakagawa K, Yamamoto E. Horizontal changes in the condylar head after sagittal split ramus osteotomy with bent plate fixation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:656–661. PMID: 18602292.

8. Ellis E 3rd. Condylar positioning devices for orthognathic surgery: are they necessary? J Oral Maxillofac Surg. 1994; 52:536–552. PMID: 8189289.

9. Costa F, Robiony M, Toro C, Sembronio S, Polini F, Politi M. Condylar positioning devices for orthognathic surgery: a literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:179–190. PMID: 18417381.

10. Bell WH, Yamaguchi Y, Poor MR. Treatment of temporomandibular joint dysfunction by intraoral vertical ramus osteotomy. Int J Adult Orthodon Orthognath Surg. 1990; 5:9–27. PMID: 2373914.
11. Bell WH, Yamaguchi Y. Condyle position and mobility before and after intraoral vertical ramus osteotomies and neuromuscular rehabilitation. Int J Adult Orthodon Orthognath Surg. 1991; 6:97–104. PMID: 1811034.
12. Choi YS, Jung HD, Kim SY, Park HS, Jung YS. Remodelling pattern of the ramus on submentovertex cephalographs after intraoral vertical ramus osteotomy. Br J Oral Maxillofac Surg. 2013; 51:e259–e262. PMID: 24070895.

13. Jung HD, Jung YS, Park HS. The chronologic prevalence of temporomandibular joint disorders associated with bilateral intraoral vertical ramus osteotomy. J Oral Maxillofac Surg. 2009; 67:797–803. PMID: 19304037.

14. Hall HD, Navarro EZ, Gibbs SJ. Prospective study of modified condylotomy for treatment of nonreducing disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 89:147–158. PMID: 10673649.

15. Hall HD, Navarro EZ, Gibbs SJ. One- and three-year prospective outcome study of modified condylotomy for treatment of reducing disc displacement. J Oral Maxillofac Surg. 2000; 58:7–17. PMID: 10632159.

16. Ueki K, Marukawa K, Shimada M, Yoshida K, Hashiba Y, Shimizu C, et al. Condylar and disc positions after intraoral vertical ramus osteotomy with and without a Le Fort I osteotomy. Int J Oral Maxillofac Surg. 2007; 36:207–213. PMID: 17239565.

17. Lai W, Yamada K, Hanada K, Ali IM, Takagi R, Kobayashi T, et al. Postoperative mandibular stability after orthognathic surgery in patients with mandibular protrusion and mandibular deviation. Int J Adult Orthodon Orthognath Surg. 2002; 17:13–22. PMID: 11934051.
Fig. 1
Preoperative facial photograph (A) and cephalometric radiographs (B) (case 1). The patient was explained for the use of clinical images on this article and informed consent was gained.
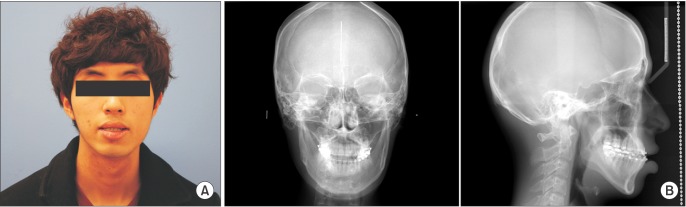
Fig. 2
Postoperative panoramic radiograph 6 weeks after surgery; intraoral vertical ramus osteotomy and coronoidotomy on the right mandible and sagittal split ramus osteotomy on the left with a miniplate and positional screw fixation.
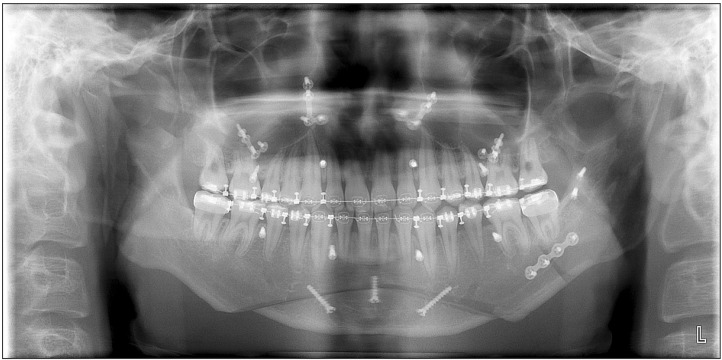
Fig. 3
Facial photograph (A) and cephalometric posterior-anterior radiograph (B) 6 months after surgery. The patient was explained for the use of clinical images on this article and informed consent was gained.
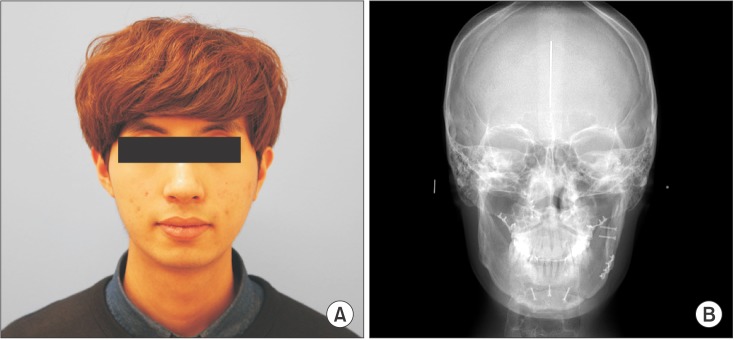
Fig. 4
Preoperative facial photograph (A) and cephalometric radiographs (B) (case 2). The patient was explained for the use of clinical images on this article and informed consent was gained.
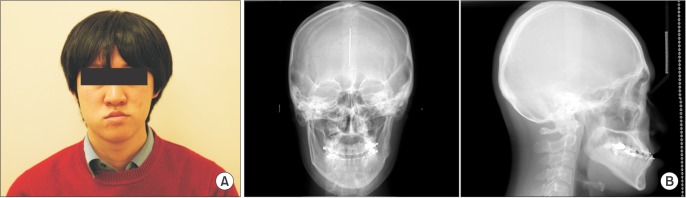
Fig. 5
Postoperative panoramic radiograph 6 weeks after surgery; intraoral vertical ramus osteotomy and coronoidotomy on the left mandible and sagittal split ramus osteotomy on the right with miniplate and positional screw fixation.
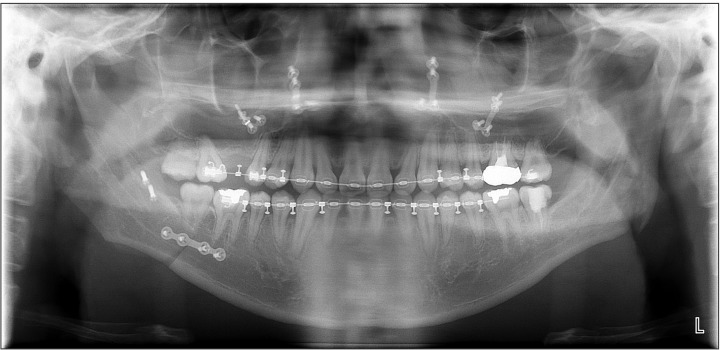
Fig. 6
Postoperative cone-beam computed tomography images. A. Postoperative 6 week; the most posterior aspect of the distal segment on the left intraoral vertical ramus osteotomy side was positioned lateral to the proximal segment rather than medially. B. Postoperative 1 year; bony union between the segments on the left as well as the right side can be seen.
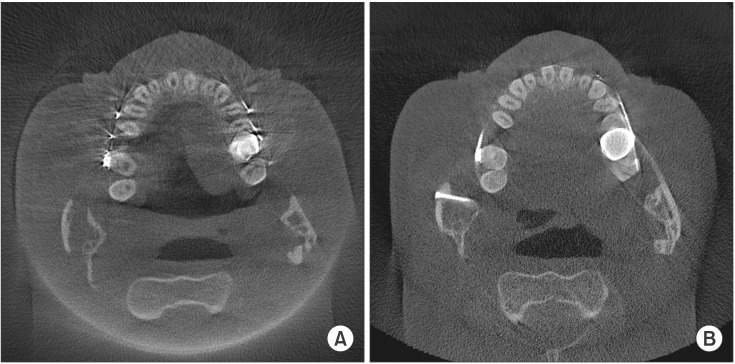
Fig. 7
Facial photograph (A) and cephalometric posterior-anterior radiograph (B) 18 months after surgery. The patient was explained for the use of clinical images on this article and informed consent was gained.

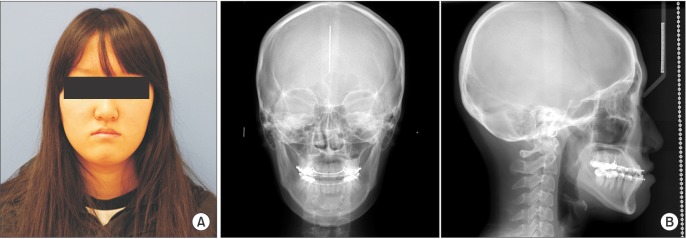
Fig. 8
Preoperative facial photograph (A) and cephalometric radiographs (B) (case 3). The patient was explained for the use of clinical images on this article and informed consent was gained.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download